EPtalk by Dr. Jayne 4/6/23
As a clinical informaticist who has been around the block more than a couple of times, I know I have more knowledge than the average physician about how EHRs work. As an informaticist who has spent the majority of her career working with large health systems and healthcare delivery organizations, I also have a good knowledge base for all the ways organizations can be set up and how they manage their relationships with physicians in their communities and in affiliated academic institutions.
I’m a member of a couple of groups on social media that help physicians navigate issues with their EHRs. I enjoy helping people find solutions for their issues or at least helping them figure out who in their organization to approach for help. It’s kind of my way of giving back, since I didn’t have a lot of help when I started out in the EHR world and I remember how helpless I felt.
A number of large organizations have extended their EHRs to community partners, and nationwide organizations provide hosted versions of various EHRs to smaller practices. I’m working with someone who just joined a two-physician practice that is on one of these hosted systems, but has no idea how to get help. Part of the problem is that she joined an existing practice that expects her to just take things on faith, even when they’re not working correctly (like when she hasn’t seen financial reports since the 2022 year-end close). The situation is complicated by the fact that the organization has given cutesy names to various EHR initiatives and modules that don’t actually align with the names given by the EHR vendor or standard terminology like “practice management system.”
For a while, none of us could figure out what EHR she was on until the group got her to send a screenshot of her login screen. She doesn’t have access to any vendor resources or education outside of what is offered through her partner health system’s learning management system, which she mistakenly thought was actually offered by the EHR vendor. The office manager is stonewalling, saying that the physicians aren’t allowed to talk to the EHR liaison.
Although I understand trying to have a local support structure in place to keep physicians from calling about things that could be handled by their office managers or super users, there seems to be a huge disconnect. Most of the large healthcare delivery organizations I’ve worked with that have these kinds of community offerings also have a designated physician liaison to work with the community physicians and make sure their needs are met, and that doesn’t seem to be happening here.
I’m hoping that we can help her figure out ways to learn how to work more efficiently in the EHR as well as ways to work with her practice leadership to make sure they’re not just taking advantage of a new physician fresh out of training who doesn’t yet know the right questions to ask. Unfortunately, most residency training programs don’t include any kind of education in the business of managing a medical practice or in trying to manage colleagues or navigate the minefields of hospital medical staff politics, so I’m hoping we can at least help her a little.

I critique the emails that I get from vendors prior to conferences, but I have to give full credit to Merative for their appropriately themed email promoting Merge Imaging solutions. The subject line was “It’s 106 Miles to Chicago…” and the email opened with “It’s HIMSS… and we’re wearing sunglasses. Hit it!” The Blues Brothers were iconic during my formative years and the musical numbers from the film are some of my favorites. Chicago isn’t my favorite location for conferences, but I always love a good Blues Brothers throwback, so thanks to the team at Merative for making a tired CMIO smile at the end of a long day.
I recently had to change my phone number and the process has caused chaos with some of my online accounts and loyalty programs. I was interested to see that Panera Bread is testing Amazon’s biometric technology at its bakery-cafes, specifically with palm scanning. Customers can scan not only to link their orders to the loyalty program, but to pay for them as well. The technology is already being used at Whole Foods locations along with some sports venues. Although some people are skeptical of giving up their biometric data, using facial recognition to unlock phones is commonplace so it’s hard to argue against palm scanning. Panera is resting at two locations in St. Louis and plans to expand use to up to 20 sites over the next few months.
It’s not about healthcare IT, but all of us are patients at some point in our lives. From a patient perspective, this research article in JAMA Internal Medicine caught my eye. The authors look at more than 200 new drugs approved in the US from 2017 to 2020 and how they were approved (or not approved) in other countries. More than 20% of the drugs weren’t approved in Australia, Canada, or the UK “due to unfavorable benefit-to-risk profiles, uncertain clinical benefit, or unacceptably high price.” Unsurprisingly, the median cost for these medications in the US was more than $115K per patient per year, with some being over $230K per patient per year. As the old saying goes, follow the money.
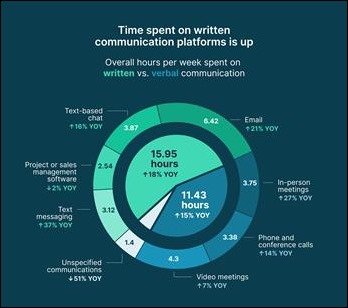
One of my favorite CMIOs sent me this MIT Technology Review article about how to break the cycle of being hooked on our devices. The highlight reel — screen time isn’t always bad, and sometimes we just need to do some mindless surfing. However, understanding how engaging with the digital world is making us feel can be valuable. Setting boundaries around digital time can be helpful, and developing new things to do when bored can help break the cycle of digital dependence.
I’m a big fan of that last piece of advice. I’ve always been a big reader and usually carry a book if I’m just around town or my Kindle if I’m on a plane. I’m a member of a couple of book clubs that have forced me to read some things that are outside my usual comfort zone. I’ve enjoyed it, plus it’s a good way to force yourself to disconnect. I still have the guilty pleasure of doing the Wordle every morning, but I don’t think that’s going to be too many people’s downfall.
What’s your favorite online time waster? Leave a comment or email me.

Email Dr. Jayne.



















Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…