Comments on Ricky Roma
By Cliff Dickerson
I’ve spent most of my career on The Dark Side, but I rarely have considered it to be that. Maybe I’m going to always be naïve, but it’s where I’ve witnessed innovation and achievement.
- I took pride in seeing the glee on the face of the DP director when transmission of the day’s billing was transferred in less than five minutes after removing the cartridge (yes, cartridge) from the Four Phase HIS and inserting it into the Four Phase front-end of a time shared financial system. It beat a day spent key punching by multiple employees.
- I was ecstatic when the ER nurse (pre-ED days) most vocally opposed to the new system told me that she loved it.
- I was pleased to know that in less than six months we had registration and ADT up, something that some major medical centers spent two to three years developing in-house or that the IT staff in the early days in a turnkey operation was a fraction of that where in-house development was occurring.
Trained as a biochemist and working in a hospital clinic lab, I fled early on to an HIT vendor. I knew that my happiness was not to be found being a bench tech. (Retention of medical technologists is a tricky act. The University of Illinois Circle Campus, in fact, eliminated its medical technology program upon realization that its graduates were not going to work for healthcare providers, but rather for biotech and pharma companies.)
The vendor life, while often paying more than on the provider side, has its disadvantages. Living out of a suitcase is not fun. Missing out on activities with friends and families is a real drag. 20+ hours of commuting is not so fun either. (When I first started, I left on Sunday afternoons and got home sometime Friday nights. It’s different now. People just don’t want to do that.)
Oh, and pay? I’ve seen some delivery organizations pay almost as much for its employees as a vendor does. $10K or $15K just doesn’t make up for long commutes and long days.
Now, I could go down a different road. Healthcare organizations traditionally have not paid IT salaries competitive with other companies. (Nor do they spend the same amount of money on IT traditionally – maybe you do get what you pay for.) And, boy, are they surprised when their clinicians turned informatics specialists say that they won’t work more than 40 hours a week unless they get overtime. But, that’s a whole other discussion about something that’s not necessarily unique to American healthcare delivery systems, but pandemic in our culture. We talk about balance, but don’t play the game.
I don’t discount anyone for wanting to make a profit – even not-for-profit health delivery organizations like to do that – and many of their employees and associates profit very well in doing so. Perhaps I should be more cynical in viewing publicly traded healthcare software vendors, but can I fault them anymore than I could fault Chase or Oracle or Phillips? No, I just can’t. (I do think that the American system has some problems. I do think that our American companies often make decisions that are poor in the long-term. I do think that we need to rethink our executive compensation system.)
Value: if someone is willing to pay $3 for $1 of value, well, I figure that they must be getting $3 of value. Or at least feel that they do. Maybe I’m a bit biased because I spent a lot of time studying pricing while working for vendors.
I’m not sure where the 66% failure rate comes from, but it does point out the need for clearly defined, achievable return on investments before the ink is signed. So many people don’t want to do their homework in advance. Technology in and by itself is no balm. It’s the implementation. How you use it. How you promote it. How you plan to ensure success.
I had a CIO teaching a class at a university ask me for a paper or case study about how poor project management lead to the failure of a project. I couldn’t find one. No one really wants to write about or talk about their failures.
Next Generation Hospital Laboratories Become a Driving Force in the Future of Diagnostic IT
By Richard Atkin, President and CEO, Sunquest Information Systems
 When Sunquest became a private corporation approximately 18 months ago, no one predicted the tumultuous economic conditions and events that would be taking place in the U.S. and worldwide. And we now know how important the healthcare IT industry’s role will be in helping deliver increased access to care, with improved outcomes, at lower overall cost.
When Sunquest became a private corporation approximately 18 months ago, no one predicted the tumultuous economic conditions and events that would be taking place in the U.S. and worldwide. And we now know how important the healthcare IT industry’s role will be in helping deliver increased access to care, with improved outcomes, at lower overall cost.
Back in October 2007, we saw a great opportunity for best of suite diagnostic IT solutions and publicly stated the strategic goals that we believed would best serve the current and future needs of our customers. We committed our focus and resources towards enhancing the automation capabilities and clinical workflow of Laboratory Information Solutions, improving patient safety, helping hospitals maintain profitability through outreach services, and to becoming a driving force and leader in the exciting area of predictive and personalized medicine. Now, with the dramatic changes over the past year, these same goals are even more relevant and delivering against them remains our top priority.
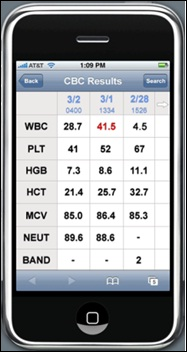
We must remember at all times that healthcare delivery is largely local and must be very patient centric. The role of the hospital laboratory in the continuum of care and the effectiveness of the Laboratory Information Solutions it uses are playing an increasingly important role in the successful delivery of clinical care inside the hospital and outside in the community. With approximately 70% of clinical decisions based on results generated in the clinical laboratory, the operational efficiency of the laboratory is critical to the effective delivery of safe, timely patient care. Laboratories are becoming information hubs for patient care, business operations, revenue growth, and the successful development of new technologies for predictive and preventative medicine.
The emergence of the hospital laboratory as a strategic, revenue generating service line, central to the goal of cost effective healthcare delivery is a development we are dedicated to supporting.
Automation & Workflow Efficiency
Laboratory services are central to healthcare delivery. Hundreds of care plan and treatment workflows are dependent on decisions that use lab results – admissions, discharges, medication decisions, follow-up testing and dietary orders to name a few. The shorter and more certain the lab result turnaround time, the faster patients and care providers can make diagnostic and care plan decisions, and the more effective those decisions will be.
Laboratory information systems must not only track, route and manage samples, but also interconnect with the overall Health Information Systems and EMRs being used within hospitals and with systems being used by external physicians and laboratories. By doing so, the transition from inpatient care to outpatient and vice versa is eased, vital resources are used more efficiently and the patient experience is enhanced.
Patient Safety
Patient safety is obviously a top priority for healthcare providers. At Sunquest we developed the concept of the Five Rights of Laboratory testing to champion the contributions the lab makes to the safe delivery of care.
Additionally, we have introduced several new products that support our customer’s goals for improving patient safety, including a closed-loop transfusion management solution. Our automated Specimen-Collection Management system integrates with the LIS and blood bank system, and utilizes wireless handheld devices and bar-coding to ensure positive patient ID at the bedside.
Closing the loop on the blood administration process, the Transfusion Manager solution is specifically designed to support patient safety processes at the bedside by automating nursing workflow and reducing preventable errors from occurring during the transfusion process.
These solutions in use at dozens of our customer sites have succeeded in reducing specimen collection errors to virtually zero at every site where deployed.
Expanding the Community Footprint
In challenging economic times, hospitals must leverage their laboratory as a strategic asset to their overall business operation and revenue generation. A single admitting community physician represents an average of $1.5MM in annual revenue to a hospital. An effective outreach program builds physician and patient relationships while enhancing the reputation of the hospital in the community.
The ability to effectively manage these community relationships is an important strategy for hospitals and the reason why we made two strategic acquisitions in Q4 of 2008.
First we acquired Anglia Healthcare in the UK for their complementary product portfolio of web based communications and messaging solutions. As a result, Sunquest now has the market-leading position in the UK with over 60% market share for laboratory orders and resulting solutions and the technologies to address the broader EU market with solutions that meet the region’s protocol standards and language needs.
We also acquired the Outreach Advantage portfolio from PAML, Spokane, WA. These solutions provide a strong complement to our existing offerings, adding courier, logistics, CRM, and business intelligence applications. The Outreach Advantage portfolio, together with our LIS and revenue cycle solution, results in the single most comprehensive outreach business management suite in the industry.
Predictive & Preventative Medicine
Patient diagnosis and treatments through molecular and genomic testing represent an area of explosive growth, great promise, and significant challenges.
Molecular diagnostics is generating more than 30 million tests annually in the U.S., with dozens of new procedures introduced every year. We are strategically committed to providing the solutions that will enable laboratories to be a leading force in the upcoming revolution with predictive and personalized medicine.
Nearly 85% of our customers already perform molecular testing and interface their instruments and systems with our LIS. One leading example of this is Nationwide Children’s Hospital, who has used its expertise in molecular diagnostics testing for infectious diseases to successfully grow its outreach testing services to support an international market.
Emerging technologies in genetic testing, digital analysis and whole slide imaging are creating a new paradigm for diagnostic medicine. Certainly the workflow inside the laboratory will dramatically shift, but even more significant is the impending transformation in healthcare delivery outside of the laboratory. Pathologists and lab professionals must become more active, visible members of the care team. To do so effectively will require collaboration, communication, and results interpretations that comprise actionable information, not just data.
Conclusion
This is both a very challenging and very exciting time to be in the healthcare industry. As vendors, we must develop and implement new solutions, in partnership with care providers, which make the industry more productive while also helping in the transformation of healthcare delivery. Connecting the laboratory to the continuum of care in the community and facilitating the transition to personalized, predictive and preventative medicines have the potential to revolutionalize patient care, improve wellness, reduce the cost of healthcare over lifetimes, and enhance quality of life for all of us. Sunquest understands its role and shared responsibility towards meeting the healthcare industry’s challenges and opportunities. We are dedicated to creating diagnostic information solutions that enable hospitals to fulfill their missions.
Will $20 billion Solve This Problem?
By Frank Poggio, The Kelzon Group
There was a poignant opinion editorial in the Chicago Tribune this Sunday that got my attention, written by Candy Schulman, entitled “There is a human in that bed”. It caught my eye and got my empathy because I lived that same experience about a year ago. There were however, two major differences. First it happened in a different hospital in a different state. Second, since I have worked in the hospital world as an administrator, systems supplier, and consultant for thirty-five years, I had a better understanding of the issues and therefore was able to force a faster resolution. As I read Candy Shulman’s article I kept asking myself, as I did a year ago, what is really wrong with this ‘system’ and what can be done about it? Also, I kept thinking will $20 billion solve this problem? Let me tell you a little about both stories before I give you my assessment and prognosis.
Candy’s Story – Dumped in the Driveway
Candy tells about her frustration in caring for her elderly mother while an inpatient at a local hospital. Two of her biggest problems came in simply getting her mother discharged at a reasonable time, and the lack of coordination with hospice care. The statement I most reacted to was, “After her month long hospitalization and three weeks in rehab, I tried all day to get her discharged, but ran into a hospital quagmire when I could not get anyone to sign the discharge papers. Finally, at 6 p.m., I left, believing I’d repeat the arduous process the next day”.
“Two hours later the rehab facility sent a bedridden, demented old woman home in an ambulance—alone. I wasn’t called to accompany her home, nor was her devoted live-in aide, Nellie (I was taking her out for a bite to eat after a long, tiring day). My poor confused mother was suddenly dumped into an ambulance. In the driveway of her apartment building, the driver seemed surprised that no one was there to take care of her.”
Candy Schulman’s complete article can be found at: http://www.chicagotribune.com/news/chi-oped0329humanmar29,0,552996.story
My Story – Who’s on First?
In February of last year, I lived through a similar experience. My 88-year-old mother, after years of struggling with CHF and COPD, was admitted to a Florida hospital. After a few days of hospitalization, we were told there was nothing that could be done and death was only a month or two away. My family decided the best course was to move her home and get the local hospice involved to supplement the efforts of me and my sister. I had spoken at length with her cardiologist, internist, and case worker and agreed this was the best course.
Needing a day to work things out with a local Hospice program, the hospital agreed she would be discharged in two days. I lined up the Hospice services to come to her home to set up the medical equipment, complete their assessment and explain to her their plan and what would transpire. Although my mother was severely physically impaired, she was of sound mind and fully cognizant of her surroundings to the day she died.
On the agreed-to day of discharge, I went to the facility to get her at 9 a.m., thinking that by 10 or 10:30 a.m. we’d be on our way. The day before, I told the Hospice staff we would be at her house by 12 noon and they then could commence their process.
To make a long story short, I did not leave that hospital until 1:30 p.m. that day, and then it was only because having worked in a hospital earlier in my career I knew how disjointed things can get. I personally tracked down the admitting doctor (not her cardiologist or internist) and brought him to the room to write the discharge orders and sign it. That was at 12:30 p.m. and still a number of other nursing and related tasks had to be completed. All the while I was running around the hospital, and in and out of her room, my mother kept asking, "Don’t these people know what they are doing and when can I go home?” I kept answering, “No they don’t, and if we’re not out by 2 p.m., we will leave AMA!”
What Went Wrong?
Everything involved with communication, coordination, and follow-up. No one knew who was on first, who had main responsibility, or what needed to be done next. As best I can tell, everyone involved was waiting for the next person to do his/her task, when in fact many of the tasks could have been done concurrently. Meanwhile this hospital has been using one of the leading HIS packages in the country for more than a decade.
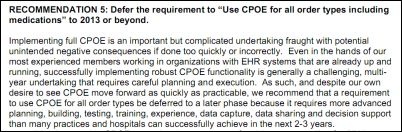
So let’s spend $20 billion on new HIT/EMR systems like Cerner, or Epic, McKesson, GE, Siemens, or Meditech — whatever flavor you like. It won’t matter. Although they may help a little, in my opinion, none of them can solve this problem. Here’s why.
The problem Candy and I described is not a data storage (EMR) or transactional (HIS) problem. It is a communication, coordination, trans-departmental workflow and management problem. Yes, HIT vendor systems can do communication, but they do very little, if anything, for work flow coordination and communication and almost nothing outside of ancillary medical services. These systems are great at ordering an x-ray and making sure radiology does the prep work, then delivering the results to clinicians and placing an image in the EMR. But what if that patient needs a dietary consult and the dietician comes to the room while the patient is still sitting in x-ray, one hour late for a test that was to be done at 1 p.m.? They almost totally ignore non-medical support services such as social work consults, dietary reviews, transportation needs, patient location or education, timely discharge orders, and more. Such tasks typically fall to nursing to ‘manage’. Inevitably one or more falls through the cracks, and when one fails the whole process collapses and the patient suffers.
Unfortunately, this problem is pervasive across health institutions as identified by a recent report issued by the National Academy of Sciences – Institute of Medicine (IOM) entitled Computational Technology for Effective Health Care: Immediate Steps and Strategic Direction. The report states: “Health care decisions often require reasoning under high degrees of uncertainty about the patient’s medical state and the effectiveness of past and future treatments for the particular patient. In addition, medical workflows are often complex and non-transparent and are characterized by many interruptions, inadequately defined roles and responsibilities, poorly kept and managed schedules, and little documentation of steps, expectations, and outcomes.”
If you still do not believe it is pervasive, then answer these simple questions. Does your facility have a time of discharge policy? If yes, what percentage of the cases hit that time within 15 or 30 minutes? Of course if you can’t answer either, that’s proof enough.
During my years as a hospital CIO /CFO and as a system’s developer I believed that the ever-expanding HIS tools and developing EMRs would someday address this problem. Today, after many years of hands-on experience at all levels, I am convinced they cannot and will not. In a nutshell, I have come to the conclusion this in not an information technology problem. It is a work flow process problem, a communication problem, and lastly, a management problem. It is not a department problem, but an inter-department or enterprise problem. An HIS /EMR can help solve it, but using those tools alone you are doomed to fail.
What is Needed?
The seemingly simple goal of implementing a set discharge time and meeting it has many challenges such as poor inter-department coordination and poor integrated work flow. Inter-department resource coordination founded on solid work flow documentation and monitoring tools is critical to successful patient flow and meeting discharge targets. Fortunately there are many sophisticated work flow tools developed outside of health care that can be used to help achieve better patient flow and control. Private industry has used tools such as optimization, production coordination, queuing analysis, and sophisticated enterprise scheduling for decades. Some of these are finding their way into health care now, but very slowly.
These tools go beyond electronic bed boards and digitized paper forms, both of which are needed but only address the symptoms. Hospitals need to know real time where they stand for any given patient. In effect, a Gantt chart or patient critical path for all activities is needed to meet a specific goal or target discharge time. Remember, a delayed discharge costs the hospital money and it’s the primary reason for ED diversions, which typically lead to large ED capital expenditures.
Proper coordination of all services (ancillary and non-ancillary) can help hospitals get through these tough times. It’s not easy, but by better utilizing your current resources, (staff, equipment and technology), through better work flow coordination, you can significantly improve patient throughput to drive improved productivity, reduced costs, enhanced revenues, and most importantly, increased patient satisfaction.
While in the hospital my mom, and I would believe Candy’s mom, received excellent medical care from some very dedicated and overworked people. But what we remember most clearly was the bungled discharge process that colored their entire stay. Medicare starts this year to measure patient satisfaction, so bungled discharges will soon become a costly mistake.







 Mr. Revak raises an interesting premise about the costs associated with use of clearinghouses, based on the 80/20 principle. However, I’d like to offer some additional perspective on the value of using a Web-based clearinghouse.
Mr. Revak raises an interesting premise about the costs associated with use of clearinghouses, based on the 80/20 principle. However, I’d like to offer some additional perspective on the value of using a Web-based clearinghouse.















I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…