Erine Gray, MPA is founder and CEO of Aunt Bertha of Austin, TX.

Tell me about yourself and the company.
Aunt Bertha focuses on the easiest way to connect people to health and human services programs through a simple interface. I experienced the need for this personally. My mom is permanently disabled. I have been her guardian for the last 17 years. Throughout this journey, I would find out about social programs after the fact. It was confusing to navigate.
I started the company nine years ago to offer an easier way to find programs and to connect to them directly and electronically. Some people call them referrals. We have 73 employees.
The concept of social determinants of health is suddenly popular, but for hospitals, it often just means having a place to record the patient’s self-reported information. Are they getting better at using that information to better transition their inpatients or ED patients to social organizations?
You’re right, there is a lot of talk about social determinants. It used to be called poverty and poverty alleviation. These are difficult problems to solve. The hospital system can do some things in many cases, but in a lot of them, they don’t have much control.
We have 175 customers, of which a good chunk are hospital systems. Many of them are just starting to record the assessments so they can at least uncover problems related to social care. Finding out if they need food or housing is a great place to start. They either turn on assessments in their EHR or they use our assessments.
That’s a great start, but some hospital systems that we’ve worked with have gone really deep. They have staffed social workers and teams who go the next mile and follow up with patients. In some cases, they actually buy wheelchair ramps, groceries, and other things if they find there’s a need.
I would say that the movement is still pretty early. It has been really neat to see how these hospital systems are experimenting.
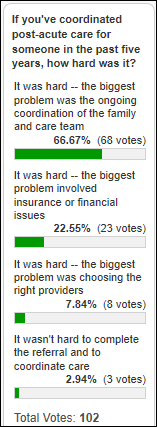
Is it hard for hospitals to make a quick, clean handoff to community-based organizations that aren’t necessarily equipped to respond quickly?
Absolutely. You still have the issue of non-profit financing. A community-based organization, or CBO, could be a government program or a social service program. Many of them are dealing with long waiting lists and a lack of funding, Some can’t serve their existing population. It is a challenge.
The question then becomes, what is the health system willing to do to engage them further, and, in some cases, to allow for reimbursement for some of these services? We are starting to see the sector think about it. CMS is starting to think about allowing for reimbursement for non-medical services beginning in 2020 for certain situations, if that service is deemed by a doctor to be medically necessary.
The short answer is that it depends. Organizations that sit down with the community-based organizations, get to know them, and build a partnership with them have seen higher levels of success under that model versus just hoping that an underfunded social care network can handle even more demand for services.
These are hard problems. Healthcare should assume longer-term commitments to these financing issues. I don’t think software is going to fix it, to be honest. Even though we’re a software company, I think the broader conversation is, how are the health systems and the local community-based organizations working together?
It’s interesting that 50 years ago, hospitals weren’t very much different from other community non-profits. Somehow their paths diverged and hospitals became monolithic and highly profitable, while most of the rest struggled for funding and hospitals quit talking to them in focusing on delivering episodic services.
You’re reminding me of the book “The Social Transformation of American Medicine: The Rise of a Sovereign Profession and the Making of a Vast Industry” by Paul Starr. It’s about how in the early days, people helped each other and how specialization within healthcare then happened. Your analogy is spot on. People did use to look after their neighbors a little bit more and there was tighter coordination. We’ve gotten away from that.
I entered the name of a remote, tiny town on your web page and it returned a list of 800 programs. It was nicely divided by the type of service and offered many simple but powerful ways to filter the list, mark favorites, make notes, and contact the organization. Your website says you have a large team manually maintaining that database versus other vendors who either unethically scrape your data or use a software bot to harvest information from the web. Why is it important to have humans doing the work?
It is incredibly important to us. If you put yourself in the shoes of a social worker or a doctor, they are sitting down with a patient and hearing about things that are happening in their lives. Maybe they need counseling, drug addiction help, or whatever the case may be. You learn very early on that the credibility of our users is on the line. The social worker is sitting down with a patient who is being vulnerable about their situation, which is hard enough. Referring to a program that doesn’t exist or that hasn’t been updated hurts the credibility of the social workers who are out there doing important work. We don’t always get it right, but we try really hard.
We determined early on that we wanted to build an operation of people for two reasons. One, because we think the product and the data will be better. That doesn’t mean we can’t automate some things along the way, and we’ve done some things to make those employees more efficient. But every listing is approved. We try hard to do this across the country, but we focus on states where we have customers and usage because we don’t have unlimited resources. That focus has allowed us to grow.
The team is 25 people and growing. That line item is one of the most expensive aspects of running the business. However, we’ve never spent any money on marketing or public relations. We’ve been able to get to know health systems, health plans, schools, foundations like AARP, and others just by providing a free search. We’ve started to get users that way. It has ended up being a good investment in the business in the long run.
Secondly, it’s a great way to find people in a growing organization. We’ve had many employees graduate from what we call the data fellows program, where they spend a year or two curating the data and verifying information. They become programmers, data analysts, and supervisors. We grow folks and get to know them. It’s a mutually trusted source. They end up doing great things with the rest of the organization.
It’s a win-win, the way we see it. There might be other approaches to maintaining a reliable database, but I don’t think they will win in the long run.
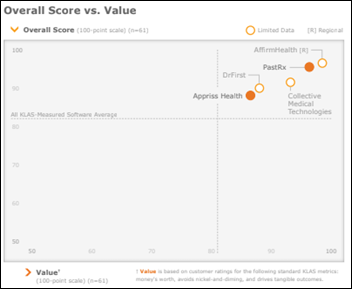
What is your revenue model and how does the community connection work?
We’re doing something different in healthcare. We try to make it simple. Smaller organizations can become a customer at a basic level, a professional level, or an enterprise level. We’ve learned that our customers don’t like seat licenses, per-user per-month models, or other models. We look at it differently than in classic health IT. We’re successful when we have thousands of customers out there paying us a modest amount. That de-risks us. If you are a health system, you can buy our enterprise version with a couple of add-ons at a set amount that is open, transparent, and explained on the website. That allows us to build trust with our prospects.
Once they become customers, we want lots of users. We don’t want to put anything in the way of that. The more users who are on the system, the more people who will get help and the more we’ll get our name out there. Our pricing follows models from outside health IT and it has worked well for us.
It’s also a lot more fun. We only have three salespeople and myself. When a sales team is getting 15 to 20 customers per quarter, they’re having fun. It’s an approach we feel really good about and our customers like that we keep it simple and transparent. This approach to pricing subsidizes the data operations team. We have been able to provide a free service at AuntBertha.com because we have enough customers to cover our costs.
Why is it important that you don’t require people to register before using your online service?
It’s understanding our users. We need to earn the trust of people who are in need, patients in the healthcare setting. We use the term “seeker,” which is basically anybody who is seeking services. Most people are not ready to identify themselves when they’re searching for help for their most intimate needs. Think of a breadwinner who loses their job. Maybe they’re not ready to identify themselves.
It’s an important principle that we allow people to look for things. We see what people are searching for. They are searching for sensitive situations, such as childhood trauma. They have the courage to at least search for help. We want to leave it as an opt-in situation because we build trust. Social workers who work in hospitals or community-based organizations also don’t like creating accounts, so we get their loyalty as users as well.
Once you start making referrals, you can identify yourself and make an account. But we are perfectly fine with users of AuntBertha.com and social workers who are using our platform to pick up the phone and call a non-profit directly instead. It’s perfectly their right to do so and we would not get in the way of that. But from a business perspective, that wins out in the long run and we get customers who want to opt in later.
How do you balance the company’s social mission as a public benefit corporation and your own advocacy work with running a business?
I don’t think they are conflicting. The trade-off in allowing for free users and that social mission side comes across during a deal cycle when we’re talking to hospital systems. Laying out what we’re about and what we’re trying to accomplish is a differentiator in that process. People can quickly tell the difference between an alternate approach that is on price maximization.
We are pretty close to break-even. Our growth and the number of potential prospects allow us to charge less, get lots of users, and still make a difference. We would not be getting into the doors that we’re getting into without the goodwill that we’ve built over the years by providing a free service.
Do you have any final thoughts?
I’m excited about the way healthcare finance is going. I’m certainly not an expert. I was a programmer by training. I worked in public policy with some state health programs. But what I see happening is that health plans and hospitals are starting to become interested in getting the basic needs of people met in non-healthcare or social care ways. They feel like it’s a win-win in the long run, for their government contracts if you’re a health plan, or under alternative payment models if you are a health system.
It’s an exciting time to watch this transformation happen. You’re starting to see teams being formed with the goal of, how can I interact with somebody in need at their moment of need? Could we as a health system or health plan solve that need by building a wheelchair ramp or getting them some groceries? It’s an amazing win-win. I don’t know what’s going to happen with government policy, but watching that is exciting.
Comments Off on HIStalk Interviews Erine Gray, CEO, Aunt Bertha







































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…