News 3/1/23
Top News

Cerebral announces its third round of layoffs in the past few months as the beleaguered direct-to-consumer telemedicine company attempts to reorganize and streamline its services.
Cerebral has struggled since the federal government launched an investigation of its prescribing practices for mental health issues, especially its heavily promoted prescribing of Adderall.
Cerebral’s valuation reached nearly $5 billion just over a year ago.
Reader Comments

From Pete Drucker; “Re: Quil Health. To exit the market, with the last day for employees being February 10 and for executives February 24.” This was sent to me on February 7, but I didn’t mention the company’s name pending verification. Quil’s web page has been taken down and CEO Carina Edwards has updated her LinkedIn with a February 2023 end date and references to the company changed to past tense. Philadelphia-based Quil was formed in 2019 as a joint venture between Independence Health Group and Comcast, offering medical alert and monitoring tools to support care-at-home for seniors. I interviewed Carina Edwards 10 months ago.
From Plural Effusion: “Re: plural words. I see examples daily where someone sticks in an unneeded apostrophe.” Plurals shouldn’t have apostrophes except for one-letter items, such as the Oakland A’s or minding your p’s and q’s.
From You Interviewed Me: “Re: my HIStalk interview. It received lots of attention. You have certainly built an engaged group of readers.” Thanks to this CEO for giving me a rare post-interview report. I’m always up for talking to CIOs, clinician executives, frontline people, or anyone who would be interesting to readers who comes from the non-vendor side of the table. If that’s you and you can spare 30 minutes for a call, let me know.
From Pshaw: “Re: attrition goals. Epic in a nutshell.” Former Amazon managers say that the company meets its attrition goals by rating decent performers as not meeting its expectations. The company refers its “unregretted attrition rate,” where it expects managers to rank 5% of employees in the lowest tier that the company wouldn’t mine losing, voluntarily or otherwise. Amazon replaces a set percentage of less-performing employees annually. UPDATE: I’m changing this since while I was thinking that Epic stack ranks employees and I thought I read long ago that the company’s philosophy was to intentionally replace the bottom tier, I’m not sure that employees in that tier are fired. Perhaps some who works at Epic can elaborate further.
HIStalk Announcements and Requests
HIStalk sponsors benefit from being listed in our guide to major conferences, which provides on-site details for those that are exhibiting or attending so attendees can seek them out. Send me your ViVE 2023 information by Wednesday, March 15 to be included. The ViVE 2023 exhibit hall floor plan shows 169 exhibiting companies, with separate musical stages for pop, hip hop, bluegrass, classics, and country (the latter being the largest by far, which wouldn’t be a plus for me). Glancing down the exhibitor list, I see a few dozen HIStalk sponsors, so those remaining dozens are welcome to contact Lorre to extend their reach beyond occupying a small patch of carpet for a half week.
Speaking of ViVE, I just got an email saying that the Clearsense-sponsored industry night entertainment is the Black Crowes. Two perpetually feuding brothers are all that’s left of the original lineup that formed 40 years ago, also the only two who played on their monster 1990 album “Shake Your Money Maker” or on their last new album in 2009.
Webinars
March 7 (Tuesday) noon ET. “Prescribe RPA 2.0 to Treat Healthcare Worker Burnout.” Sponsor: Keysight Technologies. Presenters: Anne Foster, MS, technical consultant manager, Eggplant; Emily Yan, MPA, product marketing manager, Keysight Technologies. Half of US health systems plan to invest in robotic process automation by the end of this year, per Gartner. The concept is evolving to help with staff burnout and physician productivity. The presenters will introduce RPA 2.0, explain how to maximize its value, demonstrate how to quickly start on RPA 2.0 and test automation in one platform, and answer questions about healthcare automation.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Automated coding technology vendor CodaMetrix raises $55 million in a Series A funding round. The company was spun out of Mass General Brigham in 2019 and is led by former LifeImage CEO Hamid Tabatabaie.
Sales
- Baptist Memorial Health Care (TN) selects LookDeep Health’s Clinical Action Platform to enhance its inpatient video monitoring capabilities.
- Augusta University Health (GA) will expand its Virtual Care at Home program using technology from Biofourmis.
- Southwestern Health Resources (TX) selects referral management software from LeadingReach.
- Yale New Haven Health (CT) will implement RxLightning’s automated pharmacy workflow software.
- Sheffield Teaching Hospitals NHS Foundation Trust in England will replace its Dedalus EHR with Oracle Cerner’s Millenium software next year.
People

Engooden Health, the former Cohort Intelligence, names Tom Frosheiser, MBA (Nvolve) as CEO.

Dan Michelson, MBA joins 7wire Ventures as entrepreneur-in-residence, rejoining his former Allscripts executive colleagues Glen Tullman and Lee Shapiro. He was CEO of Strata Decision Technology through May 2022.

Leah Ray (Jvion) joins Linus Health as chief customer officer.

Chris Belmont, MBA (Memorial Hospital at Gulfport) joins Ochsner Health as SVP/CIO, a position he held from 2009 to 2013.
Announcements and Implementations
Southern Illinois Healthcare implements PocketHealth’s diagnostic image-sharing software for patients and providers.
NIH-funded researchers from Cleveland Clinic and MetroHealth will use digital twins, created from de-identified EHR data, to understand healthcare disparities based on living location.
A pre-print journal article finds that ChatGPT performs well in suggesting improvements to the logic of clinical decision support alerts.
Practice management software end users give EClinicalWorks, ModMed, NextGen, and Veradigm top customer satisfaction marks in Black Book’s latest annual survey.
Government and Politics

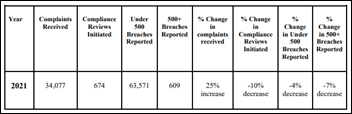
HHS OCR renames its Health Information Privacy Division to the Health Information Privacy, Data, and Cybersecurity Division as part of a reorganization that will better enable the office to more effectively respond to complaints. An OCR report published earlier this month pointed out that the office lacks the financial resources it needs to investigate HIPAA complaints and enforce penalties, both of which increased considerably between 2017 and 2021.
Privacy and Security
Researchers at Duke University’s public policy school find that since technology companies, app vendors, wearables manufacturers, and social media platforms aren’t covered by HIPAA, they are legally selling the health data of their users to data brokers without their knowledge or consent. The authors looked specifically at at mental health data:
- Some data brokers are offering user health data on the open market, with minimal vetting of customers and few stated limits on its use.
- Brokers don’t always make it clear whether their health data is de-identified, and some seem to imply that they are willing to provide identifiable data.
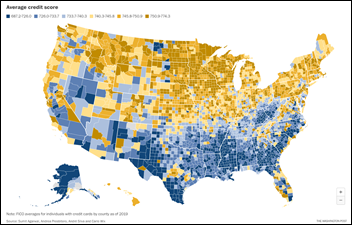
- The most active brokers offered data of people with depression, ADHD, insomnia, ADHD, and bipolar disorder that also included ethnicity, age, gender, ZIP code, religion, number of children living in the home, marital status, net worth, credit score, and data of birth.
Other
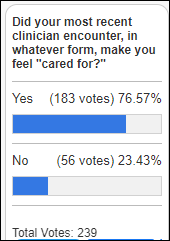
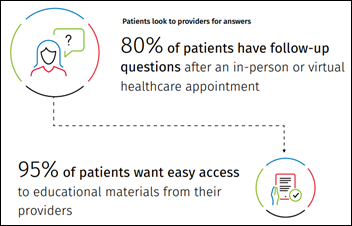
It’s not just doctors who are burned out, a Times article says, citing evidence that patients are being burned out by poor healthcare customer service that includes long appointment lead times, short visits, high prices, surprise bills, insurance aggravation, and too much focus on the EHR. Experts say to watch how patients vote with their feet as they flock to non-traditional settings that offer same-day appointments, walk-in visits, flat-rate memberships, and telehealth.
A Stat review of the boards of 15 top-ranked academic medical centers finds that 44% of board members come from the financial sector, while 13% are physicians and 1% are nurses. The authors conclude that board composition may explain why non-profit health systems focus on revenue instead of community need and employee satisfaction. They cite previous surveys showing that a big percentage of hospital board members are white males.
Sponsor Updates
- Ascom Americas gives Fairchild Communication Systems the ability to re-sell Ascom clinical workflow solutions in the additional market of Toledo, OH.
- Azara Healthcare and Bamboo Health will exhibit at Rise National March 6-8 in Colorado Springs.
- Availity will present and exhibit at State HIT Connect March 6-8 in Baltimore.
- Baker Tilly names Kat Mako (IMethods) and Cindy Kmiecik (Uniper) business development directors of healthcare IT.
- Bardavon Health Innovations partners with the Gray Institute to offer discounted CEUs to its BNotes customers.
- Biofourmis, Care.ai, Clearwater, EVisit, and Optum will exhibit at ATA 2023 March 4-6 in San Antonio.
- CTG publishes a new case study, “CTG Improves Gundersen’s Patient Portal Support with Amazon Connect.”
Blog Posts
- Survey: Your Practice is Losing Almost a Month to Financial Busy Work (AdvancedMD)
- Robotic Process Automation & Artificial Intelligence in Healthcare: Two Distinct Technologies with Distinct Benefits (AGS Health)
- Population health trends across the United States (Arcadia)
- Part 4: Supporting the Patient Experience with Pharmacy Technology (Arrive Health)
- We Must Dramatically Streamline Clinical Workflows: Here’s Why. (CareMesh)
- Voice of the Assessor (Censinet)
- Building a Unified EHR with Meditech Expanse: A Look Back at Key Decisions (CereCore)
- 7 Ways to Minimize Privacy Risk Created by Online Tracking Technologies (Clearwater)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.
























This is a great point—many discussions about patient wait times still focus on staffing or technology, while the real issue…