EPtalk by Dr. Jayne 2/9/23
Mr. H’s current poll asks about the methods used by patients to send medical information to clinicians in the past year. I wasn’t surprised to see that patient portal messages are leading the way, followed by phone calls and electronic forms. Mailed paper forms and faxes are at the bottom of the list, as expected.
It would be interesting to see a poll around the topic of “In which ways have you had productive communication and/or a positive outcome” when looking at electronic communication and portal messages. I recently tried to use the online scheduling feature offered by my dermatologist, with whom I am well established. There were no spots available until June, so I used the feature located on the online scheduling page called “request an appointment.” I mentioned that the request was to be seen for a suspicious and changing mole that had already been seen by my PCP, who recommended I see dermatology. I listed my preferred days and times, but basically said that due to the nature of the issue, I was willing to take any open appointment.
Four days later, I received a portal message back that “we are not currently offering online appointment requests” and was directed to call the academic medical center’s access center. If you’re not offering online appointment requests, I might recommend disabling that feature so that patients can’t use it. I’ve used the access center before to request an appointment with this dermatologist and it’s a centralized scheduling nightmare. For urgent issues, they take a message and route it to the office who hopefully calls you, and then if you’re like me and tied up on calls and in meetings all day, you play phone tag, which is exactly what the online requests are supposed to prevent.
I mentally said, “forget it” and made an appointment with a new dermatologist who was happy to get me in within 48 hours given the history and PCP referral. Since my clinical issue was resolved, we will see if my original dermatologist ever follows up, who now has a concerning message documented in my chart. We are going on six weeks so I’m not holding my breath, but for a patient who isn’t as persistent in getting care, it could be tragic.
From Jimmy the Greek: “Re: chatter about using ChatGPT in healthcare. It might amount to the scene out of ‘A Charlie Brown Christmas’ where Lucy is listing off phobias and asking Charlie Brown if he has them.” I’ve certainly seen some interesting applications, or should I say attempted applications, of ChatGPT recently. Today brought an email from a colleague that was most likely produced by some sort of bot since the syntax didn’t sound anything like her usual written patterns. I found it pretty annoying since what she sent was a reply to a pretty straightforward question that could have been answered in five words or fewer. It’s fine if you want to play around with it, and since we are both informaticists, it could have been “hey, check out what ChatGPT created as a reply,” but since there had to be a few more back-and-forths to get the original question answered, it wasn’t much of a time saver.
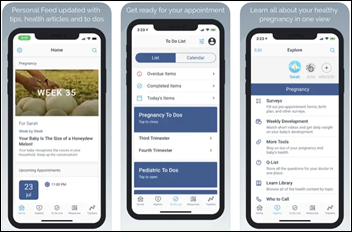
Everyone is trying to figure out how to streamline workflows in ambulatory medical practices. Solutions being implemented for pre-visit flows include patient portal-based check-in that can be completed at home up to a few days prior to the visit; chatbot-based flows that can be completed either at home or upon arrival; and self-check-in kiosks. A recent article in the Annals of Family Medicine looked at a “self-rooming” process implemented in primary care clinics from October through December 2020. Researchers found that most patients preferred self-rooming, although some felt less welcomed, more lost or confused, more frustrated, or more isolated compared to escorted rooming.
Based on the overall positive response, the organization decided to roll out the process to all remaining primary care clinics, and it will become a permanent change for the institution. The process design included some decidedly low-tech features, such a laminated wayfinding card that was used by the patient to reach their exam room. Once the visit was over and the room had been cleaned and prepared for the next patient, the card was returned to the front desk so that another patient could be directed to the newly prepared room.
I recently learned that my residency training program is celebrating its 50th anniversary and will be holding a gala in honor of the milestone. Unfortunately, they didn’t start promoting the event until 60 days out, which isn’t nearly enough lead time when you consider that most of us open our clinic schedules up to a year in advance and on-call schedules are done at least 90 days in advance. I circulated the information to my class and the residents in the years above and below mine, but it looks like only the handful of folks who can travel without taking off work are likely to attend.
I had no idea the program had reached such a major milestone and it really seems like a missed opportunity to bring people together. Other organizations I’m part of that have had similar events have sent cards anywhere from six months to a year in advance telling people to save the date, which is key if you want to try to get a couple hundred physicians together in the same place at the same time.
It’s technology upgrade time at the House of Jayne and I’m very happy about my first purchase, which was a Kindle Paperwhite. I’ve been using the Kindle app to read on a decade-old iPad and decided I wanted something smaller and lighter for travel. Amazon was offering a deal on the high-end version as long as you didn’t mind buying it in Agave Green. I’m thrilled with the purchase and have already burned through two books. I’m still getting to know all the features, but it’s a significant step up from my previous reading situation.
I also had to break down and replace one of my monitors, which started having some issues with static electricity. Every time I touched my keyboard tray after walking on the carpet and accumulating a charge, the monitor would suffer a blue screen of death that required a reboot to bring it back to life. Tomorrow is unboxing and installation day, so wish me luck as I crawl around and under the desk to get things hooked up. Still on the to-do list after that is a new phone, but that’s a much larger project, especially since I want a full featured Android device that’s on the smaller side.
What’s your favorite piece of new technology? What’s the one thing you’d recommend everyone consider getting? Leave a comment or email me.

Email Dr. Jayne.






































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…