Top News


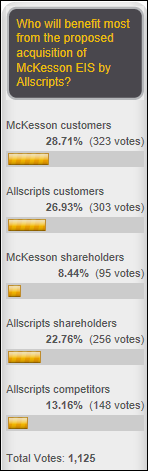
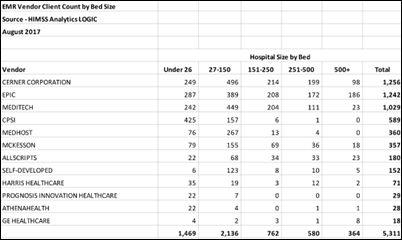
Allscripts will acquire McKesson’s Enterprise Information Solutions health IT business for $185 million cash. McKesson EIS offers Paragon EHR, Star, Series, Healthquest, Lab Analytics and Blood Bank, and OneContent.
Allscripts plans to offer Paragon to small hospitals while continuing to market Allscripts Sunrise to larger health systems.
McKesson announced in June 2016 that it was exploring strategic alternatives for the EIS business as it merged most of its IT offerings with Change Healthcare. It wrote off $290 million in October 2016 related to the EIS business. McKesson will apparently retain RelayHealth and its recently acquired CoverMyMeds, both network-focused, high-growth communications products that are aimed more at pharmacies and insurance companies than health systems.
Meanwhile, Allscripts reports Q2 results: revenue up 10 percent, adjusted EPS $0.15 vs. $0.14, meeting earnings expectations and beating on revenue. MDRX share priced dropped 18 percent in the past year in valuing the company at $2.1 billion.
Allscripts shares rose 16 percent in after-hours trading immediately following the acquisition and earnings announcements.
Reader Comments

From Bow Tie Is Really a Camera: “Re: EClinicalWorks interview. Will it lose a lot of customers following the Department of Justice settlement?” I highly doubt it. While various reports claim that a big chunk of ECW’s customers are considering mass defection, I don’t think that will ever happen since the incident doesn’t affect them personally. They either like the system or they don’t and the high-profile settlement doesn’t provide any new incentive to expensively rip-and-replace even though ECW is now on the hook to provide migration assistance should they choose to move to a new system. It’s not like painlessly boycotting a brand of soda by just reaching two shelves over for the nearly identical sugar water. In fact, the DOJ’s mandated company changes will probably make ECW’s software and support better. People subconsciously try to please a surveyor and to express indignation that they rarely act on. Customers might also appreciate the little-observed fact that ECW paid $155 million in settlement partly to protect them from having to individually repay their Meaningful Use incentives. I don’t think the settlement is going to have much effect on the somewhat stagnant ambulatory EHR market.

From Broken Tiller: “Re: the HIMSS-owned publication. How did they mistake Amazon’s healthcare projects as building an EHR?” There’s so much to dislike about this clickbait piece: the gratuitous “Wait! What?” plea for attention, calling Amazon’s rumored healthcare projects an “investigation,” and claiming in the headline that the companies are building EHRs when nothing in the CNBC article that they reworded into a lame story suggests any such thing .
From Weezy: “Re: Allscripts acquiring McKesson EIS. Why?” Good question. They bought it cheap, apparently, like day-old bread that the store is anxious to get rid of while it’s still sellable. I have to assume that the net present value of the EIS maintenance revenue stream will cover most of the acquisition price. I see no product synergy whatsoever and I seriously doubt that many Paragon, Star, or Series customers will have an interest in moving to Sunrise, just like users of the mothballed McKesson Horizon product – like the market in general — nearly universally passed on Paragon in favor of Epic and Cerner. Maybe the bottom line is that Allscripts just likes to acquire companies (Eclipsys, Misys, Jardogs, dbMotion, etc.) in hoping that it will either all come together or that investors will remain interested in a healthcare vendor that, like McKesson in years past, runs itself like a health IT mutual fund.
HIStalk Announcements and Requests
Listening: new from Alice Cooper, which has some pretty good tracks until things get even better in the final two songs, which feature the surviving members of the original Alice Cooper band, formed by the five Phoenix high school friends in the mid-1960s and named after a minor character in the “Mayberry RFD” TV series of that era. There’s also stunning new EP from Canada grungers Theory of a Deadman that brilliantly and savagely attacks our drug-happy culture. Finally, I’m enjoying outstanding old power pop from The Posies.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre for information on webinar services.
Acquisitions, Funding, Business, and Stock

Medical imaging and data management vendor UltraLinq Healthcare acquires Northern Ireland-based Intelesens, which offers wearable vital signs monitoring devices.
Viome, which offers at-home kit that monitors gut microorganisms to recommend diet changes, raises $15 million in a Series A funding round. Twice-yearly stool sampling and metabolic challenge tests cost $700 per year.

Aurora Behavioral Health signs a $20 million contract South Korea-based EZCareTech, which will create a US version of its hospital information system that is used by Seoul National University Hospital called Best Care 2.0B. They exhibited at HIMSS17, which I summarized as:
I was interested in Best Care, a Korea-based inpatient EHR whose monitors showed a cool-looking product that they are apparently trying to market to US hospitals. I tried to strike up a conversion with the stern guy standing there and he wouldn’t really talk to me. I tried again with another guy and all he said was that company is “from Korea, like K-pop” and then didn’t say anything else. I tried a third time in asking a different person on the other side of the booth if it was OK if a snapped a photo of the screen and they shooed me away. I think the company had best hire some US sales talent if they want to sell here.

Theranos settles the $140 million breach of contract lawsuit brought against it by Walgreens over its in-store Theranos lab sample drawing sites.
Sales
Cedar Valley Medical Specialists (IA) chooses EHR and population health solutions from EClinicalWorks.
People

Sutherland Healthcare hires Shailja Dixit, MD, MS, MPH (Intercept Pharmaceuticals) as chief medical officer and global head of digital innovation.

Health Systems Informatics hires Mary Beth Seaman (Pivot Point Consulting) as VP of business development.

Michael Jackman (GE Healthcare) joins imaging systems vendor Mach7 Technologies as CEO.
Announcements and Implementations
Caradigm integrates Insignia Health’s self-management survey into its Care Management solution.

Community Hospital Anderson (IN) goes live on Imprivata PatientSecure biometric patient verification.
Parallon Technology Solutions leads the migration of the two hospitals of Thomas Health (WV) to Meditech 6.15 from Meditech Magic and Siemens.
Government and Politics
A new CMS rule will allow hospitals to submit only one quarter’s worth of eCQM reporting requirements for incentive payments in 2018 vs. the previously required full year. It also allows hospitals to use either a combination of 2014 and 2015 Editions of CEHRT or either individual edition to satisfy 2018 eCQM certification requirements for CY 2018. CMS says it will determine requirements for CY 2019 and future years “in future rulemaking.”
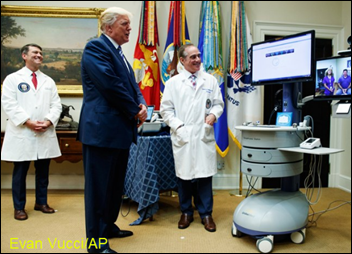
The VA will expand its telemedicine program – the largest in the country — with VA Video Connect in a collaboration with Jared Kushner’s American Office of Innovation, offering virtual visits from 300 VA medical providers at 67 hospitals and clinics. President Trump said in a statement Thursday,
Today, I’m pleased to announce another historic breakthrough that will expand VA services to many more patients and veterans. We will do this through telehealth services. It’s what it’s called — telehealth services.
We’re expanding the ability of veterans to connect with their VA healthcare team from anywhere using mobile application on the veteran’s own phone or the veteran’s own computer. This will significantly expand access to care for our veterans, especially for those who need help in the area of mental health, which is a bigger and bigger request — and also in suicide prevention. It will make a tremendous difference for the veterans in rural locations in particular.
We’re launching the mobile app that will allow VA patients to schedule and change their appointments at VA facilities using their smartphones. So this is something they were never able to do. Technology has given us this advantage, but unfortunately we have not taken advantage of that until now.
CMS withdraws its plan to require hospital accreditors such as The Joint Commission to publicly list the problems they find and the steps being taken to fix them. CMS says federal laws prohibit it from disclosing inspection reports and fears such a requirement could be viewed as an attempt to circumvent the law.
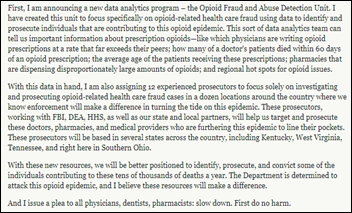
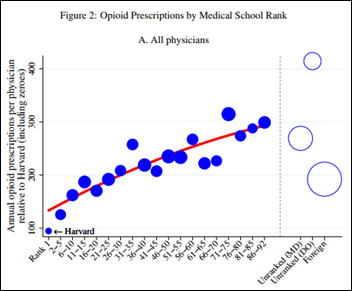
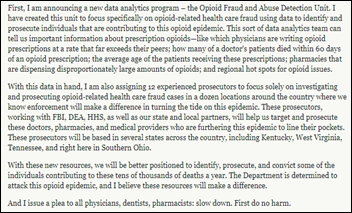
Attorney General Jeff Sessions announces formation of a Department of Justice unit that will seek out opioid-related healthcare fraud by reviewing prescribing and dispensing data for suspicious patterns. The DOJ will also fund 12 assistant US attorneys for three years who will focus exclusively in investigating and prosecuting opioid-related healthcare fraud.
The GAO announces its 15 appointees to the HIT Advisory Committee that will make recommendations to ONC as established by the 21st Century Cures Act. The first five members listed were already appointed b HHS or as consumer advocates:
- Cynthia Fisher (entrepreneur)
- Anil Jain (IBM Watson Health)
- Steven Lane (Sutter Health)
- Steve Ready (Norton Healthcare)
- Patrick Soon-Shiong (NantHealth)
- Michael Adcock (University of Mississippi Medical Center)
- Christina Caraballo (Get Real Health)
- Tina Esposito (Advocate Health Care)
- Brad Gescheider (PatientsLikeMe)
- John Kansky (Indiana HIE)
- Kensaku Kawamoto (University of Utah Health)
- Denni McColm (Citizens Memorial Healthcare)
- Brett Oliver (Baptist Health)
- Terrence O’Malley (Massachusetts General Hospital)
- Carolyn Petersen (Mayo Clinic)
- Raj Ratwani (MedStar Health)
- Sasha TerMaat (Epic)
- Andrew Truscott (Accenture)
- Sheryl Turney (Anthem Blue Cross Blue Shield)
- Denise Webb (Marshfield Clinic Health System)
ONC announces a five-year plan to switch from its own custom EHR certification testing tools to industry-developed replacements.
Privacy and Security

A New York Health + Hospitals IT employee is arrested for using the hospital’s computer and network to download child pornography. Daniel Sherlock, 28, is on probation from a similar 2015 case in which he pleaded guilty. The conditions of that case prevented him from owning a computer, he told authorities, so he used his HHC one instead. He avoided registering as a sex offender in the previous case because his low IQ classified him as intellectually disabled, a situation that apparently did not prevent him from holding a $62,000 corporate account management job at HHC.
Other

A Politico report quoting a single source claims that Epic CEO Judy Faulkner told Vice-President Joe Biden at a private January 2017 Cancer Moonshot meeting, “Why do you want your medical records? They’re 1,000 pages, of which you understand 10,” to which Biden was reported to have responded, “None of your business. If I need to, I’ll find someone to explain them to me and, by the way, I will understand a lot more than you think I do.” The source was Greg Simon, now president of the Biden Cancer Initiative and a cancer survivor. Politico’s source material was apparently this video from Simon’s fireside chat at MedCity Converge conference this week in Philadelphia. I transcribed his full comments from the video:
I think everybody here is familiar with the problem with EHR companies, which is they’re billing systems, and yet we rely on them to track doctors’ visits, our treatments, our outcomes. But they’ve never been designed to be patient friendly. They’ve never been designed to be shared. They’ve never been designed to be interactive with other systems.
The EMR companies blame all that on their customers, the hospitals primarily, and large provider networks, and they have some guilt here as well. But the Cures act that passed in December requires data from electronic medical records to be shared in a digital, longitudinal way that can be used by patients.
When we had a meeting just before we left the White House with several EMR companies, hospitals, and others, we had, as they say in the State Department, a candid exchange. The head of a company that won’t be named – Epic – said to Vice President Biden – I should have sold tickets to this part – “Why do you want your medical records? They’re 1,000 pages, of which you understand 10.” So Biden said what I knew he would say, “None of your business. If I want to nail them to the walls of my kitchen, that’s my business. I don’t have to understand 1,000 pages. I want my records. If I need to, I’ll find someone to explain them to me, and by the way, I’ll understand a lot more than you think I do because people with cancer and their families and their friends and themselves learn a lot. So don’t make assumptions.” And it went downhill from there …
How can I as patient make better use of my medical records than having them sit in my doctor’s office? … if your financial advisor says, “Why do you want your statement?” run to the nearest police station .. we did spend tens of billions of dollars to encourage people to buy their products and we made billionaires of the executives of these companies. They’ve had fun – now it’s our turn.
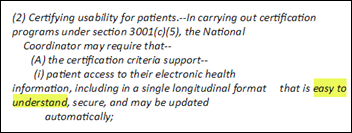
An Epic spokesperson sent me this response to the Politico article:
The recount of a portion of the January 2017 White House meeting is inaccurate and misleading. Vice President Joe Biden was consistently polite and positive to every person, including every vendor, in the meeting. Epic supports patients’ rights to access their entire record, something they have been able to do for decades. In the meeting, Judy raised an issue regarding the 21st Century Cures Act that would potentially require a patient’s EHR information be transmitted in a way that was “easy to understand.” She said that a requirement to translate EHR medical terminology into patient-friendly language could be a barrier to getting the medical record out to patients. Vice President Biden agreed, saying, “That’s actionable” and requested that one of his staff get the requirement fixed.

A fascinating Bloomberg article profiles the 20-something brothers from rural Ireland who started credit card processing Stripe and built it into a company worth $9 billion and made themselves billionaires. The company just announced a deal in which it will process some of Amazon’s transactions in its goal to “increase the GDP of the Internet” and expanding its product line to help businesses incorporate, pay workers, and detect fraud so that “two people in a garage [will have] the same infrastructure as a 100,000-person corporation.” The frugal brothers moved the company into San Francisco office space previously occupied by Dropbox, immediately getting rid of the Lego room, sofa swings, and gourmet meals cooked to order, explaining, “It’s slow and indulgent to wait for food.” One of the brothers keeps a countdown clock on the wall that estimates how much time he has left to live, explaining, “When you talk to people who are old, some wish they had enjoyed themselves more, but not many wish they had wasted more time … It’s not that I don’t enjoy TV. If I had infinite time, I would watch it. This might be the entirely wrong optimization.” It’s Atlas division offers a startup toolkit that provides Delaware incorporation, a bank account, a Stripe account, and both free and discounted professional advice.
Ireland’s Healh Services Executive warns physicians that a bug in its image archive omits the less than symbol (<), so that reviewing a result that lists stenosis as “<50 per cent” would be displayed as “50 per cent.” At least 25,000 images are affected. The HSE CIO resigned right after the story ran, but HSE says his departure is not related to the glitch.

Hurley Medical Center (MI) will identify patients with food insecurity via two EHR questions, with positive responses generating a referral to the hospital’s food pharmacy that will dispense a two-day supply of healthy food. The hospital hopes to provide assistance to its Flint patients who don’t necessarily live in poverty, but whose financial circumstances may require them to choose between buying medications and buying food.
In England, a Business Insider investigative article finds that Google-owned DeepMind has paid Moorfields Eye Hospital $144,000 in expense reimbursement in a project to apply artificial intelligence to optical coherence tomography scans, hoping to automate the early detection of diabetes-related macular degeneration. The hospital performs 3,000 of the tests each week.
Sponsor Updates
- ROI Healthcare Solutions is sponsoring the RocketShot 5K on August 12 in Roswell, GA.
- Learn on Demand Systems CEO and Chief Product Architect Corey Hynes receives the Microsoft Most Valuable Professional Award.
- Inc. profiles Logicworks CEO Ken Ziegler.
- Forrester names Salesforce Health Cloud a leader in its latest report on enterprise health clouds.
- MedData and Experian Health will exhibit at the HFMA Region 8 – MidAmerican Summer Institute August 7-9 in Kansas City, MO.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne, Lt. Dan.
Get HIStalk updates. Send news or rumors.
Contact us.






















































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…