Submit your article of up to 500 words in length, subject to editing for clarity and brevity. Use your real or phony name (your choice). Submissions are subject to approval and become the property of HIStalk.
A Physician’s Experience with Kaiser’s Epic/HealthConnect Rollout
By Bernie Tupperman, MD
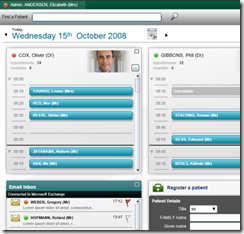
I am a Kaiser physician in Northern California and a user of HealthConnect (Kaiser’s implementation of Epic) for inpatient and outpatient records. Our medical center has used Epic’s outpatient software since early 2005. We recently went live with the inpatient EMR and operating room software. I read the HIStalk reports about Stanford’s physicians supposedly rebelling after their Epic rollout. I wanted to tell you informally about our experience.
Eight of our medical centers are live for inpatients in Northern California. Each rollout has been smoother and smoother. It takes proper preparation, the right education, and peer group help.
Preparation for an Epic inpatient implementation starts years in advance. In Northern California, central planning and coordination of support, educational web-based training, and training of regional physician and specialty staff is coordinated from a central headquarters in Emeryville, CA.
Each hospital is linked to Kaiser’s data centers across the country. Implementation of computer layout and wireless PC cart connections starts 18-24 months in advance: networks, computers, UPS power in closets, design of networks (vendors), review of construction and facilities, switches and access points… and testing.
Epic inpatient software is purchased off-the-shelf (inpatient, CPOE, Operating Room, Reports), but national and regional builds are created with the help of regional specialty groups and domain groups. A domain group is a local committee of multidisciplinary users who work in a specific area of the hospital, such as pharmacy, inpatient nursing, periop, etc. They make local policies, identify and solve problems, and develop workflows for their area.
The Epic inpatient modules were first rolled out in one medical center, where problems were ironed out and methods of implementation were tried out. Epic programmers worked with local physicians and team leads to troubleshoot the deployment and create training materials and customized "navigators" to guide physicians, nursing, and ancillary staff into a logical workflow, helping to smooth the interaction between Epic and the human users. Total time to troubleshoot was about a year and a half.
Things have worked so well that the pace of installation and rollout will be increased from one medical center every three months to one every month.
Medical centers going live on inpatient are required to already be live on the Epic outpatient EMR, preferably with several years’ of physician and staff experience. The inpatient and outpatient modules are similar in function and appearance, so that makes training easier.
Probably the most important resource Kaiser has developed to improve physician and nurse acceptance and training is the creation of Physician Clinical Experts (PCEs) and nursing Faculty Clinical Experts (FCEs). These are self-selected or nominated physician or nursing IT champions who are given time off for additional orientation in the inpatient modules and are given early access to training environments for practice. They are given the opportunity to attend a medical center go-live and are allowed to assist other staff in this time period. They get experience helping others use the software while being assisted by regional physician and nursing leads. The new physician follows an experienced physician and learns basic troubleshooting techniques and how to solve the most common problems.
Experienced specialty physicians who have regional support and appointments develop departmental connections with IT departmental champions and mentor them in preparing their department.These are frequently leaders who emerged from the early go-live department centers.
Four to five months before go-live, groups of physicians are begun on early adopter programs, allowing them to use limited inpatient charting tools. Web-based training is the primary method of instruction, but the physicians are free to use "sandbox" Web sites to get some familiarity with the system.

Early adopters primarily use Epic inpatient charting with special limited navigators, but orders are not placed at this time or accepted since there is no one to acknowledge them. Since these inpatient charts are still primarily paper, all notes written in the inpatient modules still have to be printed and placed in the chart. However, physicians have access to problem lists and special smart abbreviations to create history and physical exams, operative notes, discharge summaries, and, most importantly, complete patient discharge instructions that fulfill all regulatory requirements. Familiarity with the electronic charting and navigator use simplifies the steep learning curve and makes the conversion to the full inpatient modules easier.
Two to three months before a medical center go-live, all inpatient specialties are asked to take Web-based training covering the basic functionality of the inpatient Epic modules. This includes inpatient specialty physicians, nursing, pharmacy, ADT, interventional radiologists, and other inpatient support staff (clerical, respiratory services, physical therapy, discharge planning, and utilization services).
Three to four weeks before go-live, training starts in earnest. Groups of physicians work in a training environment in a computer lab, overseen by an instructor who runs through basic functionality using a pre-determined script. Most classes are small and supported with written customized manuals, additional computer support staff, and a physician IT champion or clinical expert with inpatient software experience. Questions that cannot be answered are logged and answers are provided afterwards.
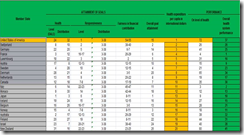
Teams of physicians and nurses are recruited from other medical centers to support a go-live. In addition to the Regional teams of leaders who have responsibility for the go-live, local teams are formed from admitting, pharmacy, nursing, radiology, dietary, biomedical engineering, IT, and programmer technical support. A reporting bridge is set up for reporting trouble; programmers are available 24 hours a day to test and fix software. A quality hub is set up for monitoring of all aspects of charting and ordering and all activity is monitored, including medication administration, discharge instructions, orders needing co-signing, pended notes and orders, prescriptions, discharge summaries, history/physicals, and more.
On go-live day, chart cutover begins early in the morning. Groups of staff from specialties and departments meet in conference rooms and receive their assignments, process, and schedules for the day. Between 15 and 30 teams of physicians and nurses are dispatched to every ward and await the signal to begin reviewing each chart and entering the patient’s paper orders into the electronic medical record. Cutover does not begin until the pharmacy, X-ray, and lab are ready to receive orders and process them.
Once the go-ahead is received, all orders are carefully scrutinized by physicians and entered into the electronic medical record. The chart is passed to one of several nurses on the team to enter the nursing flowsheets. The orders and flowsheets are verified with the patient’s nurse to be sure that everything is correct. Finally, the chart is sealed with a distinctive rubber band and marked with a red sticker confirming that the chart is now in HealthConnect.
It is not usually necessary to enter the medications during cutover since pharmacy has already entered these. Only nursing care orders, diet, code status, and ancillary staff consultations such as respiratory therapy, physical therapy, or nursing care consults are entered, simplifying the conversion. The charts are converted and sealed one by one until the last chart is done. The unit is then marked as being on HealthConnect.
Some teams move to other wards to continue the cutover, while some remain on the unit to offer post-live support and to assist the staff with their charting and workflows, which had previously only been practiced on the training environment. Certain key members of the staff on the nursing unit coordinate the flow of charts and make sure that new orders are not entered in the paper chart or paper notes are written after the chart is sealed.
During the go-live, emergencies always occur that require urgent surgical care. All staff are told that patient care comes first. Charting and orders in the EMR can be done later. A periop PCE (Physician Clinical Expert) is available at all times to assist physicians with the workflows and can be summoned by a simple phone call. PCE and FCE (nursing) support continues for three weeks after the go-live, 24 hours a day. After that, there is local trained software support staff for several more weeks. Telephone support is available through a local hotline and night support through a regional toll-free number. That continues indefinitely.
What have we learned?
First of all, the EMR absolutely does not change our business. We always focus and take care of the patient first. When you actually look at what we did before and how we do things now, the basic workflow, orders, and actions are the same as the paper chart. The difference is that the computer is much more specific about what goes where. It presents the same activities in a new manner that tends to trip people up or makes them feel like they are learning to practice medicine all over again.
There are inefficiencies and inconveniences and a lot of learning how to do things at first. With familiarity, improvements are evident within days. Those more than make up for the steep learning curve.
We stress to the staff that it is OK to make mistakes in learning the new workflow, telling them to do their best, focus on the patient, ask for help (since there is plenty of nursing, administrative, and physician support there in the first few weeks), keep their sense of humor, and give others the benefit of the doubt. We have found that encouraging the staff to stay in the workflows that were developed for them (navigators) and to keep documentation simple and concise helps all learn and become comfortable.
What about emergencies where there is not time to document? This actually happens. If we have time, we document the minimum, make the phone calls, take care of the patient, and document later. In a surgical emergency, patients can be brought from the ER to the OR with minimal documentation and can be taken care of in the usual fashion, with documentation following later. In these situations, even paper documentation is appropriate in the Epic workflow.
What about physicians who resist or are angry and "act out," or refuse to cooperate? There will always be these types of physicians, but their numbers are fairly small, perhaps two percent or less. With time, they can be usually brought around once the software nuances become more apparent and the advantages of an EMR are clearer. Peer pressure helps, too. Their complaints are listened to, acknowledged, and sympathized with, but they are reminded that there is no perfect medical record system.
What about physicians who cannot appear to "keep up" or fall behind? A few physicians, even in the paper record, fail to keep up or do sub-standard charting. The EMR makes their work or deficiencies easier to track and monitor. The most difficult decision that the local medical center leadership has to make is what to do about these deficiencies.
I am a strong advocate about why we are going to an electronic medical record. With the paper chart, only one person can work in it or review it at a time. If the chart is moved off the ward to another part of the hospital, no one has access to it. You can’t find it. If you want to write an order, you have to find the chart. If you write a brief operative note but the note is torn out and lost, then the note is lost for good. If you put a form in the chart that is accidentally removed, it is gone. If the binder comes loose and all the notes and charting falls on the floor, someone has to pick it up and put it together again. If you want to write an order but you are not physically present in front of the chart, you have to call and wait for a nurse and give a verbal order. If you want to see how the patient is doing, you have to call the nurse to get a report or go up and see the patient and look at the chart. If you want to review the orders to see what the patient is getting or what labs are ordered, you have to walk up to the floor and look at the chart. If a consultant is writing a consult in the chart, then you have to wait until they are done before you can review the chart. If the nurse is charting and you want to see the chart, then she has to stop what she is doing and give you the chart.
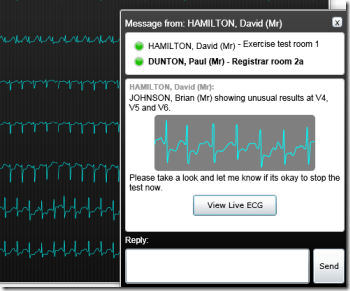
With the electronic medical record, at every day and at every moment, I can see and review the active medications and care orders and make corrections. It is a tremendous patient safety feature. I can communicate securely to the nurse and my associates using the medical record. Computerized physician ordering can help enforce national guidelines for antibiotics, deep vein thrombosis prophylaxis, and accidental ordering of medications to which the patient is allergic. Both medications and the patient are bar-coded, so deviations or overrides in medicine administration can be tracked and active interventions carried out.
I think you get the idea.
From the Mailbag
To have your question answered by Mr. H or Inga in From the Mailbag, just e-mail (note: if this is a medical emergency, please log off and dial 911).
Not long ago, Mr. H sent me the link to a certain Dr. V, aka Dr. Venus Nicolino. Dr. V is a psychologist who, according to Mr. H, is a “hottie” (he liked the clunky glasses just waiting to come off and the bedroom hair). He even suggested we might want to consult with her next time we had a neurotic poster or the like.

Since I wasn’t about to be displaced for a moment by someone named Venus, I volunteered to go through my recent e-mails and provide my own expert opinions on some of the more worldly matters that readers have brought to my attention. And to make me feel better about not having a smoldering head shot like Dr. V, Mr. H sprang for an artist-rendered picture (no kidding) that, while possibly a bit customer-flattering like all commissioned portraits, was actually drawn using real photos of me as a model. So, this is me as a Barbie doll.

Dear Inga,
I am totally with you on the fist bump thing. It’s just not me and not very professional. However, what do you do when one of your male co-workers presents his fist for bumping? There is a part of me that wants to be one of the guys and I really don’t want to come off as a wet hen. Signed, Handshake Gal.
Dear Handshake Gal,
I appreciate your desire to fit in with the guys. Guy co-workers can make the job fun and it usually is a good career move to get along with any of your fellow employees. So, the interesting thing about men in the workplace is that many aren’t much different than the guys you went to school with in 7th grade.

Remember the guys that would hit you because they liked you? It didn’t really make sense that they were smacking you, but in truth the guys just didn’t know how else to act around you. Many guys still haven’t got the whole woman thing figured out, especially those in the workplace. They don’t know if they should treat you as one of the guys (e.g., giving you the fist-bump) or as a delicate flower (like they do with their wives and girlfriends.)
The key to guys is you have to tell them what to do (this is a universal truth, by the way.) Unlike females, men don’t get offended if you tell them something plainly and don’t spend a week analyzing the situation to death.
So, next time you get a fist and you rather have a handshake, simply explain you aren’t a fist-bump kind of woman. Or, perhaps make him feel special and tell him nothing makes your day more than feeling the palm of a man’s hand. Trust me, this method works particularly well.
Dear Inga,
I’ve been thinking about that study you mentioned about the presence of a particular genetic variant that makes some men more prone to unfaithfulness. I think some men certainly seem to have trouble staying faithful no matter the circumstances. I found myself wondering what percentage of those men with high levels of the hormone were still prone to stray if the sex life at home was fulfilling and frequent. Can you tell I’m divorced? Signed, Manly Man.
Dear Manly Man,
There is no doubt that some men are simply pigs. However, those that choose to act like pigs should be aware that the female pig goes into heat only once every three weeks. I suspect everyone would be happier if people didn’t act like pigs.

Dear Inga,
I don’t know if you pay much attention to politics, but don’t you think it is pretty cool that there is a female on the presidential ticket? And she is attractive, smart, AND well-spoken. Even if one doesn’t agree with her politics it’s a great step for women! OK, so between us girls, what do you think of her hairstyle? Signed, Hear Me Roar.

Dear Hear Me Roar,
I have to admit I was pleasantly surprised by Palin. Even if her ticket doesn’t win, I suspect we will see more of her in the future.
Regarding the hair, I suspect it’s the bangs that you find troublesome. If that is the issue, I bet you are under the age of 40. You see, when you get to be a certain age, your choices are bangs or Botox to cover unsightly forehead wrinkles. I’m not loving the bangs either, but governors with five kids simply don’t have time for Botox.
 I have been reading discussions on the HIT provisions in the new stimulus bill that was signed this week by President Obama. One discussion that caught my attention relates to what it means to be a “certified” product. Throughout the bill, it states that funds are to encourage adoption of “certified” products. While it is not yet completely clear what this means, most folks are assuming it will mean certified by CCHIT.
I have been reading discussions on the HIT provisions in the new stimulus bill that was signed this week by President Obama. One discussion that caught my attention relates to what it means to be a “certified” product. Throughout the bill, it states that funds are to encourage adoption of “certified” products. While it is not yet completely clear what this means, most folks are assuming it will mean certified by CCHIT. 























I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…