Agile Analytics in Healthcare: Fast Deployment, Low Cost, Short Time to Value
By Jason Monroe, Mark Moffitt, and Satish Jetty, MD
Adena is a regional integrated health system located in southern Ohio serving seven counties around and including Ross County. The system is anchored by Adena Regional Medical Center and includes two critical care facilities, a freestanding cancer center, and 11 clinics employing about 180 providers.
Clinical, financial, and administrative data at Adena is spread across multiple systems including Meditech Magic (acute care), eClinicalWorks (ambulatory), LSS (previous ambulatory system), Lawson, and Kronos. Business intelligence or BI applications were limited to analysis of data in only one of these domains with a few exceptions. This made analyzing data across the enterprise difficult. The annual direct maintenance fees paid to BI vendors was about $500,000 per year and growing.
Adena was looking to improve clinical, financial, and administrative analytics by having a single system that could combine and use data across disparate systems, lower the cost of deploying and supporting these applications, and speed up the time to deploy applications requested by users.
The solution to Adena’s requirements for a BI system was found in a technology called associative query language (AQL). Our commercial BI product’s associative data model is designed for deployment speed and for providing users with an environment that is designed to encourage data exploration. It is easy to program and does not require personnel with specialized skills to build and maintain applications as compared to the traditional model for analytics using a data warehouse and cubes.
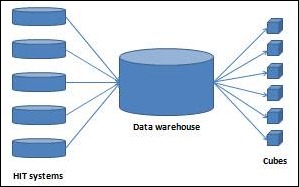
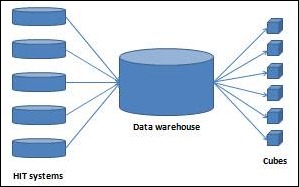
Traditional BI vendors use a data warehouse to consolidate data from multiple systems. Data is fed from transactional systems to a data warehouse in real time or in batches at the end of the day.
Once a data warehouse is deployed and populated with data, cubes are built and deployed to users. Cubes contain data from a data warehouse that is aggregated to answer a specific set of questions. A user is working with a subset of the data in the data warehouse rather than the whole data set. The design and build of cubes is an iterative and ongoing process between users and personnel with technical skills in building and optimizing cubes.
Our product uses data in memory in a compressed form with associations defined between data items rather than joins as used in a traditional database. These associations are derived automatically during the data load process into memory based on matching column names across tables. Matching column names from different systems is easy.
AQL makes it possible to load data from multiple transactional systems directly and bypass a data warehouse and cubes. The product does require work to set up and update a data set. However, this effort is much easier than building and maintaining a data warehouse and cubes.
The project was approved in late 2011 and started in January 2012.
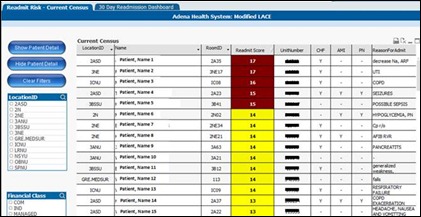
Readmission Risk Dashboard
The Readmission Risk Dashboard combines data from Meditech, eClinicalWorks, and LSS (ambulatory PM and EMR used prior to eClinicalWorks) to provide a complete picture of Adena’s inpatient census. The application uses the Modified LACE Tool which assesses patients length of stay, acuity, co-morbidities (20), and emergency room activity as a predictor of the likelihood the patient will be readmitted within 30 days of discharge. Adena has initiated protocols based on a patient’s LACE score that include:
- Nurse navigator consults initiated for patients with a LACE score of ≥ 11.
- Coordinated conversations with the attending physician, nurse navigator, and the patient’s primary care physician initiated for LACE score of ≥ 15 to discuss options such as palliative care.
The initial result of this project is enhanced productivity of our nurse navigators and significant enhancement to the timeliness and pertinence of the data that is presented to care providers. Long term, we expect improvement to the readmission rate at Adena Health System, which has a positive financial impact, but more importantly, allows for improved quality of care and overall patient experience.
The build of this application took less than two weeks from discussion to a beta version available in production. The clinical program is in pilot and will be implemented system-wide.
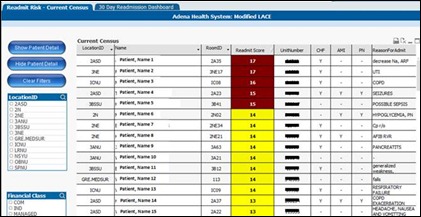
Figure 2 – Readmission risk dashboard
Readmission risk dashboard summary:
- All inpatients
- Sorted by highest modified LACE score
- Patient detail including problem list, ED and urgent care visits, scheduled appointments
- 30-day readmission tracking dashboard
- Data sources: Meditech, eClinicalWorks, LSS
- Application development time: two weeks
- Time to deploy: four months
- Direct savings through elimination of other system(s) or avoidance of new system(s): $80,000 per year
Patient Centered Medical Home (PCMH) Dashboard
PCMH is an initiative that is being piloted in one primary care provider office. The PCMH dashboard was developed to give providers and staff a view of PCP’s patients admitted to the hospital, patients seen in the emergency room or urgent care in the past 30 days, and inpatient discharges for the past 30 days. This dashboard gives providers easy access to information not previously available. The program gives nurse navigators a tool to identify patients needing discharge follow up or more dedicated attention.
Additionally, the application lists patients scheduled in the next few weeks that have a chronic disease. Clinicians are able to determine if the patient has required lab or imaging tests scheduled so the tests are completed prior to a clinic visit. Previously this was a manual process requiring considerable staff time to assemble the required information. No screen shot is provided because most of the data is patient information.
PCMH dashboard summary:
- PCP’s patients in hospital
- PCP’s patients who have been to the emergency room or urgent care in the past 30 days
- PCP’s patients discharged from hospital in the past 30 days
- Patients with chronic disease scheduled in the next three weeks
- Data sources: Meditech, eClinicalWorks, LSS
- Application development time: 45 days
- Time to deploy: 60 days
- Direct savings through elimination of other system(s) or avoidance of new system(s): $500,000 over three years
Provider Scorecard
Wellness and preventative health is tracked for annual wellness exam (AWE), mammograms, colonoscopy, osteoporosis screening, and BMI capture rate. For comprehensive diabetes care, performance rates are monitored for A1C control, LDL control, and microalbumin screening.
At the provider level, readmission rates are tracked for CHF, AMI, pneumonia, and COPD. Also, patient experience scores are extracted from Press Ganey data and incorporated. Finally, the dashboard displays practice activity, in real time, of patients waiting in the reception area, patients in a room waiting on a physician, and patients in a room with a provider.
Provider scorecard summary:
- Provider and practice level scorecards and performance metrics: wellness and preventative Health is tracked for AWE, mammograms, colonoscopy, osteoporosis screening, and BMI capture rate
- Comprehensive diabetes are: performance rates monitored for A1C control, LDL control, and microalbumin screening
- Readmission rates are tracked for CHF, AMI, pneumonia, and COPD
- Real-time view of patient activity in a clinic
- Data source: Meditech, eClinicalWorks, Press Ganey
- Application development time: 60 days
- Time to deploy: 90 days
- Direct savings through elimination of other system(s) or avoidance of new system(s): $140,000 per year
Revenue Cycle Management (RCM)
Rather than buy a third-party application for RCM, the commercial BI product was used to build an application to provide functionality in the first phase including aged trial balance, summary detail, transactional detail at patient level, coding workflow, self-pay analysis, and account balance in multiple insurance
- Data source: Meditech, eClinicalWorks
- Application development time: 16 weeks for Phase 1
- Time to deploy: 20 weeks
- Direct savings through elimination of other system(s) or avoidance of new system(s): $250,000 per year
Personnel spent the previous year trying to meet the requirements of this project using Excel, and when that failed, another vendor’s BI system that failed to meet the requirements of the program. Using the commercial product, the team was able to produce an application that met all requirements in 90 days.
At the start of the project, there was only Adena employee working on it. Consultants were used for the first four months to accelerate development on RCM applications. A second person was added to the team in July 2012.
Super users are being trained in RCM, finance, clinical, quality, operations improvement, strategy, and the Adena Medical Group. These are not new hires, but subject matter experts in their area with strong Microsoft Excel skills. These super users work with SMEs to build prototypes, deploy applications, and support programs in their respective area.
The first year of deploying the system had expenses of $500,000, mainly licenses, hardware, and consulting services to accelerate work on RCM. Direct savings so far equals $2 million over three years. These savings are from the cancellation of contracts for existing systems or cost avoidance of new systems that were budgeted and planned for deployment.
Another benefit to the system is that applications are being developed faster. Before, clinical programs needing analytics waited as applications were purchased and installed. Using the commercial BI product, prototypes are built in days or weeks and applications are piloted in a few months and at a lower cost than before – hence the term agile analytics. The results have exceeded our expectations.
Jason Monroe is director of enterprise data management with Adena Health System. Mark Moffitt, former CIO at Adena, is senior director with Ascension Health Information Services-Seton. Satish Jetty, MD, is CMIO of Adena Health System.
















I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…