News 8/30/19
Top News
University Hospitals in Cleveland takes home a $1 million grant after winning the Ohio Opioid Technology Challenge.
The hospital’s innovation arm, UH Ventures, developed post-discharge software that helps providers assess a patient’s risk for opioid dependency, and keeps track of adherence to needed prescriptions as patients transition from hospital to home. A six-month pilot project of the UH Care Continues solution at a dozen UH hospitals kept 12,000 pills out of circulation.
UH CEO Tom Zenty says the award substantiates the health system’s decision to create UH Ventures, which launched in 2017 to help the system diversify its income stream.
Reader Comments

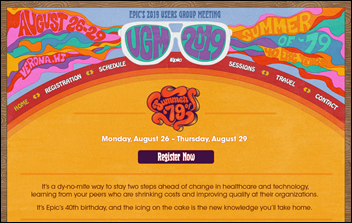
From UGMbracer: “Re. Epic Cosmos. Other sites mentioned its announcement this week at UGM. Why not HIStalk?” Because it’s not new. Epic’s Cosmos research network was first announced at the 2015 UGM, with the only news being that nine health systems have signed up since.
Webinars
September 5 (Thursday) 2:00 ET. “Driving 90% Patient Adoption Across Your Network: How US Dermatology Partners is Showing Us The Way.” Sponsor: Relatient. Presenters: Michele Perry, CEO, Relatient; Sara Nguyen, VP of applications and integrations, US Dermatology Partners. US Dermatology Partners is helping its physicians reclaim time they can spend with patients and is turning patient engagement strategies into business results across its 90 locations in eight states. Attendees will learn how US Dermatology Partners defined its patient engagement objectives and physician-optimized strategies. They presenters will provide advice on starting or accelerating patient engagement goals.
September 19 (Thursday) 2:00 ET. “ICD-10-CM 2020 Code Updates.” Sponsor: Intelligent Medical Objects. Presenters: June Bronnert, MSHI, RHIA, director of terminology mapping, IMO; Theresa Rihanek, MHA, RHIA, classification and intervention mapping lead, IMO; and Julie Glasgow, MD, senior clinical terminologist, IMO. The 2020 regulatory release is right around the corner. Join IMO’s top coding professionals and thought leaders as they discuss new, revised, and deleted codes; highlight revisions to ICD-10-CM index and tabular; discuss changes within Official Coding Guidelines; share potential impacts of the code set update; and review ICD-10-CM modifier changes.
September 26 (Thursday) 2 ET. “Patient Education Data: A Key Ingredient for Improving Quality and Patient Experience.” Sponsor: Healthwise. Presenters: Victoria L. Maisonneuve, MSN, RN, director of the Nursing Center for Excellence and Magnet program, Parkview Health; Marta Sylvia, MPH, senior manager of quality improvement and outcomes research, Healthwise. Healthcare data is everywhere! It’s scattered across various systems and in countless formats, making it difficult to collect and glean actionable information. Knowing where to start depends on what your organization wants to accomplish. Vicki Maisonneuve will share how her team analyzes data around the use of patient education. By combining different data sets, she can easily identify trends, gaps, and opportunities to improve quality and patient experience across Parkview Health.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Patient engagement vendor Luma Health raises $16 million in a Series B round led by PeakSpan Capital. The San Francisco-based company has raised $26 million since launching in 2015.

San Francisco-based life insurance startup Ethos raises $60 million in a Series C funding round led by Google Ventures. The company uses predictive analytics to determine an applicant’s life expectancy, and then offers up a best-fit policy after an application process that takes just minutes to complete. The technology, which verifies health histories against an applicant’s medical record, eliminates the need for most to undergo a medical exam, according to co-founder and CEO Peter Colis. “You shouldn’t have to endure what’s essentially a medical and financial strip search in order to protect your family,” he adds.
Rock Health founder Halle Tecco launches Natalist, a monthly subscription box company for women looking for clinically-validated products and resources to help them conceive. The company is taking a decidedly anti-Goop approach to its product line and marketing, assuring customers they won’t encounter “junk science” and explaining why they don’t carry products like fertility crystals and birth control cleanses.
People

Eric Dishman announces he will transition from head of the NIH’s All of Us research program to its chief innovation officer.

LogicStream Health names Luis Saldaña (Texas Health Resources) CMIO.
Sales
- The University of Tennessee Medical Center taps Gozio Health to develop its mobile wayfinding and patient engagement software.
Announcements and Implementations

In England, Gloucestershire Hospitals NHS Foundation Trust’s CIO says his organization is “one of the most digitally immature organizations in the health service” with primarily paper records, but it will implement Allscripts Sunrise while retaining its InterSystems TrakCare patient administration system in a “clinical wrap” approach that will move faster than implementing a new PAS first. Deployment started last month and go-live is planned for July 2020.

UC San Diego Health implements provider information management software from Phynd.

KLAS looks at Cerner’s revenue cycle improvement performance since an August 2018 big-hospital customer roundtable. Most participants say their relationship with the company has improved and two-thirds believe that RCM is a top Cerner priority, but 88% are not satisfied with tangible results in the year since the meeting and 56% can’t name a single delivered Cerner win. The top confidence-inspiring action by Cerner was making leadership changes. The biggest client concerns are Cerner’s ability to execute and its sense of urgency in proposing a multi-year roadmap.
Privacy and Security

The National Institute of Standards and Technology seeks vendor insight and demonstrations of cybersecurity solutions for telehealth. The project will help NIST’s National Cybersecurity Center of Excellence develop a Cybersecurity Practice Guide for providers and vendors.

ProPublica looks at the ways in which insurance companies are helping to perpetuate ransomware attacks on local governments and private businesses, noting that the FBI has even said that hackers are now targeting American companies that they know have cyber insurance. At the end of the day, the bottom line tends to trump moral outrage: “Paying the ransom [is] a lot cheaper for the insurer. Cyber insurance is what’s keeping ransomware alive today. It’s a perverted relationship. They will pay anything, as long as it is cheaper than the loss of revenue they have to cover otherwise.”
Other

The next iteration of Fitbit’s Versa smartwatch will feature Amazon Alexa integration and access to the company’s new monthly subscription service that will provide a deeper dive into user health stats. Access to health coaches will be available for an additional fee later this year.

The Atlantic highlights the strange ways in which medical debt collectors attempt to reach patients burdened with bills they’ve been unable to pay – some incurred by out-of-network providers brought in while patients were unconscious. A particularly creepy collector even went so far as to send a LinkedIn request to heart transplant recipient Joclyn Krevat, who remembers thinking, “Is this lady stalking me or does she really think we’d be good in each others’ professional networks?“
Sponsor Updates

- Definitive Healthcare raises and donates nearly $130,000 to fund cancer research at its fourth annual Jimmy Fund Golf Tournament.
- EClinicalWorks will exhibit at CASA 2019 Annual Conference & Exhibits September 4-6 in Monterey, CA.
- HealthCrowd and InterSystems will exhibit at the Florida Association of Health Plans 2019 Annual Conference September 4-6 in Orlando.
- Google Cloud will work with NTT Data Services to develop and deliver digital offerings in cloud, analytics, and AI to help providers and payers improve the patient experience.
- Vocera adds Imprivata’s authentication capabilities to its Collaboration Suite of shared clinical mobile devices and smartphone app.
- The Medicaid Black Book gives Collective Medical a five out of five star rating in an overall assessment for Medicaid effectiveness.
- Greenway Health congratulates customer Health Choice Network on its 2019 Quality Improvement Awards from HRSA.
- Redox offers free support to customers who access patient data via the USCDI functionality on the FHIR standard.
Blog Posts
- The Rise and Importance of Telemedicine (EClinicalWorks)
- 6 Considerations When Preparing for EHR Billing Cycle Support (Optimum Healthcare IT)
- Clear Patient Assignment Methodology: The Fourth Attribute in a Modern Care Management Model (Ensocare)
- How to set up a new Chromebook (Google Cloud)
- 22 ways to promote patient portal use and increase patient engagement (Greenway Health)
- The Drought is Over: It’s Raining Health IT IPOs (Healthcare Growth Partners)
- Mergers & Acquisitions: Don’t Lose Sight of Culture (Impact Advisors)
- Improving coordinated labor and delivery care for mothers and babies (Meditech)
- Cultivating the next generation of leaders through the Imprivata Leadership Development Program (Imprivata)
- Legacy Clinical Data Archiving: Beyond a Historical Patient Snapshot (InterSystems)
- Putting Providers at the Forefront of Access: Learnings from Prisma Health (Kyruus)
- Nordic’s 2019 Open House Recap (Nordic)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.


































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…