EPtalk by Dr. Jayne 5/31/18
A reader sent me this piece about an Ohio hospital that added physicians to the emergency department triage process, helping them lower their wait times for patients to be seen by a provider. The headline was attention grabbing, but when you look at their process, basically they started running their triage area like a mini-urgent care, with providers performing H&Ps and ordering tests. They also created a separate waiting room for patients who were waiting for test results. I’m not sure how different this is from creating a “fast track” section of the emergency department or adding an on-campus urgent care or convenient care facility to divert non-emergency cases from the core emergency department. I’m sure it created some interesting flows for documentation, since providers would be using different workflows depending on whether they were working in triage or as traditional emergency department physicians.
When I work with clients who are “stuck” with their EHR projects, I occasionally encounter a physician who has built his own EHR and uses it as the gold standard against which he compares what we’re trying to implement or optimize. (I use the male pronoun intentionally, because I’ve never had a woman physician admit to it.) I’m all for home-based innovation, but I have to draw the line at DIY Gene Editing which apparently is a thing. Apparently, there are meetups for these biohackers, including “Body Hacking Con” which was held in Austin. After reading how easy it might be to brew up a batch of bioweapons in your bathtub, I’m almost wishing I hadn’t read it. Plausible deniability might be better, after all.
EHR vendors take note: the next set of screening questions you add to your product might need to be around your patients’ tax preparation strategies, or lack thereof. The StreetCred program is a partnership between various hospitals and community organizations, including Boston Medical Center, where patients are supported so that they can receive tax benefits and other entitlements that might help reduce the impact of poverty on chronic medical conditions. BMCs program operates through the Department of Pediatrics and ensures that clients receive tax credits for which they qualify along with tax refunds. Families with improved financial stability have lower stress levels and higher participation in care programs than those whose situations might be more tenuous. Yale School of Medicine has a similar program based on the work at BMC.
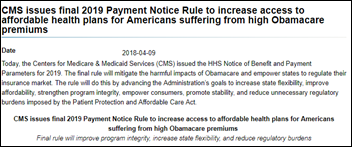
Kudos to CMS for figuring out new ways to use acronyms to confuse us. The Direct Provider Contracting model is being referred to as DPC, causing confusion with the Direct Primary Care movement. In Direct Primary Care, patients contract directly with a primary care provider (usually a solo physician although some DPC practices are small groups with low overhead) for services and pay a monthly fee. Direct Provider contracting is different, and includes provider networks which receive Medicare funds in an advance-payment scheme, to manage their patients’ care. It’s considered a potential alternative to the Alternative Payment Model (APM) options already out there. MGMA has already voiced concern about this new direct contracting model and its potential negative impact on small groups.
CMS further sullies the acronym soup by referring to these provider networks as CIOs (clinically integrated organizations) which by necessity must include professional, technical, and hospital service components. Medicare would incent patients to participate by offering lower co-pays for patients seeking care within the CIO-created network, which sounds dreadful for anyone who has ever had to deal with an unexpected “out of network” bill. Most billing systems do a mediocre job of handling non-fee-for-service payments, so providers who might want to do this need to be discussing it with their EHR and practice management system vendors as this unfolds. It’s another nail in the coffin of ambulatory-only products since trying to do the cost accounting needed to make this viable becomes tricky when you’re working on multiple systems. I missed the boat on this one since CMS only accepted public comments on it through May 25.
Given our society’s obsession with smartphones, I am always on the lookout for articles discussing how people use them effectively or to their detriment. In my travels, I see more and more people who are so engaged with their phones they create problems for the people around them. On my flight this week, a woman deplaned a few people in front of me and pulled out her phone in the jet bridge. Her forward momentum dropped as she started fiddling with her phone, resulting in the person behind her (who was also fiddling with a phone) smacking into her. Heads up and hands out, people, and be ready to interact with the world around you. Unfortunately, judging by the number of children in the under-13 set who are also face down on phones or tablets, I don’t see any improvement in this over time. The Wall Street Journal covered the topic, discussing CEOs who have tried to address the issue. The statistics are staggering — the average person engages with his or her phone over two hours per day, including during work hours.
I’ve been in meetings were electronics are banned and find it unfortunate mainly because I take verbose meeting notes on my laptop all the time. Taking notes on paper results in lost productivity later as I have to transcribe my notes. I also like to fire off action item emails in real time rather than carry a list of to-dos back to my desk. On the other hand, I’ve watched people openly surf Facebook or play games during meetings and that’s just not acceptable.
Going “no phones” needs to also address the prevalence of smart watches and other notification devices. My clinical office has a “no cell phones” policy in the workplace and surfing the internet is against our code of conduct. Employees aren’t even allowed to have phones in their pockets for emergencies – they are expected to provide their children and loved ones with the office phone number so they can be reached in case of emergency. Although this may sound draconian, it has resulted in more engaged employees who look for tasks to complete in the office or who actually talk to their co-workers rather than head down the social media rabbit hole. Apparently, an upcoming version of the Android system will include a time tracker to help people track their phone use and I have some family members I can’t wait to try it on.
What do you think about smartphone overuse? Are we addicted or just bored? Leave a comment or email me.

Email Dr. Jayne.















Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…