Top News

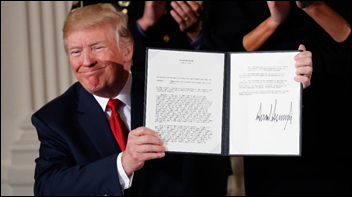
Senators Lamar Alexander (R-TN) and Patty Murray (D-WA) release their bipartisan plan to stabilize the health insurance exchanges in the short term. It quickly earned President Trump’s blessing “to get us over this immediate hump.”
Reported terms of the plan, announcement of which without specific draft language sent healthcare stocks flying on Tuesday, include:
- Payment of the ACA cost-sharing reductions that the President just ordered to be stopped would be reinstated for two years.
- $100 million of ACA sign-up assistance would be restored.
- The waiver process for states that want to customize ACA rules would be simplified.
- The availability of high-deductible, less-expensive policies would be expanded to all ACA enrollees, not just those under 30 years of age.
Vocal ACA supporter Andy Slavitt, former CMS acting administrator, is a fan of the Murray-Alexander proposal (even though he frets that it won’t get passed or that Senate Republicans won’t stop their quest to repeal the ACA entirely) since it would:
- Preserve the ACA.
- Reverse some of the White House’s ACA “sabotage.”
- Provide new affordable plan options that, while not for everyone, are still better than no insurance.
- Bring healthier people into the market.
- Give states the flexibility they have been demanding while protecting lower income and sicker populations.
Reader Comments

From Lingua Frank: “Re: grammatical errors. I recently heard a cyberscurity expert talking about ‘security tenants,’ which I assume was supposed to be ‘tenets.’ An HIT project manager described dividing a project into ‘epics’ instead of ‘epochs.’” I was about to rail about colleges that graduate students who are poor writers, but I realized that the real culprit is a culture that accepts poor grammar and writing, as well as sloppy presenters and writers who indignantly insist that we stop grammar Nazi-ing them and instead serve as their auto-correct by proxy. Facebook has taught me to immediately stop reading posts from people I don’t know personally that feature misspelled words or hideously bad grammar since I have to assume that the person is equally lazy in their logic and execution. We all make mistakes, but only some of us care enough to fix them. I’m not as militant about mistakes like these two examples since it’s easy to misuse similar-sounding words especially when you hear them more often than you read them, and if you don’t know the difference between the words, no amount of spell-check will help.
From Peony: “Re: Allscripts. The press release mangles the name of their new customer, Catholic Medical Center.” Indeed it does, but at least only after listing the name correctly six times. “Care Medical Center” is actually a pretty good name.
HIStalk Announcements and Requests

I was curious about the five-year share price performance of some of the publicly traded health IT vendors. Buying Cerner or Athenahealth would have earned you a five-year return of around 85 percent, while Allscripts and Quality Systems were dead money and buying CPSI would have lost you 40 percent over five years. With 20-20 hindsight, you would have passed on these and instead bought index funds for the S&P 500 (up 78 percent) or the Nasdaq (up 120 percent), both of which provided great returns without the white-knuckle share price rollercoaster thrills along the way. Click the chart above to enlarge.
Listening: new from Mostly Autumn, an English progressive rock band (Pink Floyd-ish at times) formed in 1995 mostly known for near-constant touring, not signing with a big record label, and having a considerable turnover of personnel that has necessarily changed their sound over time. YouTube made a good related suggestion in 4th Labyrinth, which in addition to playing decent pop-tinged prog rock, has one of the most mesmerizing bass players you’ll ever see in Claudia McKenzie (they do a nice cover of “Locomotive Breath.”)
Webinars
October 19 (Thursday) noon ET. “Understanding Enterprise Health Clouds with Forrester: What can they do for you, and how do you choose the right one?” Sponsored by: Salesforce. Presenters: Joshua Newman, MD, chief medical officer, Salesforce; Kate McCarthy, senior analyst, Forrester. McCarthy will demystify industry solutions while offering insights from her recent Forrester report on enterprise health clouds. Newman and customers from leading healthcare organizations will share insights on how they drive efficiencies, manage patient and member journeys, and connect the entire healthcare ecosystem on the Salesforce platform.
October 24 (Tuesday) 1:00 ET. “Improve Care and Save Clinician Time by Streamlining Specialty Drug Prescribing.” Sponsored by: ZappRx. Presenter: Jeremy Feldman, MD, director, pulmonary hypertension and advanced lung disease program and medical director of research, Arizona Pulmonary Specialists. Clinicians spend an average of 20 minutes to prescribe a single specialty drug and untold extra hours each month completing prior authorization (PA) paperwork to get patients the medications they need. This webinar will describe how Arizona Pulmonary Specialists automated the inefficient specialty drug ordering process to improve patient care while saving its clinicians time.
October 25 (Wednesday) 1:00 ET. “Delivering the Healthcare Pricing Transparency that Consumers are Demanding.” Sponsored by: Health Catalyst. Presenter: Gene Thompson, director, Health City Cayman Islands. Health systems are unlike every other major consumer category in not providing upfront pricing information. Learn how one health system has developed predictable, transparent bundled pricing for most major specialties. Attendees will gain insight into the importance of their quality measures and their use of actual daily procedure costing rather than allocated costs. They will also learn about the strategic risk of other market participants competing with single bundled pricing. The organization’s director will expand how its years-long process is enabling healthcare delivery reform.
October 26 (Thursday) 2:00 ET. “Is your EHR limiting your success in value-based care?” Sponsored by: Philips Wellcentive. Presenters: Lindsey Bates, market director of compliance, Philips Wellcentive; Greg Fulton, industry and public policy lead, Philips Wellcentive. No single technology solution will solve every problem, so ensuring you select the ones most aligned to meet your strategic goals can be the difference between thriving or merely surviving. From quality reporting to analytics to measures building, developing a comprehensive healthcare strategy that will support your journey in population health and value-base care programs is the foundation of success. Join Philips Wellcentive for our upcoming interactive webinar, where we’ll help you evolve ahead of the industry, setting the right strategic goals and getting the most out of your technology solutions.
November 8 (Wednesday) 1:00 ET. “How Clinically Integrated Networks Can Overcome the Technical Challenges to Data-Sharing.” Sponsored by: Liaison Technologies. Presenters: Dominick Mack, MD, executive medical director, Georgia Health Information Technology Extension Center and Georgia Health Connect, director, National Center for Primary Care, and associate professor, Morehouse School of Medicine; Gary Palgon, VP of healthcare and life sciences solutions, Liaison Technologies. This webinar will describe how Georgia Heath Connect connects clinically integrated networks to hospitals and small and rural practices, helping providers in medically underserved communities meet MACRA requirements by providing technology, technology support, and education that accelerates regulatory compliance and improves outcomes.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock

CNBC reports that Apple was recently considering acquiring its on-site medical clinic operator Crossover Health or national primary care clinic One Medical, although the sources did not indicate whether Apple’s interest was in running health clinics (which would be huge mistake and one that Apple is too smart to make) or partnering with them in an unstated technology role. The article describes Crossover Health as a startup, which might stretch the term since the venture-backed company was founded in 2006 by Medsphere co-founder Scott Shreeve, MD after Medsphere bizarrely fired and sued him and his Medsphere co-founder brother Steve for publicly releasing source code, an odd move for an open source software vendor. Crossover Health has raised $114 million, runs four locations in Silicon Valley and one in New York City, and Scott remains as CEO, which I think takes it beyond the “startup” label.
Non-profit accelerator BioEnterprise Corp.will take over management of Cleveland’s county-owned, money-losing Global Center for Health Innovation. The building, which is attached to a convention center, changed its name from the less-sexy Medical Mart before it opened to a collective yawn in 2013. HIMSS signed on early as the anchor tenant.
Eye Care Leaders, which sells EHR/PM for ophthalmologists and optometrists, acquires competitor IMedicWare.
Sales

Adventist Health System will implement Glytec’s EGlycemic Management System at 39 of its hospitals.

Three hospitals in Belgium choose Cerner Millennium, although the company already announced University Hospital of Antwerp early this year.
CVS – whose MinuteClinic and specialty care management programs use Epic — will implement Epic’s Healthy Planet population health and analytics platform to give prescribers point-of-care information about drug formulary status, suggest lower-cost alternatives, and perform electronic prior authorization. The integration will also send a patient’s non-prescription drug purchases made via digital store front to their record in Epic’s EHR .
China-based Internet technology vendor Tencent – whose messaging apps are used by two-thirds of China’s population – will offer its users evidence-based consumer healthcare information from Healthwise that it calls “the best health information in the world.”

Catholic Medical Center (NH) will implement Allscripts CareInMotion for population health management.
Announcements and Implementations

The American Medical Association launches its Integrated Health Model Initiative that will attempt to create a physician-developed holistic common data model around topics such as function, state, and goal to apply medical knowledge and improve interoperability. Initial communities are hypertension management, diabetes prevention, asthma functional status and patient goals, and defining wellness. Collaborators include AAFP, the American Heart Associaation, AMIA, Apertiva, BioReference Laboratories, CareCloud, Cerner, Clinical Architecture, IBM, Intermountain Healthcare, PCORI, PCPI, Prometheus Research, and SNOMED International. The announcement contained a lot of vague, lofty statements, so what AMA will actually do is not obvious.
Bernoulli Health will expand into Canada to offer its device integration, continuous monitoring, and clinical surveillance solution.

Healthgrades publishes its 2018 analysis of the top quality US hospitals and its “Report to the Nation.” It finds that if all hospitals performed as well as its five-star hospitals, 220,000 lives would be saved each year. Also released is the company’s National Health Index that lists the country’s 25 healthiest cities, with Minneapolis-St. Paul, Denver, Sacramento, Cincinnati, and Portland, OR taking the top five spots.

Voalte and Lightning Bolt Solutions will integrate their respective caregiver communications and hospital physician scheduling systems.
Government and Politics

President Trump declares in a Monday cabinet meeting that the term Obamacare is obsolete, explaining, “Obamacare is finished. It’s dead. It’s gone. It’s no longer. You shouldn’t even mention it. It’s gone. There is no such thing as Obamacare any more.” I’ll take all wagers that the President himself will tweet that term within a few weeks in trying to blame someone else for the inevitable “Trumpcare” meltdown.
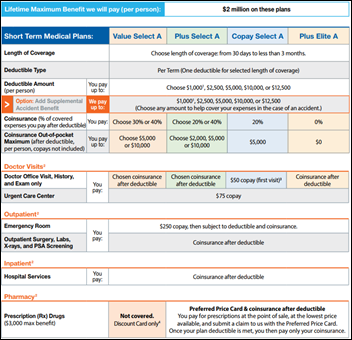
Meanwhile, UnitedHealth Group says it’s excited about selling short-term medical plans again per the President’s executive order that extends their maximum coverage period from three months to one year. Investors loved the company’s reaction, which probably means prospective customers should be wary given the history of those policies excluding of pre-existing conditions (even if the insured person doesn’t know about them) and generating consumer complaints and lawsuits.

Politico reports that Seema Verma and Scott Gottlieb have fallen off President Trump’s short list to replace Tom Price as HHS secretary, with the frontrunner now being Alex Azar, a former HHS deputy secretary (basically HHS’s COO) who ran drug maker Lilly’s US operations until he left the company in January.
Three New York City doctors are sentenced to two years in prison for accepting cash, strip club tabs, and sex acts in exchange for referring patient blood samples to a private New Jersey lab company. Fifty people have been convicted so far, 36 of them doctors, for a bribery scheme run by Biodiagnostic Laboratory Services that improperly steered $100 million in Medicare and insurance payments to the company.
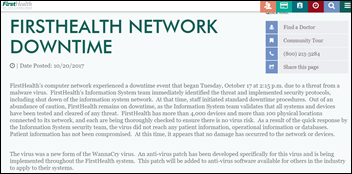
Privacy and Security

Chase Brexton Health Care (MD) notifies 17,000 patients that four of its employees fell for a phishing scam by filling out a phony email survey that gave hackers access to their email accounts. The hacker re-routed the paychecks of those employees to their own bank account. In terms of exposed PHI, the FQHC said the employee email accounts contained a lot of it that triggered the breach notice, but didn’t explain further.
Other

Venture capitalist Vinod Khosla famously said years ago that computers would replace doctors, which I thought was arrogant, clueless blather until I read this new interview with him that goes beyond the sound bite in elaborating on his thought process. Snips:
- [On why he said we need algorithms rather than doctors] “I tore my ACL skiing … I did an MRI and I took it to three different docs and they recommended three different things. I said, this is stupid. There’s one right answer. When I talked to them about probability, they didn’t understand probability, and these are really good docs.”
- “NNT (number needed to treat) is an incredibly important number that few doctors are aware of … If (medicine) was a science, for any given patient, you’d always have the same answer no matter who you ask, even if it is a probability distribution of outcomes. My goal became to change the practice of medicine, which is pretty damn good, into the science of medicine.”
- “We don’t even measure the stuff that doctors can’t directly understand. We’re starting to run into this a little bit because in genomics, you might get 1,000 data points and no doctor can look at 1,000 data points. So in the past, we didn’t measure anything humans couldn’t consume, which meant they can at best look at a few numbers. We should have thousands of numbers per patient, per episode.”
- “Anything that’s computing-based is near zero cost eventually. Which is why we spend way more compute cycles on a two-cent ad on Google than $10,000 medical decisions like, do you need a meniscus repair? … Let’s say you’re dealing with something serious like colon cancer. Does he know what each of the thousands of mutations could be? No, he doesn’t. So when he’s sitting down with the patient and saying, ‘You’ve got this cancer mutation,’ does he remember the 5,000 papers published in oncology journals recently? No, he doesn’t. He can’t.”
- “There’s a company in Israel called Zebra Medical Vision (note: Khosla is an investor in the company)… In India today, they are offering reading any image for a dollar. Now that’s impactful. There aren’t enough radiologists in India … you have the analysis done almost immediately, if you are connected, for a dollar .. we will see better results than a radiologist and way faster. Higher quality, faster, and dirt cheap. The radiologist couldn’t do a phone call for a dollar. What else do you need?”
- “There’s no reason an oncologist should be a human being. The right kind of oncologist isn’t the research oncologist. They know the most, but the guys who know how to take care of a patient are the community oncologists in Fresno or Stockton. They cannot always read all these journals, but they care for patients … They can be assisted with a virtual tumor board or an AI oncologist.”
- “Watson could do AI. IBM has the scientific talent to do AI, but they chose to package Watson and market it for what it wasn’t. I think they can do much more, but the early efforts have been less than successful because they over marketed its capabilities.”

A federal judge invalidates the expired patent of drug maker Allergan for dry-eye treatment drug Restasis, allowing the sale of generic products despite Allergan’s attempt to protect its patent by transferring it to an Native American tribe to shield it from administrative review. Allergan offered the St. Regis Mohawk Tribe $13.5 million upfront and $15 million per year as long as the tribe used its sovereign immunity to keep the patent intact, a tactic the judge slammed as a “scheme to evade their legal responsibility.”
Bloomberg reviews the history of short-term medical plans that would become legal to sell again under President Trump’s executive order, recalling that those policies generated a lot of patient lawsuits for refusing to cover the cost of pre-existing conditions. A woman bought a short-term policy to cover her between jobs, was diagnosed with breast cancer, and was left on the hook for the $400,000 treatment cost when the insurer refused to pay even though she wasn’t aware that she had cancer until after she signed up. An attorney of a patient whose insurer refused to pay for treatment of his newly diagnosed throat cancer said more insurance choices isn’t necessarily a good thing: “With insurance it, doesn’t work that way. You’ve got to put everyone in the same pot.” Everyone could save a fortune by buying barebones insurance (or none at all, for that matter) if only they had a functional crystal ball, but until that happens, health systems should assume they’ll be eating a lot more cost as patients who can’t afford the patient portion of their low-coverage insurance will still show up demanding care. My biggest frustrations in the insurance debate are: (a) lack of political will to look at provider and pharma costs means every solution is just another form of cost-shifting and rationing; and (b) politicians seem clueless about how insurance and charity care works in declaring that nobody should be forced to buy insurance they don’t need, raising the question of how they know they won’t need it or who pays for the care they will demand if they guess wrong.
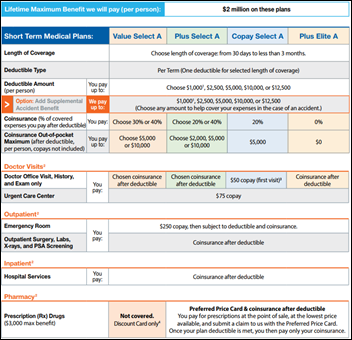
I ran a sample quote for United Healthcare’s short-term medical insurance, assuming a 40-year-old, non-smoking resident of Chicago under today’s underwriting policies. The company’s best Golden Rule-issued plan would cost $94 per month and would carry a $10,000 deductible, 60/40 co-insurance, 20 percent co-pay, and a $10,000 out-of-pocket maximum. The maximum lifetime coverage is $2 million. All payments, including ED and hospital, require the insured to pay the $10,000 deductible. No prescription benefit is included, nor is any out-of-network coverage at all (I would probably buy relatively inexpensive travel insurance with medical coverage while traveling on business or on vacation). Pre-existing conditions aren’t covered at all, defined as those for which the insured sought diagnosis or care in the previous 24 months or if the insured had symptoms for which “an ordinarily prudent person” would have sought care in the previous 12 months (at least you know upfront if that’s you). The price is great, you get United’s much-lower negotiated prices instead of paying provider list prices for cash, and people who can absorb the financial risk will be OK as long as they don’t get a new diagnosis of a chronic disease. Those with any existing or newly diagnosed chronic medical problems or who have less than $10,000 in liquid assets might not fare as well unless the ACA plans remain available so they can jump back in the next enrollment period (which isn’t really the way insurance is supposed to work).
EHR consultant Loretta Gallagher sues NYC Health + Hospitals, with a former IT director testifying that AVP Al Garofalo polled peers at a holiday party about which female consultant they would like to have sex with. The plaintiff sued NYC H+H last year, claiming her company was fired after she was refused to falsify a monthly Epic progress report as the CMIO ordered, although the health system’s OIG recommended her termination in 2015 after finding that her aunt – an HHC employee – improperly arranged to hire her and other family members.

Pretty funny.
Sponsor Updates
- Black Book names MModal the leading vendor in transcription technology solutions and services as well as a top industry disruptors and challenger.
- Spok welcomes 150 customers to its Connect 17 annual conference in New Orleans.
- Diameter Health posts a podcast titled “Quality Measures Past, Present, and Future.
- Meditech’s 6.1 and Client/Server EHR platform and portal earn Infoway’s certification for meeting standards in Canada.
- Ability Network announces the top-performing home health agencies in its annual HomeCare Elite program.
- Agfa Healthcare releases “Enterprise Imaging crosses The Tipping Point – Episode 1.”
- Aprima will exhibit at the Academy of Integrative Pain Management Annual Meeting October 19-21 in San Diego.
- Besler Consulting will present at the MAPAM Annual Fall Conference October 23 in South Yarmouth, MA.
- CarePort will exhibit at the Florida Association of ACOs annual conference October 19-20 in Orlando.
- Clinical Architecture joins the AMA’s new Integrated Health Model Initiative.
- The Jacksonville Business Journal recognizes CSI Healthcare IT CEO Rafe Sanson as a 2017 Ultimate CEO.
- Direct Consulting Associates and Dimensional Insight will exhibit at the HIMSS Midwest Fall Conference October 22-24 in Indianapolis.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne, Lt. Dan.
Get HIStalk updates. Send news or rumors.
Contact us.













![]()




































































It's nice when Epic takes on patent trolls and other bad actors in the industry. They do great when they…