Girish Navani is CEO of EClinicalWorks of Westborough, MA.

Tell me about yourself and the company.
EClinicalworks was founded in 1999. We have had significant success in the ambulatory electronic health records space.
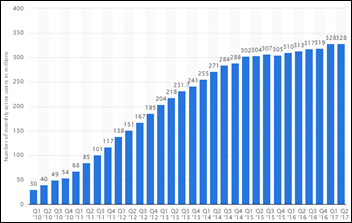
What may not be very easily identifiable is the size at which we have had an impact. For example, last year more than 200 million electronic prescriptions and more than 270 million visits were recorded by a provider using EClinicalWorks EHR. I’d go as far as to add that in last 17 years that other than Epic, no other EHR company has had more physician EHR implementations than EClinicalWorks.
Additionally, over the last five years, we started building products for patient engagement under the Healow brand. We have had remarkable success in terms of acceptance. As an example, last year Healow providers sent 200-plus million reminder messages to patients regarding conditions and visit reminders.
That’s the summary of the company in terms of its footprint and how it gets used everyday in the healthcare space.
The company didn’t admit any guilt in the Department of Justice settlement involving falsified testing results, lack of data portability, and failing to keep customers informed of software defects. Given the limits of what you’re allowed to say based on the settlement terms, what’s the side of the story we haven’t heard?
First of all, let me say this. There are regulatory requirements that electronic health record users have to comply with and there are requirements that electronic health record vendors have to comply with. In 2015 and 2016, there were technical non-conformities identified by the government. Once identified, we addressed them promptly. These non-conformities were not intentional on our part, nor did we know about them and ignore them. Nevertheless, I respect the right of the regulatory authority to enforce the requirements.
We have to move forward. We addressed the non-conformities. We also found a meeting ground on the settlement that allows the company and me to focus on tomorrow. I have resumed my normal work activities, including my personal time with family that got compromised last year. We have developed a stronger compliance program and it has made the company stronger. I am more focused on developing our next EHR version and making a positive impact
Do you think the value of the settlement at $155 million reflected the DOJ’s desire to have a single point of resolution without having to ask your customers to pay back their Meaningful Use payments?
I can’t speculate on all parts of the question. But, yes, the settlement amount certainly represented a portion of the Meaningful Use dollars paid under the program.
How have your customers and prospects reacted since the settlement was announced?
I have received hundreds of positive, reinforcing emails. We’ve done well by our customers. My customers recognize it and I’ve received support from a large number of my customers. I have not seen any attrition attributed to the settlement.
Secondly, in terms of new business, June was our best sales month of 2017. We signed 100 new customers and over 1,000 new providers on the electronic health record side. We did well on the population health side as well, as five new ACOs picked our pop health product. Last Friday, we announced our Q2 2017 numbers. We had a strong June and second quarter in terms of new and existing business.
I would summarize by broadly saying that the customer base likes the product and loves the company. It is my commitment to everyone that uses our product that EClinicalWorks is going to be focused on a much brighter tomorrow and that message is strongly heard by my customers. I am dedicating a lot of my time to making the product and service better. I don’t see why an existing customer won’t be delighted with that information and I think it has been reconfirmed to some extent in June with our continued momentum
What progress has the industry recently made in interoperability and data portability?
I have positive data to share in this particular regard, not just for EClinicalWorks, but for many industry players. I would unequivocally say that Carequality has been successful. We’ve been able to connect many Epic customers on a regular and routine basis.
It’s not just connectivity in terms of data exchange, but the simplicity with which we are able to do it. We’re able to onboard practices within minutes. We built the Carequality Hub in the cloud and we can add new practices quickly. There was a recent article regarding an ECW customer, Eagle MD, a 61-provider group in North Carolina. They have a lot of patients in common with Cone Health, which is an Epic implementation. They talked about how patient care has improved because of Carequality.
CommonWell Health Alliance, which we are also a member of, has had success when it comes to Cerner Hospitals. Some of the other acute EHR vendors have not necessarily put the same energy behind it. I hope that changes and we see more success there.
Broadly, I am excited about the fact that these networks can become equated to Visa or Mastercard networks and interoperability becomes more of a trust model that providers have to activate versus custom software that vendors have to develop. We are there from a technology standpoint. It’s now a question of getting providers to start activating the trust relationships so they can retrieve and send data to any provider as patient care is being delivered.
It is happening. This is not hope for the future. We are seeing data exchange happening every day.
How would you assess the industry’s maturity in managing cloud-based systems based on the latest high-profile, extended outage?
The move to the cloud model is — not just for healthcare, but for the ecosystem of every industry — irreversible. We are seeing business models over the last decade facilitated by the cloud that just cannot be contemplated by on-premises and siloed implementations. Uber doesn’t own any cars and does not own the mapping technology, yet it is now one of the largest transportation companies.
Healthcare is no different. Healthcare has the provider side. Healthcare has the consumer side.
The move to the cloud is an irreversible process. It has to go through its trials and tribulations, but the same can be said for an on-premise system. I would not take this episode to be the barometer of whether the cloud is going to revolutionize the delivery of care. I think it will, and it is as we speak.
What significant changes in the ambulatory EHR market have occurred recently and what developments do you expect going forward?
Let me give you an analogy and then make my point. Microsoft Word, Excel, PowerPoint, and Outlook were mostly on-premise deployments with Microsoft Exchange servers. That has been replaced with Office 365. Not everybody has moved to Office 365, but if you look at both Microsoft and its customer base, Office 365 is the trend. I don’t think that is reversible. You want one cloud service that provides all end user capabilities and IT capabilities — storage, collaboration, and anytime, anywhere access.
You expect the same when it comes to not just ambulatory, but healthcare information technology in general. You need to have a unified cloud service that delivers capability, whether it’s scheduling, EMR, practice management, patient engagement, or population analytics. A customer should expect these to be an unified cloud service.
Will it require significant investment? Yes. It’s not 1, 2, 5, or 10 million dollars. It’s tens of millions in terms of capital, organizational investments, and processes that have to be invested. We’ve gone through this over the last 17 years. We know the effort and capital required. So if it results in any significant market change from a vendor standpoint, it will be based on the ability for those investments to be made.
Alternatively, there is Amazon Web Services and Microsoft Azure. It doesn’t preclude a smaller company from leveraging these platforms and building a cloud offering if they want to. But the product has to be architected first to be cloud-centric. It’s not about taking a client-server product and deploying via Citrix or Windows terminal server in the cloud and merely hosting the system. The true differentiator is a cloud collaboration platform that encompasses all capabilities we just talked about.
Companies that can deliver health information technology via the cloud will succeed over the next decade. The other models won’t survive. You and I don’t get electricity today through generators that we power our individual homes with. We expect the electric grid to deliver power. Users should expect the cloud to deliver data and information powering the devices and not having servers housed locally doing it.
What is the status of the hospital system ECW is developing?
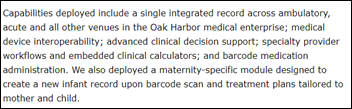
We have two products to talk about. One is for the ambulatory surgery center market. Over the last two years, we developed our ASC offering and have had success with existing customers that have ambulatory surgery centers. This product took us in the OR space with anesthesia documentation, preference cards, surgery scheduling, etc. Our ASC product has been successfully rolled out and we’re able to get many of our customers to now implement it.
We have also, without too much fanfare, been developing our Acute Care EHR offering for many years. Our pathway is different. We don’t want to acquire a company to build the solution. Instead, we partnered with our ambulatory hospital customers as joint development partners, or JDPs. We worked with them to develop the Acute Care EHR solution.
We have a large team of product analysts working on site with our JDP hospitals. We have had good customer acceptance to the whole idea of a unified cloud-centric inpatient-outpatient system that will manage the breadth of the acute care space — from ER on one side to all of the ancillaries that include pharmacy, LIS, RIS, etc. We expect to go live with our JDP customers in the first half of next year.
What challenges do you see as you enter that market, which has had basically no new significant entrants for decades?
First, I see excitement, I am an entrepreneur who has a strong technology background. I thrive on the idea of change. Getting into an established market like inpatient, and to some extent, challenging it with a newer premise — a cloud-based offering — that’s exciting.
What challenges does it offer? It is a wide space. The Acute Care EHR requirements and the number of modules as we count them exceed 25. I would put ER as one module, LIS as another one, for example. There are 25 such modules that we have to develop. The breadth is substantial. It takes significant engineering work, product analysis, and product management.
We communicated to our customers that this was going to be multi-year journey. I am comfortable with the progress we have made. We are getting to the stages of user acceptance testing and integration testing in the second half of this year.
The challenge also is the mindset. Can per-bed, per-month pricing truly change the status quo? If you draw parallels, SAP used to dominate the ERP systems for a very long time. Then came Salesforce, with a different model. Salesforce initially succeeded in smaller footprint enterprises and then it stepped its way up the ladder to enterprise systems that have larger scale.
It’s not uncommon for me to be asked a question, will you be limiting this to a certain size of the hospital? It’s more intuitive for me to answer that we will start with the smaller ones and we’ll step it up. But we are not designing the product to meet the needs of a critical access hospital and ignoring larger hospital systems. The market will accept it on its own terms after we have proven success. I am patient while quite enthusiastic about investing in this space.
What is the population health management opportunity and how are you responding to it?
Population health is primarily being driven by the fact that payer reimbursement for care delivery is changing. EClinicalWorks has developed the analytics platform, the care management platform, and has additionally developed risk models and predictive analytics. From a market share standpoint, when it comes to physician groups that are accountable care organizations, we have one of the largest footprints in this space.
The next evolution is patient engagement. When it comes to home trackers, home monitoring, telehealth etc., we have a sophisticated product offering developed under the Healow brand.
In summary, I don’t see this to be a niche area. I see this to be an evolution of the digitization of healthcare. But then again, that’s how I have always visualized technology. I see this as a vertically integrated supply chain. You start from one end of the spectrum and you go to the other.
The first decade was about digitizing the provider space. The next decade is going to be about digitizing the patient experience and managing panels of patients. Companies that do well in that space will thrive and the ones that build a fully vertically integrated ecosystem will do even better.
You said in our 2008 interview that your goal was to work 15 years and leave behind a legacy of a stable software company that could be turned over to the next generation. We’re more than halfway into that 15 years. Where do you see the company going from here?
I have obtained the first goal that any entrepreneur founder has about a company, which is to have success that can be recognized in its industry. We have attained that.
Along the way, I have developed broader goals. To me, it was always about building a company that outlasts its initial founders. This was the premise that made us not go public or take on private equity.
This area of my thinking has been further enhanced over the years. I expect in my next 10 years to serve a broader population of patients, I’d like to see digital healthcare result in positive health outcomes, I’d like to see our company participate in clinical trials and research. I would like to see genomic data become a part of electronic health records so that precision medicine can succeed.
I am energized and enthusiastic about the next 10 years. Over the last six weeks, I’ve rediscovered myself to some extent and I’m plowing forward. You should expect more from my company and me.
Do you have any final thoughts?
I love my work and I think the future of digital healthcare is bright. Every industry has to go through a maturation phase, I think we’ve attained that in the US healthcare system in terms of the adoption of the basic foundation of digital care.
What we need to now focus on are the benefits. Anytime, anywhere patient care via the use of telehealth and intelligent messaging, genomic data resulting in personalized medicine. I just don’t see why a patient in some part of the world can’t get a second opinion from a neurosurgeon in the US. Many of these broad goals can be attained with the use of technology. It will take some time, but it will happen in this lifetime.





































































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…