HIStalk Interviews Jim Higgins, CEO, Solutionreach
Jim Higgins is founder and CEO of Solutionreach of Lehi, UT.

Tell me about yourself and the company.
I started Solutionreach in the year 2000. For me, it was about changing the relationship between the provider and the patient.
I’ve got a daughter with an autoimmune disease, so my wife and I have seen a lot of specialists over the course of the last 12 years. We’ve had a lot of questions after leaving appointments with confused faces, feelings, and thoughts and not being able to reach those providers in an easy manner. It’s just very, very difficult feeling disconnected and on a patient island. That’s what we’re trying to do at our company. That’s why I’m here doing what I’m doing.
I’ve been here 16 years. It’s gone by fast. I’ve been in technology for a long time and I’m excited about focusing my efforts in a way that’s very personal to me and making a difference overall, versus just pounding away at great technology solutions that are not really making an impact on the lives of people in a way that I think need to happen.
What technologies work best for physician practices that are interested in improving or expanding their patient relationships?
Anything that extends the accessibility of two-way communication between patients and the practice. There’s just too much stuff going on right now. There’s too much change, too many questions. There’s a lot of information out there, which is a good thing, but that breeds questions.
For instance, patients going into self-diagnosis mode — which we all tend to do at times, because there’s so much information, which is fantastic and I love that — puts practices and physicians in a spot. They have to unwind a little bit what we as patients perceive we may have. Then we may already be down a path of diagnosis as we’re coming in, and then just the care that’s associated with that. We need that guidance from our physician to say, "You’re going to read a lot of things. You’re going to see a lot of things. This is what I really want you to stick to."
That’s the most important thing that we can do for our health. Any kind of tools or technology that you can put in place to extend that kind of communication in a very simple and effective manner.
There’s a lot of technologies out there that are not very simple and effective, meaning they don’t match up with patients in terms of the consumer and what we actually do on a daily basis. It’s one thing to think about logging into a portal, but I might be five clicks away from a simple message. I might not get that response for days.
Those types of things don’t stand the test of time. We’re in a society where our expectations are very different now, where we expect to have information quickly and accurately. Accessibility needs to be there, not only from a velocity perspective, but ease of use. We’re out and about and trying to think about, "I’ve got to get to my doctor," and somehow do that in a way that it doesn’t really fit into our lifestyles, one where you’re going to have limited communication. Limited communication leads to fewer questions, and overall, leads to worse outcomes for patients.
Hospitals and practices are set up under the Jiffy Lube model, where they don’t want to get to know you – you just show up, get work done, and leave until next time. Calling them up sends you to a phone tree and maybe they’ll return your call or maybe they won’t. It’s hard to get in touch after business hours that may not be convenient. Does the motivation exist to change that to make patients feel more valued as individuals?
Well stated. That’s exactly what’s happening. I’ve been in a lot of different industries with technology and it’s amazing the amount of information and the service levels that we can provide. Just think about the financial industry. It’s crazy. I can be in Europe walking down the street, see an ATM, put my card in, and in seconds I can get cash out. It recognizes who I am, where my home location is, what bank I use, and all that stuff routes in seconds. It’s amazing that we go into healthcare, we check in, and someone doesn’t even know what’s going on with us.
In other industries, any company might be thinking about their customers. They know their customers, they stratify their customer base, they have a CRM program. You have to have at least that to even start a business nowadays. Then they have targeted marketing. All these things where you’re saying, I know my customer, I know what predictive models say they’re going to buy. For instance, on Amazon.
We see that with technology and we expect that now. We expect that, "I bought this. The next five things I’ll likely buy would be these. I want to get information." The knowledge that companies have about us makes the experience better, whether it’s shopping, e-commerce, or finance.
It should be that way in healthcare, but the PCP is just trying to stay above water. They’re giving great care when you’re with them and they’re engaging you on a face-to-face basis. Of the many PCP customers we have, they talk about, "I do my very best and I care about my patients." We say, absolutely.
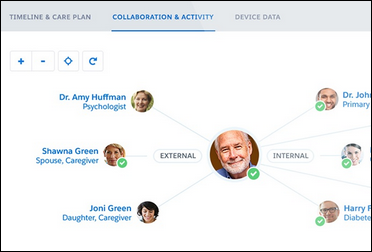
The issue is, they don’t really know what their patient base looks like. They don’t have a feeling for, how many chronic care conditions do you have? How many patients have multiple? Which ones are those? What do you do about them? How are you trying to motivate your patients? How are you trying to communicate with your patients, based on what they have and then their history of all this information and data that you already have in your system, and then more data that you can utilize with technology? That’s a critical part of what’s happening, where people don’t know who you are.
The other point I would make is that a customer of ours said, I’m there at eight o’clock. I’m trying to leave at six o’clock. I see a ton of patients, I’m doing my very best. I care, but I have a family. I try to have a semblance of a life, but I have 60+ calls waiting for me after six o’clock. It will take everything from me. There’s no way I can be there around the clock all the time. There’s no way I can really get back to those people.
Those are things that stack up — the questions that are asked. If you can be proactive and if you can have a system that helps you scale the care you’re providing, that’s what everyone’s looking for. Technology can do that in a personalized way.
In both clinical care and IT, the recipient of services usually likes and respects the person they worked with, but their satisfaction may tinged by other factors, such as how long it took to be seen, how polite the first-level people were, and how friendly the end result was, like a patient bill or a service call summary. Do you wonder how much patient satisfaction is driven by the red tape we wrap around the clinical encounter and not something the clinician themselves can influence?
No question. When I started the company, I said, there’s the concept of Doc Mayberry coming down the country lane with a medical bag and caring a lot. Doc Mayberry, you can always see him and he knows you from cradle to grave. He has taken care of you and your family for generations. That personal relationship is so strong and so important.
Yet you’re right — we have gotten away from that. The bureaucracy has played a part. In patient relationship management, our cause is to use technology in a personalized way in such that you return to Mayberry a little bit.
That personal relationship is critical. I can tell you in my experience with my daughter, it’s very critical in terms of the relationships that we have. That contact that we get, that trust, and that history that we understand, versus somebody just coming in and we see somebody different every time. Even though they pull the EMR and see the records, “OK, I see that this has happened in the past," for us, that doesn’t work. It just doesn’t. We don’t want to explain our story over again, and then afterwards, we feel like we’re on our own. That’s not a good place to be.
Patient self-scheduling seems like it should be universal since it offers benefits to both patient and practice, yet I don’t see much of it. What’s holding back its use?
The challenge with self-scheduling is the integration into the EMR. EMRs with scheduling systems don’t do a great job at connecting with the patients on a personalized, one-on-one basis. Other companies fill that gap. They build really beautiful software and great workflows, make it simple, and outreach to the patient in the right context so the patient understands why they need to book an appointment. Not just to have it out there, but the fact that, "Oh, I really do need to come in." Outreach has happened — the invitation to come back in because their condition is there that they need to be seen. Then the presentation of booking and making it consumer-centric.
The challenge is that these independent companies that are trying to accomplish that don’t have enough technology under their belt in terms of the integration into the different EMR systems to make that a seamless process. It’s almost standalone. When we get to this standalone basis, practices go, "I’ve got to maintain three different schedules in different systems.” They’re not syncing together. Wouldn’t that be great if they could?
My belief is that you can do that if you put the time and effort into it. It comes with experience and time and a lot of effort, but when you do it right, it’s a seamless transition. We don’t care as consumers what happens on the back end of stuff. I don’t care about my plane when I fly. I want to have a decent experience, but mostly I just want to get there safe and on time. How it all works and how all the baggage gets there, I don’t know and I don’t care. I just want to see my bag come out when I get there.
That’s true about anything that consumers interact with. They just want to make it work and make it easy. On the back end, it’s fairly convoluted. There’s different systems in a clinic, for instance — different EMRs, different PMs, different schedules for providers, different ways that providers are using their schedule to book breaks and lunch breaks, and different things like that. It’s tough to read that and get it right so that when a patient books an appointment, it’s done — with the right provider, in the right location, and when they’re actually available. That’s been a challenge for a lot of companies that are trying to make their way through that process.
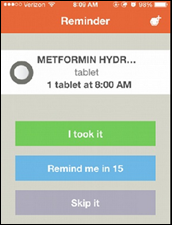
Is it now common for practices to use text messaging to send appointment reminders and to allow patients to text a cancellation message so the practice can open up that appointment slot to someone else who would most likely pounce on it?
It’s definitely available. Technology can do that. We’ve been doing that for a long time. But when you think about widely used, I would say it’s not.
It’s interesting to compare medical care to dentistry in sending text messages and connecting those to workflow. It’s around 50 percent in dentistry and 6 percent in the ambulatory space. Why is that? The adoption isn’t there yet. That’s why companies like ours and others are out there beating the drum and saying there’s a better way.
At some point, we’re going to ask, when we’re looking at a new practice, what insurances do you take and are you text enabled? The ability to get to that practice whenever we need to in a reasonable fashion. The phone number and the text lines are the same. There’s no app to download, no new numbers to learn, no short codes or all those crazy things that some companies get caught up in that don’t make any sense. The consumer experience in understanding how to make that easy and accessible. That’s what patients will start talking about and expecting.
Once that kicks in, everything you talked about takes place. It can be a completely automated fashion, whereas today it’s just archaic the way we do things. One practice’s goal is to completely eliminate the telephone. You think about that and go, how could you do that? Well, it can be done, and they’re well on their way to becoming a completely 100 percent text-enabled practice, period. That’s an interesting dynamic when you start thinking that practices are starting to actually think about that. That’s revolutionizing the way that we communicate.
It was the same way when the telephone first came into practice. Why wouldn’t you have people walk in and talk face-to-face? You’re going to have a telephone? That was a revolution. Now it’s going away from that and getting to communication that’s more efficient, more effective, more cost-effective, and more scalable. Practices win and the consumers or patients win, too.
Do you have any final thoughts?
When I think about healthcare and the experience that we have, both on the provider side and the patient side, I’m pretty sure I know how the movie ends. I think I can see in the future and I think everybody can envision it in 25 years or 50 years. We’re going to have accessibility and it’s going to be almost immediate. We can all picture how much better it will be, but you have to do something now to get there.
It’s really important for practices to evolve, and consumers will push that evolution because their expectations are already there. It’s important for physicians to embrace technological change because that’s what the expectation is.
Healthcare can improve and not lose that personal touch when you’re thinking about what the end of that movie looks like in the next 20 years or 30 years or 50 years. That’s what inspires me personally. That’s why I’m involved with healthcare and in building technological solutions. It’s a shared goal that we should all have in building a better future. We can do so many amazing things with technology today. It’s just a matter of embracing that, understanding that, and feeling good about change.













































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…