HIStalk Interviews David Wenger, CEO, Bridge Connector
David Wenger is founder and CEO of Bridge Connector of Nashville, TN.

Tell me about yourself and the company.
I’m the founder and CEO of Bridge Connector. Bridge Connector is an integration platform as a service with a data-driven workflow automation solution. It is focused on solving the business workflow aspect of healthcare and creating interoperability between systems and ease of communication without the need for code. It is a truly scalable platform that provides an affordable solution to any sized healthcare organization so that they can streamline their business use case workflows.
It’s unusual for someone with no healthcare or IT background to be diving deep into the technical aspects of interoperability. How did that come about?
I grew up around the medical field. My dad’s a doctor, a businessman, and an entrepreneur. I watched him my entire life and learned from him about healthcare and why it’s broken. I’m an entrepreneur. I started a marketing and advertising agency about six years ago that focused on branding, marketing, web development, and cool tasks like that. It focused on helping smaller healthcare systems, drug rehabs, and behavioral health facilities with marketing to get customers in the door as well as keep customers or patients. I learned healthcare through that.
I saw a really big problem with one of my drug rehab clients. We were hired to integrate their Salesforce instance with their electronic medical record software. They were getting 150 phone calls a day and had a full team of people in their office typing the information manually from one system to the other. It was a 30- to 45-minute process per patient. I said, we can build this integration, and it took about six months.
After we built that first integration, I thought that there must be a faster way to do this, where any of these drug rehabs or smaller healthcare organizations could connect System A to System B without having a full team of people trying to build the integration on a custom basis or manually typing the information back and forth.
My father owns a surgical center under Envision Healthcare, which is a very large company. I spoke to people at the company and learned that this is a problem across all of their surgical centers and doctor’s offices. They have no way to get the data from the doctor’s office to the surgical center, or vice versa, without having to manually type the information back and forth.
I decided to do more research and build a proof of concept. I hired some smart developers and bootstrapped the whole thing out of my own pocket with some help from some friends and family. We built and deployed a fully-functioning, working prototype. We partnered with companies like Salesforce, for example, in taking this to the masses, focusing on smaller businesses at first and scaling it from there.
Systems can talk to each other in many ways — FHIR, APIs, app stores, and traditional vendor interfaces. What are the technical and business challenges in solving the interoperability problem?
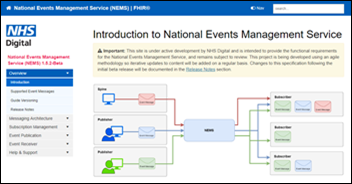
There’s a lot of standards out there, and a lot of companies that are stuck with the systems that they have. The solutions that are coming out are around API management or coding to specific APIs to build integration, so that developers have a tool they can easily use. We’ve taken a different approach. We have focused on meeting our customer at the spec their core system uses, whether it’s FHIR, HL7, API REST, SOAP, or a on-premise server solution.
We’ve created a way to connect to any type of standard and not make our customer have to code to any of those specs. We do it for them. Our platform is capable of digesting any of the types of information into one to make it a truly functioning integration. A solution like ours can go to the masses and be deployed to any type of healthcare organization, regardless of what system they’re using. As long as there’s a way to connect to that back-end system of truth or the other systems of truth, we have a way to do it, regardless of what standard they’re using.
What developments have you seen in making sure the information being exchanged makes sense to both sides and that it is inserted into the workflow at a point that makes it actionable instead of just making it available for a manual lookup?
We are focused on solving the business problems of healthcare. The problem in healthcare isn’t just clinical data. It isn’t just sending data back and forth. The problem is automating the business problem of healthcare. What drives physicians, what drives hospital organizations, isn’t just the money and patient care, but it’s automating the workflow so their daily processes can be as smooth as possible.
The government is saying to focus on interoperability. They’re trying to put a focus around it and develop it, making sure EMR companies or other vendors have fully-functioning APIs or FHIR standards. They are focused on trying to solve this problem. Companies like Bridge Connector and some of the other players out there are focused on building a standard that any sized system can easily connect to.
How do you work with traditionally low-technology, small-scale providers such as long-term care facilities and small medical practices?
We’ve partnered with the EHR companies in the long-term, post-acute care space. Their customers are requesting this type of integration and the ability to have their data flow easily. We partner at scale with a Salesforce, Clinical Care, or Brightree, for example, and provide a solution to all of their customers. The unique part about our platform is that once we build the connector or build an integration with one vendor, we’re able to rapidly deploy it again and again and again without the need for code.
Time to value, especially from a marketing brain, is everything. The faster you can go live, the better. The longer it takes, the more money the organization is losing. These smaller-sized facilities that aren’t at the leading edge of technology are trying to find ways to streamline their data so that they can solve their business workflow problem and then maximize their revenues by automation.
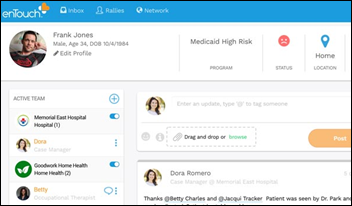
How does your social determinants of health functionality work?
We are launching our social determinants of health application. We’ve built a fully-functioning application on top of Salesforce. Anybody who owns Salesforce, such as a payer or large provider, can download this application that we’ve built — when it becomes available in the next month or so — and provide social determinants of health within their Salesforce org. They’re not only automating their workflow with integration and utilizing Salesforce to have all their customer data in one customer-centered place, but now they will be able to remove the barriers of care to their patients through this application that they can automatically deploy within their existing Salesforce org.
Salesforce made some healthcare-related announcements a couple of years ago, but I’m not clear what they are actually doing or who is using their product. How do you partner with them?
They are obviously a very, very fast-growing company. They have a significant interest in the healthcare space. They’re are doing a great job of providing value to the customers from a business perspective and automating that customer-patient view.
We partner with Salesforce to help the customers that they’re signing or customers that need integration. We partner with them to help automate those integrations and make them faster and make them easier to deploy, providing affordable solutions so that they can focus on what they need to focus on, which is obviously taking care of the patient.
Salesforce enables them to market to their patients and to schedule their patients. The functionality of Salesforce in healthcare is extremely impressive. We’ve been happy to partner with them and are excited to see where that goes.
What’s it like working with Salesforce, which was built on the concepts of openness and partnerships, compared to an EHR vendor?
Some EHR vendors have been slow to recognize that their customers want to be able to have the data flow as it needs to and to get the reporting that they need easily. The goal isn’t to take the data out of the EHR or make the EHR any less important to the healthcare organization. The EHR is important for the success of the business from a healthcare side as well as the patient.
The reputation of that openness of data is growing. EHR vendors are grasping the need and responding to what their customers are asking for, with integration and being able to have the data flow wherever it needs to. Obviously in keeping it secure and removing the identifiers and stuff like that. Salesforce is extremely secure. Bridge Connector is extremely secure, as well as the EHR. The core focus is taking care of the patient data and making sure it’s as protected as possible.
The company has grown quickly in headcount, customer count, and funding, but some see the healthcare IT market leveling off to some degree. How do you see that growth continuing and what will drive it?
We launched a year ago and we’ve raised $20 million so far. We had five people about 14 months ago and now we have 75 full-time employees. There’s such a need and so much customer demand for integration. Interoperability as a buzzword is more than just sending clinical data back and forth or patients having access to their medical records. The problems exist with the business use case. The markets that we’ve targeted, such as hospitals, are at the leading edge of technology.
We’re focused on the commercial space of healthcare. We are solving that business problem for those commercial vendors that can’t necessarily afford to spend money on a custom integration or developers building out integrations. They need is a rapidly deployable, affordable solution that generates immediate ROI.
We’ve grown so fast because of that, how we’ve partnered, and who we’ve partnered with. The overall need in the marketplace for a solution like what we have is driving our growth. Our growth is pretty astonishing to me, as someone who’s been here since the beginning and saw the idea and where it has taken us.
I think we are just getting started, to be honest. I think the growth will continue. We’ll continue to double in size. We’ll continue to rapidly increase revenues and customer counts and provide a solution that’s easily deployable to the masses over and over and over again, and at scale. We’re looking at hundreds of systems being rapidly deployable without the need for code over the next six to nine months. In healthcare, that solves a huge problem.
While the market might be leveling off a little bit, we think it will hit another inflection point in the next six months, where we will just continue to scale rapidly.
Do you have any final thoughts?
Healthcare is a semi-broken industry. Doctors need to focus on taking care of patients. A guy like my dad, for example, goes home every day after seeing 35-40 patients and types notes or does follow-up work on each patient. It’s an extremely draining task because of the need for notes or documentation, which are important, but there’s no way to easily do that.
The faster that the healthcare market allows for full interoperability or full connections between systems without EHRs getting in the way, from a API being available or charging customers lots of money to be able to have these integrations. As the market keeps growing, there will be a continuing need to connect systems, make the data actionable, and let the business automate workflows, Otherwise, the healthcare industry is not going to get fixed.
The way to fix it is to first solve the business problem, allowing System A, B, C, and D talk to each other. They can do that in every other industry in the world. Why can’t we do that in healthcare?
As a company that has grown as fast as we have, we feel that over the next year, we can help provide that solution to the masses. Not just hospitals, not just large enterprises, but to a small doctor’s office so their system can talk to other doctors’ offices, or have it talk to their billing system without having to go to their EHR vendor and paying thousands of dollars on top of the actual integration costs. The goal is to be able to deploy this to the entire healthcare market, not just the enterprise.



































I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…