Top News

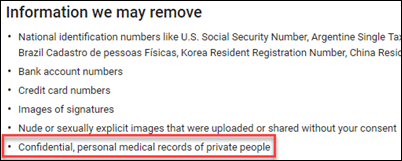
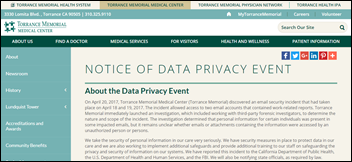
Google adds medical records to the handful of categories that users can ask the company to remove from searches. Someone whose medical records have been exposed inadvertently or otherwise can ask Google to hide their information from its search results.
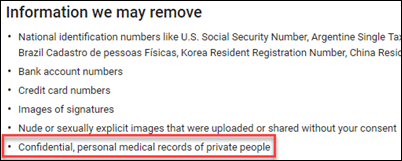
Medical records thus join the Google categories of federal ID numbers, bank account numbers, credit card numbers, scans of signatures, copyrighted materials, and revenge porn that are already covered by Google’s removal policies.
The material is still visible on whatever site posted it, but is less likely to be discovered when it’s filtered from Google searches.
Reader Comments
From Vendor Locking, Data Blocking: “Re: Cerner and the DoD/VA. You covered this a year ago and it’s even more outrageous in light of the VA’s decision. Cerner forced the DoD to host MHS Genesis because, by Cerner’s rules, only Cerner can, even though the DoD finds that it’s technically doable by others. Cerner ‘is not willing to negotiate at this time for the procurement of the data rights that would enable the government to utilize the Cerner solution in a competitive environment.’ Why? Because it ‘could adversely impact Cerner’s … competitive market advantage.’ Is this is the good faith Shulkin should expect heading into negotiations without a competitive bid?” I don’t know much about government procurement (and don’t want to), but publicly naming Cerner and presumably Leidos as the VA’s no-bid vendor for a contract whose value could exceed $10 billion seems absurd regardless of the Congressional pressure the VA is facing. The DoD messed up in failing to force Cerner (pre-contract, of course) to open up the DoD’s hosting options even though Cerner came up with a hollow-ringing excuse about population health management requirements, forcing us taxpayers to ante up a few more dozen million dollars that unfortunately constitute little more than a rounding error in the massive project.
From Supine Position: “Re: losing an IT job when systems are replaced. It’s SOP for health systems implementing Epic.” Indeed it is. Epic forces its own employment model onto its customers, requiring experienced hospital IT employees to interview competitively for newly created Epic positions and to take Epic’s bizarre but apparently effective logical reasoning and IQ-type tests that are scored secretly by Epic, resulting in only a gladiator-like thumbs up or down passed along from Epic to the hospital’s project executives who defer to Epic’s wisdom for fear of rocking the boat of their employer’s gazillion-dollar project. It’s almost like Epic is invalidating the hospital’s own methods of choosing and keeping employees. The rank and file who get passed over for the Epic team are thanklessly turfed off keep the legacy system lights on, huddling depressed like death row inmates as they watch former teammates head off to new physical locations, Epic training, and a secure employment future. I’m surprised that hospitals are readily willing to part ways with employees who have decades of experience, but on the other hand, the Epic model of creating new jobs and then eliminating the old ones is a convenient way to clean house without feeling guilty. Make no mistake – when your health system employer chooses Epic but not you, your IT life, your social standing among peers, and perhaps your city of residence will change.

From Interested: “Re: Quantros. The CEO is leaving, according to this announcement that identifies her new position.” A May 26 trading update from Informa PLC says that Quantros CEO Annie Callanan will join the business intelligence and publishing company this summer. She joined Quantros in July 2014.
HIStalk Announcements and Requests
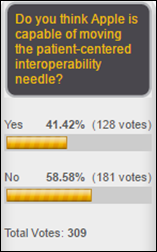
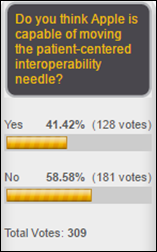
The majority of HIStalk readers don’t believe Apple will live up to the hype in making the iPhone a significant interoperability component. John Smith says Apple doesn’t understand interoperability but instead is mostly interested in selling hardware to customers of its walled garden. Nick predicts Apple will be Fitness Trackers Round Two in giving already healthy people yet another gadget to play with. JC says the company’s deep pockets and strong consumer focus could allow it to make a difference, while Mobile Man says people need ways to store and share the medical information of themselves and family members that could be accessed by providers and anything Apple can do to support that would be great.
New poll to your right or here: Have you ever lost a job due to a health IT implementation?
Jenn did a great job covering for me while I was on vacation for several days. I like that she makes me at least temporarily redundant so I can get away without worrying about HIStalk, although I’m always anxious to get back in the saddle.
My candidate to become the next MySpace – LinkedIn, which under Microsoft’s ownership has become maddeningly slow, is being bloated with questionably useful and unintuitive features, and is becoming a nagware showcase of trying to get users to buy premium services. I actually dread looking someone up on LinkedIn now, nearly as much as I hate getting unsolicited pitches from it (like never-ending recruiter spam and generic partner pitches from India-based companies).
Webinars
June 29 (Thursday) 2:00 ET. “Be the First to See New Data on Why Patients Switch Healthcare Providers.” Sponsored by Solutionreach. As patients pay more for their care and have access to more data about cost and quality, their expectations for healthcare are changing. And as their expectations change, they are more likely to switch providers to get them met. In this free webinar, we’ll look at this new data on why patients switch and what makes them stay. Be one of the first to see the latest data on why patients leave and what you can do about it.
July 11 (Tuesday) 1:00 ET. “Your Data Migration Questions Answered: Ask the Expert Q&A Panel.” Sponsored by Galen Healthcare Solutions. Presenters: Julia Snapp, manager of professional services, Galen Healthcare Solutions; Tyler Suacci, principal technical consultant, Galen Healthcare Solutions. This webcast will give attendees who are considering or in the process of replacing and/or transitioning EHRs the ability to ask questions of our experts. Our moderators have extensive experience in data migration efforts, having supported over 250+ projects, and migration of 40MM+ patient records and 7K+ providers. They will be available to answer questions surrounding changes in workflows, items to consider when migrating data, knowing what to migrate vs. archive, etc.
Previous webinars are on our YouTube channel. Contact Lorre for information on webinar services.
This Week in Health IT History

One year ago:
- Massachusetts General Hospital (MA) notifies 4,300 patients that their information was exposed in a February 2016 breach of dental practice systems vendor Patterson Dental Supply.
- McKesson announces that it will divest its Technology Solutions business into a new joint venture company that it will co-own with Change Healthcare (the former Emdeon).
- The VA signs up for IBM Watson to bring precision medicine to cancer treatment.
- Teladoc announces its planned acquisition of consumer engagement platform vendor HealthiestYou for $155 million.

Five years ago:
- ONC’s Director of Meaningful Use, Joshua Seidman, PhD resigns to take a job as managing director of quality and performance improvement with Evolent.
- The Supreme Court rules to uphold the ACA, including the individual mandate.
- A GAO report finds that the VA and DoD have made progress in their pilot project to integrate care at the James A. Lovell Federal Health Care Center (IL), but delays in implementing the IT component have created additional costs.
- Practice Fusion gets $34 million in Series C funding from by Artis Venture.
- Five senators introduce a bill that would create a national standard for notifying affected individuals about information security breaches.
Ten years ago:
- Michael W. Carelton joins HHS as CIO.
- The Healthcare Solutions business of JPMorgan Chase and RelayHealth offer an integrated set of claim and payment processing solutions.
- Mediware delists itself from the NYSE Arca stock exchange.
- Two DoD medical agencies attempt to stifle use of the Joint Patient Tracking Application so they can spend millions to build their own.
- Cerner gets 510(k) clearance for its new transfusion and specimen collection system that will be marketed under the Cerner Bridge Medical name.
Weekly Anonymous Reader Question
Last week’s survey: what is the best practice you’ve seen for a company to encourage gender equity?
- Pay equality.
- Promote the qualified women into management, upper management, and into the C-suite.
- I have not seen this implemented anywhere, but names should be removed from resumes. Resumes should stand alone on the quality of the content, not the name of the applicant. This would also level the playing field for people who get bypassed (and there are a LOT who do) for their “ethnic” sounding name.
- Can we please stop referring to our MAs, RNs, and receptionists as “girls,” as in “I’ll have one of my girls get that for you” or “My girls didn’t come in today, so we unable to see patients.”
- Actually promote women to senior line roles. Most senior teams are a horde of white guys and a few token women in legal, HR, and marketing.
- Data, data, data. Benchmark all positions against market rates and target hiring/paying everyone at the 50th percentile. Stop asking new hires what they make (now the law in Massachusetts); decide what the position is worth and pay that to all applicants.
- Having a respected female leader.
- Hire more men? Not always true at upper management, but at middle and down, my teams have been dominated by women for as far back as I can remember. Nurses (female-predominant career) switching to IT plays a huge role in this.
- None that I’ve seen, but the term gender equity is a good example of an oxymoron.
- Truly following an employee engagement strategy like those from Gallup, Press Ganey, etc.
- It’s not really a best practice per se, but I started my career at Epic, and as a female, I did not see any limits to my career based on gender. The CEO and many senior leaders are female. I think having that as a first example helped shape what I will accept and what I have sought out culturally at future employers.
- Several years ago while I was on active duty, the Air Force opened fields that were previously closed to women. Of all the careers positions that I have held since then, I have come to appreciate that no organization does a better job at “assimilation” than the military.
- Promoting a feminist to CEO.
This week’s survey: If you were offered a new job, what would be your limit on expected weekly work hours and travel requirements? I’ve never had a travel-intensive job so I don’t really know how that works, other than I’ve heard people gripe about spending their evening hotel hours catching up on work after a full day in front of clients and prospects. Maybe my next survey should address travel tips from road warriors who have learned to live out of a suitcase with little time back at the office.
Last Week’s Most Interesting News
- Senate Republicans publish the Better Care Reconciliation Act of 2017, the GOP’s renewed effort to repeal and replace ACA.
- Theranos reaches a tentative settlement with Walgreens that would result in the retail pharmacy getting only $30 million and losing more than $100 million of its original investment.
- Teladoc acquires Best Doctors, a telehealth vendor focused on offering remote second opinions to support complex medical cases.
- CMS publishes the 2018 Quality Payment Program proposed rule.
- FDA Commissioner Scott Gottlieb, MD outlines his digital health plans for the agency, which include the development and launch of a third-party certification program for low-risk digital health products.
Announcements and Implementations
The ACOs and IPA of Orange Care Group will implement Epic’s Healthy Planet population health management system and will also offer its EHR via Memorial Healthcare System (FL) and Epic Connect.
Government and Politics
Some of the scariest words I’ve heard out of Washington, DC involve the idea that people shouldn’t be forced to buy health insurance they “don’t want or need.” Who might that be, other than psychics who can predict with certainty that they won’t have an auto accident, experience a stroke or heart attack, get hit by an exploding genetic time bomb, or find that they have cancer? Choosing not to buy insurance is a gamble in which those who bet wrong on the likelihood of circumstances beyond their control stick hospitals with their bills (and thus everybody else who was responsible enough to insure themselves), receive inadequate care, or lead their families into medical bankruptcy. There’s a reason that even good drivers are forced to buy auto insurance even though they might rather spend the money elsewhere. Healthcare is so expensive that even the relatively rich couldn’t afford the uninsured cost of a major, short-term illness or any long-term one. Personal responsibility in healthcare comes from both lifestyle decisions as well as backstopping the inevitable eventual costs with insurance.
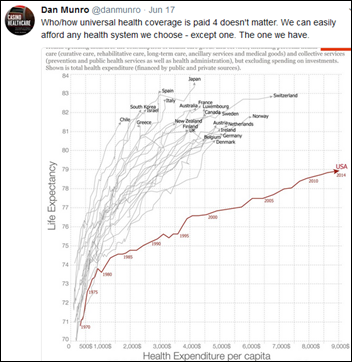
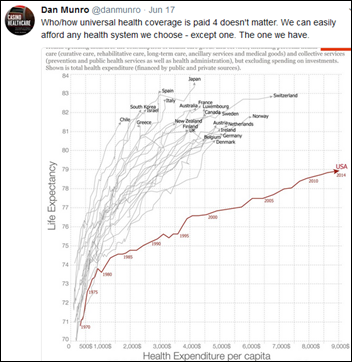
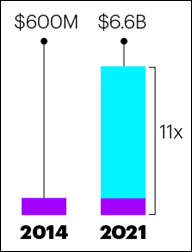
Meanwhile, here’s the most insightful comment I’ve seen on the US healthcare system given that everybody focuses on the cost of insurance that inevitably reflects the cost of healthcare services.
Sales

Australia’s Northern Territory selects InterSystems for its $196 million clinical systems replacement project. Telstra Health, Epic, and Allscripts failed to make the cut from the shortlist, while Cerner, Meditech, and Orion Health didn’t advance to the final four.
Decisions

- Ocean Beach Hospital (WA) will replace Healthland (CPSI) with Epic in October 2017.
- University of California Irvine Medical Center (CA) will go live on Epic in November 2017.
- Winneshiek Medical Center (IA) will replace Meditech with Epic in September 2017.
- Mayo Clinic Hospital – Rochester (MN) will go live on Epic in 2018.
These provider-reported updates are supplied by Definitive Healthcare, which offers a free trial of its powerful intelligence on hospitals, physicians, and healthcare providers.
Privacy and Security

Anthem will pay $115 million to settle a class action lawsuit over the 2015 cyberattack that exposed the information of 78 million people.
Other
A hospital in India denies well-placed rumors that its patient oxygen supply went offline for 15 minutes and thus killed 11 patients, even though reporters seeking information found that the records of the victims had vanished along with the oxygen supply logbook. Administrators of the 1,400-bed hospital say there’s no need for alarm since 10-20 patients die there each day. The same hospital killed two children last year after giving them nitrogen instead of oxygen.
A professor in South Korea says hospitals interested in artificial intelligence should focus their efforts on EHRs instead of IBM Watson. He adds, “I have to question whether we can use Watsons with absolute trust. It seems that hospitals have introduced the technology mainly for publicity reasons. They are promoting Watson to win the competition, especially now that its cost is falling.”

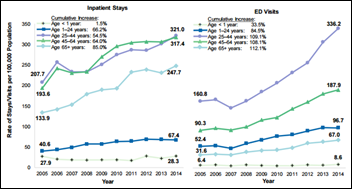
A depressing New York Times article covers the opioid addiction problems of Delray Beach, FL, whose paramedics responded to 748 overdose calls in 2016, 65 of them involving fatalities. Most of the victims were from elsewhere since the town has several addiction treatment centers that draw in addicts from all over the country who stick around afterward, who are then pursued by minimally supervised, often fraudulent, and insurance-paid treatment centers, labs, and group homes that profit from their relapses. Delray’s mayor notes that you can’t cut hair in Florida without a license, but you can run a substance abuse center. Also noted is that the Affordable Care Act gave young addicts insurance that made them a target for unscrupulous operators found in abundance in South Florida, to the point that they try to steal business from each other by offering addicts manicures, gym memberships, and sometimes even drugs, also rooting for their relapses that restart the insurance benefits clock. Residents complain that the rapidly proliferating sober homes create endless noise, property crime, and homelessness once a resident’s insurance runs out.
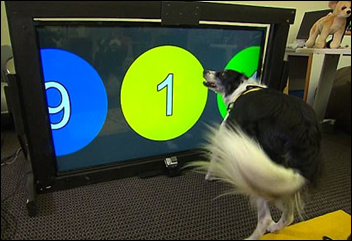
Georgia Tech researchers are developing a touchscreen that will allow dogs to call 911 if their owners experience distress or ask them to summon help. Those in technology-powered homes who plan in advance might name their dogs Alexa or Siri to double their chances of obtaining assistance.

Weird News Andy notes the potential rollout of “self-driving doctors,” in which a Seattle design firm proposes a rather ridiculous system of in-home monitoring and a self-driving health pods that people step into to have their health-related measurements taken at their own location. The pods would also offer telemedicine sessions and dispense medications via artificial intelligence, whatever what means. The company says it’s just a concept, but adds that “there’s a very big need for much better care experiences.” I wish the many people who propose Jetsons-like ideas for improving health would take the time to understand it first, particularly from a public health perspective, but unfortunately all the techno-gimmickry focuses on that small population of self-paying people who can theoretically fuel a company’s bottom line.
Sponsor Updates
- QuadraMed, a Harris Healthcare company, Sagacious Consultants, The SSI Group, T-System, ZirMed will exhibit at the HFMA ANI Conference June 25-28 in Orlando.
- Surescripts will exhibit at the AHIMA Long-Term Post-Acute Care & HIT Summit June 25-28 in Baltimore.
- Verscend Technologies releases a new podcast, “why value-based care requires ‘strength from all sides.’”
- ZappRx names Julia Austin (Digital Ocean) to its board.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates. Send news or rumors.
Contact us.



























































While unsanctioned AI tools are likely causing great consternation for CIOs/CISOs, the industry has a long track record of clinical…