
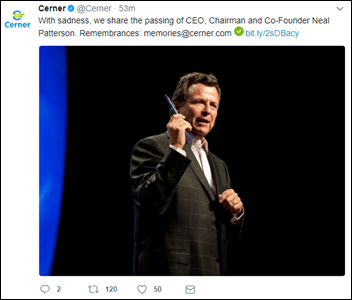
I invited readers to share their thoughts and memories about Neal Patterson following his death Sunday. I’ll keep this page updated with new submissions from the guestbook form and from my LinkedIn post comments.
I remember doing rounds at Spectrum Health in Grand Rapids Michigan many years ago and Neal kept saying, “Two seconds is too slow!” Somehow I think he believed if he said it enough, it would come to pass. Alas, we in healthcare IT wish for that kind of performance. A true visionary, passionate and compassionate leader lost too young. (Kate Crous)
Neal Patterson had great vision and will be missed.
As an EHR veteran for 20 years, I’ve always felt that Cerner was a “good guy” in the emerging market. Am sad to see his passing and thoughts and prayers are with his family. (Matt Ethington)
My deepest condolences go out to Neal’s family, friends, and colleagues. For nearly four decades, Neal’s vision and spirit helped transform the healthcare landscape in a way that will have a lasting impact for generations to come. (Judy Faulkner)
Neal Patterson was controversial in and out of Cerner. He pushed a lot of buttons and sent many an executive on a high-speed-wobble. He was a hands-on executive with a vision that held true for decades.
I always looked up to Neal as someone who used his vision to craft an entire industry. For those of us old enough to remember, he was doing clinical computing when clinical computing wasn’t cool. It wasn’t easy to sell clinical applications to CFOs who ruled IT back in the 80s and 90s, yet Cerner always prevailed. He created a clinical software and services company that did revenue cycle, unlike his peers who grew up during the gold rush of revenue cycle dominance a couple of decades ago. His vision that eventually the revenue cycle would become subservient to the core of patient care, where the patient is treated and where medical knowledge resides, proved true as the industry moved to his vision allowing Cerner to become a dominate healthcare companies in the world.
Healthcare can be flaky as a business. Companies come and go as our government shifts policies and changes funding. Few companies have the patience to survive the waves of change. Neal was a one-of-a-kind who saw a future in healthcare and was unwavering in staying the course, even when the course was hard to see through the fog of regulatory uncertainties we’ve experienced over his professional life.
While Neal was a tornado of a businessman, he not only leaves the legacy of Cerner, but also leaders who spawned out of Cerner to run many of the major corporations in our industry – maybe more than any other healthcare company. I’ve met many of those leaders and they all have the same get-it-done, make-no-excuses, grit that Neil fostered in them in building the culture of Cerner. I tip my hat to one of the original entrepreneurs in our industry. (Ivo Nelson)
I got involved with our Cerner EMR Committee at the start of my career, and worked on Cerner pretty happily for 15 years. I got to know Neal over that time and found him to be the CEO you would want in an HIT company – he was a visionary that made things happened. He listened to clients and cared immensely about making their product better and improving the healthcare system at the same time. I enjoyed his quirkiness and quick mind, which made me realize that it’s OK to be a rebel in healthcare. And in fact, this is the quote that I think embraces Neal the best: “Without Rebels, The Storyline Never Changes.” (DrLyle)
Sad news. Neal was indeed a great competitor and as EXVP of IDX I competed with him many times. The industry has lost a valuable asset in changing healthcare. (Bob Galin)
Absolutely loved that man. He was a warm, and dedicated soul. He “got it.” His visionary leadership style has been inspirational. He will be sorely missed. (Alistair Erskine)
I had the pleasure of working with and for Neal for 16 years (not directly). Neal was a visionary. He was brash and intense and at the same time one of the most down to earth and loving people I had the opportunity to know. Neal was passionate about leadership and about culture. He was passionate about innovation and interoperability. Because of his amazing leadership, Cerner will be a place where I am proud to be for another 16 years. We are changing healthcare for the better with our clients and that, in the end, will be Neal’s legacy.
I was a pioneer with the original HBO. I remember when Neal started Cerner. I had just started my own market research firm. He was a real inspiration and a patron to healthcare IT. He left behind wonderful successes in healthcare IT. Many people have had the luck of working with Neal and I bless God that he gave me the opportunity 20+ years ago to conduct his win loss and customer satisfaction studies. Neal had a passion to understand his marketplace and customers and really cared as he was actually involved. I learned a lot from him, like so many others have. Thank you — I will miss you.. (Cynthia Porter)
I bumped into Neal at the Cerner Health Conference one year and made him laugh with my impersonation of an Irish presenter at CHC. He seemed like a hard-driving yet friendly guy.
As a Cerner customer, I had the opportunity to meet Neal on several occasions. I can say without a doubt that he truly wanted to improve the care of patients. One can argue the pros and cons of how he went about that, but I don’t think anyone should doubt that his ultimate goal was to improve the patient’s experience and outcome.
Much has been and will be written about this remarkable man and industry icon. In the many interactions I had with Neal over the past 30 years, one thing was clear — this man was purpose-driven and committed to solving healthcare’s most vexing challenges and to those who worked with him. He built a great company and will be missed. My condolences to his family and friends. (Scott Kolesar)
I had the honor of working with Neal for 20+ years and his passion and leadership will be sorely missed. He never backed down from a challenge and inspired us all. Condolences to Neal’s family and the entire Cerner family. (Sam Pettijohn)
Sad day for our industry. I interviewed with Neal for my start at Cerner in 1990. Thanks for the opportunity Neal and may you Rest In Peace. Thoughts and prayers to Neal’s family. (Jay Deady)
A very sad day! (Bill Gouckenour)
Wow, so many people got their careers started in HIT under his tutelage. (Michael Silverstein)
With a heavy heart, I express infinite gratitude for being in the Cerner family. Neal’s vision and unparalleled tenacity had me at hello. Goodbye is hard. (Jean Scherschel)
I started working for Neal I the early years of Cerner. He was a leader and visionary beyond all. This is a loss of an amazing person. (Sarah Sample-Reif)
Sad to hear the battle was lost. I am proud I worked for Cerner and was led by a man I must say impacted more people to be better and accomplish more than any other man I’ve personally met. His imprint is upon so many other companies because of the leaders he and the Cerner team built. Condolences to his family and the entire extended Cerner family. (Mark Horner)
Possibly the most progressive and visionary health IT executive in the world. Will be seriously missed. RIP and my condolences to his family and all Cerner employees. (Rick Valencia)
His legacy will continue. My condolences. (Jarrett Runey)
Hit me hard when I read the news today. 67 years young and really transformed HCIT. Made a real difference. All the best to family friends and colleagues. Too young to be gone. RIP. (Jim Maughan)
I love it when a good personality leads a high pressured and elevated role. I could sense his smiles throughout the photos. (Alex Guizzotti)
Proud to have been mentored by Neal for 26 years. Neal was always there for me and my family. Rest In Peace my friend, leader, mentor, and fraternity brother. (Ken Boyett)
I have had the opportunity to be both a client and an employee of Cerner. While I’ve never been fortunate enough to get to know Neal personally, his vision and leadership has significantly influenced my career the past 20 years. Cerner is the company that I measure all other vendors against. It was not surprising to hear that a succession plan was in place and a new CEO would be named shortly. I hope Cerner continues to challenge the status quo and move us to new heights. I am hopeful that Neal was able to instill his way of looking at the world in his top leadership. He will be missed. (Sheri Rawlings)
I would like to extend a posthumous thank you to Neal for creating an organization that introduced me, and countless others, to the complex and wonderful world of healthcare IT. The recruiting program at Cerner Corporation has brought scores of talent into our industry. As it was with many of my fellow recruits, I entered the health IT world wide-eyed and eager to learn with very little (that’s generous) knowledge of healthcare. The Cerner jumpstart program was a constant feeling of drinking from the fire hose. We worked long hours, had some great fun, and established lasting bonds and relationships. I remember those days fondly. Mr. Patterson was a healthcare visionary, entrepreneur, and fraternity brother that will forever leave a lasting mark on healthcare and myself. (Don C. Ellis)
Neal Patterson was brash, arrogant, and aggressive. Yet despite some of his less admirable personality traits, we have to admit that he did reshape the healthcare IT industry. Neal took a relatively small lab company and changed it into an innovative, expansive, and formidable enterprise. By changing Cerner, he inadvertently changed all of his competitors who designed, developed and sold hospital information systems – whether we knew it, or even liked it, we became better vendors because of Neal. I’ll never forget his full-page picture in the Wall Street Journal. And, yes, “tick, tock” — time runs out for us all. Rest in peace, Neal.
I worked at Cerner for a brief time and everyone always referred to him as Uncle Neal. When the news of his passing was made public, I received at least 10 text messages among my Cerner friends- all of us in shock. Did you know that Cerner requires all new staff to receive orientation in Kansas City no matter where their home base is? Kansas City is a different place because of Cerner and Uncle Neal. RIP
Neal gave me not only the opportunity of a lifetime, but a renewed passion for the health and care of people. Even though I only got to meet him twice during my 14 years at Cerner, he was a daily inspiration to me and helped me get some very tough days. RIP Neal. You’ve made me a better person. (Liz Chamberlain)
A great guy, and he treated everyone with dignity. I met him abut 10 years ago when I was providing services to him and his wife, Jeanne. They were both kind and unassuming. Neal was appreciative, and even took time to get to know me. As busy as he was, and with all he had going on in his life, it was amazing that he would take the time to be such a decent and pleasant guy to someone like me. I remember one evening my wife and I were walking on the Plaza, and encountered him as he came out of the Capitol Grille. I said hello to him, and he courteously acknowledged me. As we walked on he suddenly ran after me, he had obviously just remembered me (as I was not in uniform and in a completely different environment from where he would normally see me). He just could have not been nicer, and even remembered that I had told him that my wife regularly utilized Cerner programs in her management job at a local hospital. What a memory for as busy as he was. Again, a great guy. He will be missed. (Tom Scatizzi)
Deeply saddened by the loss of a health IT giant and bold visionary. Neal inspired and made it possible for thousands in my generation to start and pursue meaningful health care careers where we can make a difference. I have infinite gratitude to my Cerner family and remember my time there fondly. It’s an honor to have known Neal and to have had personal interactions that I will cherish dearly as treasured memories. For many like me, he remains a lasting example long after last encounters. (Santosh Mohan)
A leader in our industry. Respected by all. A legacy that will live on for decades. Thank you for what you brought to healthcare and technology. (Tom Aikens)
This is indeed sad news to read of Neal’s passing. Like many on this post and countless others, Neal instilled vision and passion in his work, those who worked for him, and transformed HIT like no other single person — he was a contrarian that often bucked conventional wisdom and pushed his organization and the industry to innovative heights. Building Cerner from a meeting on a park bench with friends Cliff and Paul and idea born on the back of a napkin, very few CEOs can lay claim to Cerner’s shareholder ROI over the years. (Greg Leder)
Neal was one of the smartest people I ever met and one of the greatest business minds of any founder/CEO of any industry, let alone healthcare. I met him when he was taking the young lab IT company to a new level with an inpatient system and Cerner was installing it in a brand new hospital in Edinburgh, Scotland. I was supplying the cardiology and patient monitoring stack with Marquette. We made an attempt to buy Cerner after that — you can imagine how long it took him to turn us down.
Later, after starting Picis, we met again and I told Neal that he wasn’t getting the market credit for the complete rewrite of his codebase which was well received by customers. He listened to people and he started to pitch that to the analysts and the stock appreciated quite a bit. Though we eventually became quasi-competitors, Neal would personally stop by the Picis booth every year at HIMSS — once with a young associate who he said to in front of me, “Watch this company.” I took that as a great measure of pride and respect.
Neal built a great team — the Cerner culture is one of a strong sales culture backed by execution and delivering. From his partner Cliff to Paul Black, Trace Devanney, Bill Miller, Mike Valentine, and Zane Burke today — all are leaders in Neal’s image. They know because while being a bear to work with/for, they all came away with great leadership skills. The people I’ve hired out of Cerner know how to get things done. Look at the tremendous same store sales record Cerner has had with its customers over the years as a testament.
Neal was one of those people in my life that greatly influenced me — one that I could sit around with for hours and just engage in the most vibrant conversations I’ve ever had about our industry, politics, Ayn Rand, human nature, you name it. We will miss you greatly, Neal! (Todd Cozzens)
When you look back over your career and think about leaders that made you better, anyone that has worked with Neal would have his name high on their list. The healthcare informatics industry is better because of Neal and the leaders he has supported, coached, mentored, and pushed over the years. Neal has seeded this industry with some of the best and brightest leaders in this industry, including Paul Black, Mike Valentine, Bill Miller, and Zane Burke. His legacy and his vision have been left in good hands! Rest in peace, Neal. We will continue to pursue your vision.
I had the good fortune of working for Cerner for 16 years, half of it in the early days. When Neal would begin to spin a tale of the intersection of health and IT, it was spellbinding, engaging, dramatic, motivating, and above all, about improving the quality, dignity, capability, and humanity of all involved in the endeavor. He has been an inspiration, a motivation, and mentor for many of us. But to me, he was the guy — the leader — the reason to work in this industry. He will be sorely missed. His ideas will live on in the next few generations wherever health is impacted by IT.
Every once in a while you meet people who are doing exactly what they love and are called to do. Neal was one of those people. This news is sad. He was inspirational, innovative, provocative, entrepreneurial, yet personal. The world is a much better place because of Neal Patterson and Cerner. (Doug Pousma)
Neal will be missed. (John Simmerling)
Although I didn’t know Neal Patterson at all, his name and company were well known to anyone in the industry. I was fortunate (or so I think!) to have joined the HIT industry around 17 years ago and still laugh at some of the crazy things vendors did back in the day to convince docs they needed to get on the bus. I really enjoyed reading the HIT eulogies from others in this industry who have also been a part of this movement, both leaders and others like me who were just blessed to be a part of the movement. It was interesting to see who added their thoughts, as well as those who didn’t. That being said, Neal Patterson won’t be the first or last to leave the planet, but I want to thank him for all the things he did to keep this HIT stuff moving forward. Thoughts and prayers to NP and his family! RIP Neal Patterson.
Healthcare IT is such a difficult place to do business in, and on top of that, to have a vision and look into the future. Not many people have that. Always amazes me that it all started on a bench in a park. Visionary and a true leader. Neal, you will be missed.
Rest in peace, Neal. It was an honor to have had the pleasure to know him, to have been a proud member of the Cerner family, and watch him build a formidable legacy which will continue to unfold far into the future. My deepest condolences to the Patterson family. God Bless! (Guillermo Moreno)
One of the few leaders in our industry who did the “right” things for the “right” reasons. (Mark Edelstein)
I never worked for Cerner, but as a business partner of Cerner’s many years ago, I was in a handful of meetings with Neal, always a small group of four or six. Driven, passionate, and visionary is how I would describe him in those meetings. While I didn’t always agree with Neal’s position, there was no denying that he was a driving force and advanced our industry. His contributions to HIT have been invaluable and everlasting. RIP. (Jim Hall)
All of us who worked in the Cerner family learned from Neal Patterson’s passion, drive, and vision. All of us who knew him are better for the experience, and the world is poorer at his passing. RIP Neal, and respects and condolences to your family, and the great company that was your passion for so long. (James Hazy)
He made a difference in so many lives, including mine. The man had a well lived life, overcoming obstacles as they arose with his own style — brash or pushy to some, direct and incisive to those who got his vision. Show me another CEO who can stand up and answer and ask questions about the entire company for 3+ hours year after year, who saw the big picture and drove innovation years ahead consistently. We need him now more than ever, and he will be missed. If you don’t have a Neal Story or two (even if handed down), you didn’t work at Cerner. You can shove that Pie Award. (Joe Boyce, MD)
Exceptional visionary and indeed he created a visionary company. His legacy isn’t just Cerner, but also the leaders he created that went on to lead many other companies — creating a much wider AND generational impact. I had the privilege of working for him and earning my stripes. He had this innate ability to extract the best out of you! He will be missed! (Hemant Goel)
Neal was an extreme visionary leader and a demanding manager. I’m glad to have worked under his tutelage. (Rich Marra)
My deepest condolences to the family friends and colleagues of Neal. He was a true visionary that helped to transform the delivery of patients, families, and communities world wide. His spirit, passion, and vision has helped all of us drive for improvement.
This world is a better place thanks to his work and that is a beautiful thing. Thank you Neal for helping us take care of one patient and family at a time. Rest well, Starfish. (Cynthia Davis)
Though we met only a couple times — in the Cerner Vision Center when I was a much younger Cerner implementation project manager — your enormous Midwestern presence in those meetings made an endless impression on me. Your ability to see a day in the not-so-distant future when data-driven healthcare delivery would make a positive difference in peoples’ lives is here! As someone who shares in this same vision, I am forever grateful for your work and the opportunities your pursuits have afforded me and many, many others. Rest in peace, Neal Patterson. Your innovative spirit lives on, now more than ever. You will not be forgotten, sir. (Jamie Trigg)
I first met Neal in 1994. A kind but driven man with a vision. He altered the landscape of healthcare and thus the lives of many. Thanks, God Speed Neal. (Tom Liddell)
Neal’s years of dreaming, passion, and creative engineering have brought much to our healthcare system and others around the world. It was always an exciting environment in the vision center with Cliff and Neal driving, energizing and listening to all who would share their passion and convictions for dramatic change and a better system of healthcare. From labs, to hospitals, to health systems, to integrated delivery systems, CINs and ACOs and National Delivery models they and all the leaders who grew up in Cerner (the list is too long to list here) brought so much energy and commitment to making things better for patients, people/employees, and now consumers. My best wishes to all those in his family at home and all those Cerner family members who shared their lives with him. We are all better for his being here with us all these years. God Bless you all. (Jay McCutcheon)
A healthcare game changer and warrior is no longer with us. Neal Patterson has been an icon, a mentor in the industry, and will be remembered forever.
I have been in this challenging arena of healthcare IT for almost 2½ decades. Challenging only because of the constant changes that forced all of us to constantly adapt and re-invent ourselves. I have faced some challenges as an ally to Neal, and some on the other side as competitors. We won and lost some battles together and as competitors. The challenge is what made it fun and Neal’s brilliance made us think harder to stay in the game. The most important thing is that we were always driven by our shared mission and passion to do the right thing for our customers and the healthcare industry. The customers and the industry always won!
As we get older and wiser we all are confronted by our own mortality and realize that we are at that inflection point, where the only way to transform healthcare is by leveraging from the experience gained to this point and joining forces with other game changers to make a difference. Today we should carry Neal’s torch and together execute on our shared vision. We thank you my friend for making us better and joining your mission and vision. We will not disappoint you! (Alan Portela)
Neal’s Cerner was an adventure ride unlike anything Disney had ever imagined. Being on the front lines and having a court-side seat while executing his vision to transform an industry was daunting, crazy, fun, unpredictable, and, above all, incredibly rewarding. For the hundreds of alumni who have gone on to run businesses, the lessons we learned and experiences we gained from Neal Patterson eclipse the most prestigious MBA one could earn.
We vision using white boards, we are never comfortable with status quo, we give ‘pen-raised’ youngsters opportunities beyond their current experiences, and cringe at the words vendor, customer, or employee.
I smile when I think of Neal in Heaven. His new associates will be certain to have their vision statement ready to be recited at a moment’s notice, they’ll absolutely have a riveting question to ask during the Town Hall and, by all means, they’ll know to stay low when a debate gets especially lively.
I extend my deepest condolences to Neal’s family. (Gary Pederson)
Neal was truly an amazing person that never forgot his roots. From the moment I met him, he made me feel very welcome and supported. Like most farm boys, he did not expect people to address him as Mr. Patterson or anything formal. Instead, he would insist that you just call him Neal.
I had the privilege of working closely with Neal for many years and gained invaluable professional experience while also getting to know him personally. Make no doubt, whether in the professional environment or personal, Neal was competitive and encouraged and expected excellence. Those years were packed with many late nights, early mornings, … and fun. Neal would joke that when he was around, others had more fun, but it was a reality. I also got to see the personal side of Neal, which was a very compassionate and caring person, something the business world unfortunately often overlooks.
My hope is that we (not just Cerner, but this industry) continue to do what is right for the person, the patient … us. Let us all be compassionate, caring, empathetic, and make “one last round after sundown” in honor of Neal. Because after all, Neal (and many before him) proved that in the end, health care is personal.
Neal made each of us better. He may be gone from this place, but his legacy lives in each one of us. Let’s make him proud!
Comments Off on Neal Patterson Guestbook Comments















































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…