News 12/9/16
Top News

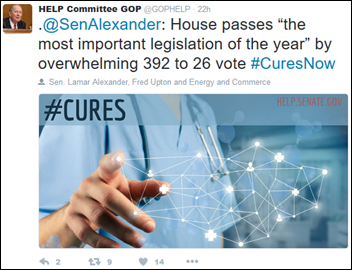
The Senate passes the 21st Century Cures Act in a 94 to 5 vote, sending it to the President’s desk for signature. The President praised the $6.3 billion legislation Wednesday and confirmed that he would sign it. Sen. Lamar Alexander (R-TN), chairman of the Senate health committee and one of the most ardent proponents of the bill, was understandably excited given that it has been circulating for two years and is considered to be one of most heavily lobbied pieces of legislation in recent memory. It provides money for cancer research; funds mental health treatment and resources to combat the opioid abuse epidemic; helps the FDA speed up drug approvals; and bolsters healthcare technology goals related to interoperability, privacy, and security.
HIStalk Announcements and Requests
This week on HIStalk Practice: Arianna Huffington includes Doctor on Demand in new wellness venture. Banner Urgent Care goes with RCM services from Zotec Partners. Health apps found sorely lacking in privacy precautions and safety standards. Marathon Health upgrades its EHR for workplace health centers. Montana preps for statewide HIE. PPJ Healthcare Enterprises raises $5 million.
Webinars
December 14 (Wednesday) noon ET. “Three Practices to Minimize Drift Between Audits.” Sponsored by Armor. Presenter: Kurt Hagerman, CISO, Armor. Security and compliance readiness fall to the bottom of the priority lists of many organizations, where they are often treated as periodic events rather than ongoing processes. How can they improve their processes to ensure they remain secure and compliant between audits? This webinar will cover the healthcare threat landscape and provide three practices that healthcare organizations can implement to better defend their environments continuously.
Acquisitions, Funding, Business, and Stock
Google Ventures founder Bill Maris raises a $230 million venture fund dubbed Section 32 (a likely homage to Star Trek’s Section 31 security operation) that will focus on healthcare investments. Maris, who left Google earlier this year, plans to run the fund solo from San Diego rather than Silicon Valley.
![]()
Augmedix closes a $23 million round of funding led by new investors McKesson Ventures and OrbiMed. It has raised over $60 million since launching its Google Glass-powered remote scribing service in 2012. Jenn talked with CEO and co-founder Ian Shakil about the company’s plans to move beyond its core services in “Value-based Care Prompts Glass to Grow Up.”

Brentwood, TN-based consulting and staffing firm Vaco merges the newly acquired Pivot Point Consulting and Greythorn – both based in Washington – to form Pivot Point Consulting, a Vaco company. The new subsidiary brings together 50 employees and combines Pivot Point’s EHR implementation and advisory services with Greythorn’s recruitment expertise.

The patent case over CRISPR-cas9 technology, likely the most valuable patent in biotechnology, begins as the University of California argues to have MIT and Harvard’s patent invalidated and transferred to UC. The patent office awarded The Broad Institute of MIT and Harvard its first CRISPR patient in April 2014, during which time it was reviewing UC’s patient, filed in May 2012.

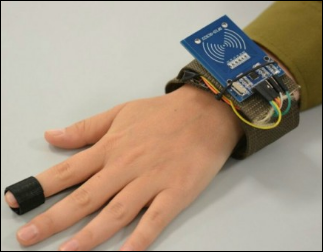
After much speculation, Fitbit buys Pebble’s software assets for an undisclosed sum, though Bloomberg has valued the transaction at less than $40 million. Pebble, which launched via a crowdfunding campaign in 2012, will no longer produce or sell its smartwatches.
Looking to further bolster its diminishing wearables market share, Fitbit also will work with Medtronic to add glucose monitoring to its fitness trackers. Type 2 diabetes patients will be able to combine their Fitbit-generated data with Medtronic’s IPro2 Continuous Glucose Monitoring system, which can send pertinent data to a patient’s provider.
People

Juliana Hart (Verscend Technologies) joins MedCPU as vice president of market development.

Brooke Patterson (FEI Systems) joins health IT and management consulting firm ARDX as SVP of government services.


Cricket Health appoints University of California-San Francisco nephrologists Carmen Peralta, MD chair of its medical advisory board, and Anna Malkina, MD medical director.
Announcements and Implementations

Chicago-based Union Health Service implements RadNet’s RIS, speech recognition, and mammography tracking.
Nemours Children’s Hospital, Seven Rivers Regional Medical Center, and Westchester General Hospital sign up for the Florida HIE’s event notification service, which patient hospital encounter notifications to participating ACOs, physicians, and payers.
Technology
SecureDx.net develops Secure Data Exchange messaging technology featuring two-factor authentication.
Sales

Looking to set up a private HIE, Chicago-based Rush Health chooses HealthShare interoperability technology from InterSystems.

Schleicher County Medical Center and Nursing Home (TX) taps CPSI subsidiary American HealthTech to help it implement technology upgrades to its clinical and business management operations. The company will also provide Medicaid AR management services.
TaraVista Behavioral Health Center (MA) signs on for MedSphere’s OpenVista EHR. The inpatient facility will also utilize the company’s Phoenix Health Systems division for IT support.
Government and Politics

The FBI indicts 21 employees from Forest Park Medical Center (TX), claiming that they paid $40 million in bribes and kickbacks in exchange for referrals to its purely out-of-network health system. Those indicted include owners Alan Beauchamp, Richard Toussaint Jr., Wade Barker, and Wilton Burt; and Jackson Jacob and Andrea Smith, both of whom set up separate shell companies to funnel bribe and kickback payments to surgeons in exchange for the referrals.
The DoD taps Medical Information Network – North Sound to develop and maintain an HIE-like portal that will be accessible in any clinic or hospital within the DoD system. Integration with the department’s new Cerner-built EHR, currently in pilot phase at several bases in Washington, is expected.

The House passes the telemedicine-friendly Expanding Capacity for Health Outcomes (ECHO) Act, which now heads to the president’s desk after receiving unanimous Senate approval last week. Once signed into law, the act will set in motion an HHS study on the feasibility of training providers to expand technology-enabled healthcare delivery in underserved areas.
Research and Innovation
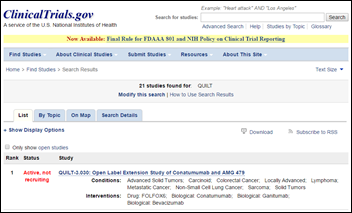
NantHealth makes its Quantum Immuno-oncology Lifelong Trial (QUILT) Programs available via ClinicalTrials.gov. CEO Patrick Soon-Shiong, MD believes making the QUILT trials available through the NIH registry will improve patient access to active and future immunotherapy-based trials for a variety of cancers.
Other
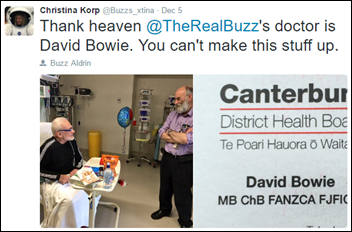
Quite a space oddity: David Bowie treats former astronaut Buzz Aldrin in a New Zealand hospital after Aldrin was rescued from the South Pole after falling ill. The 86 year-old was part of a tourist group that was visiting the Amundsen-Scott South Pole Station through December 12.
Sponsor Updates
- Imprivata will exhibit at the CIO Forum December 8 in Yorba Linda, CA.
- Ingenious Med receives the Emerging Company of the Year Phoenix Award from the Metro Atlanta Chamber.
- Database Trends and Applications Magazine names InterSystems Cache a trend-setting product in data and information management for 2017.
- Kyruus will present at the Carolina Healthcare Public Relations & Marketing Society meeting December 9 in Charleston, SC.
- Liaison Healthcare expands its relationship with London-based reseller partner AK Loman.
- LifeImage releases video insights from RSNA 2016.
- Gartner includes LiveProcess as a representative vendor in its 2016 market guide for clinical communication and collaboration.
- Meditech shares a brief case study featuring Anderson Regional Medical Center (MS).
- Netsmart will exhibit at the Community Behavioral Healthcare Association of Illinois Conference December 12 in Schaumburg.
- Computerworld names NTT Data VP of Digital Experience Lisa Woodley a 2017 Premier 100 Technology Leader.
- Black Book ranks Nuance first in CDI for the third consecutive year, and first for end-to-end coding, CDO, transcription, and speech-recognition technology.
- Health Catalyst receives the 2017 Glassdoor Employee Choice Award.
- Rock Health names Health Catalyst CEO Dan Burton the winner of its annual Most Beloved CEO award for 2017.
- Verscend Technologies publishes a new white paper, “The Evolution of DxCG, the Gold Standard in Risk Adjustment and Predictive Modeling.”
Blog Posts
- Your Breach Response Team May Not Matter … Until it Does (ID Experts)
- Top 5 Success Strategies for Integration Projects (Impact Advisors)
- Prepare Your Hospital’s 2017 Digital Marketing Strategy (Influence Health)
- The Pollsters Were Wrong: What are the Big Data Implications? (Liaison Healthcare)
- Telling Your Front-Office Team, “I’ve Got Your Back!”: Tips for Maximizing Patient Payment Revenue (Navicure)
- Printing Healthcare’s Bright Future, in 3D (Orion Health)
- CHIME 2016 Fall CIO Forum underscores increasing financial pressures in healthcare; need for better analytics (Infor Healthcare)
- Innovations in Encrypted Paging Protect PHI (Spok)
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates. Send news or rumors.
Contact us.

















































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…