EPtalk by Dr. Jayne 10/13/22
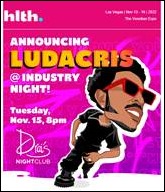
The HLTH conference team has announced the headliner for its Industry Night celebration. Let’s just say nothing celebrates digital health and transformation quite like Ludracis.
The American Telemedicine Association shifts the dates of its ATA2023 Annual Conference & Expo. The conference moves from a mid-week placement to begin on Saturday, March 4 and will run through Monday, March 6. The organization notes this is to accommodate busy schedules and to ensure that “even more frontline providers and virtual care practitioners” can attend in person. The meeting remains in San Antonio and two of the evening events have “Celebrity Mixologist” in the title, so it looks like it will be entertaining as well as educational.
The National Center for Health Statistics releases provisional life expectancy estimates for 2021. It shows that from 2019 to 2021, US life expectancy dropped by 3 years for men and 2.3 years for women. The new values – 73 years for men and 79 for women – are the lowest since 1996. Approximately 75% of the drop was attributed to COVID-19 deaths, with the remainder including overdose deaths, suicide, chronic liver disease, and homicide for men. Women lost years due to COVID-19 as well as heart disease, stroke, and chronic liver disease. Losses were not as high as they could have been, however, since they were somewhat mitigated by reductions in deaths due to influenza, pneumonia, and other respiratory diseases.
Mr. H recently posted a poll to assess “Which of the following items did you earn after age 35 that has been most valuable in your career.” Although there were some good choices, including master’s degrees, doctorates, professional degrees, and more, the list didn’t include my personal pick: my Clinical Informatics board certification. As a relatively home-grown clinical informaticist, most of my training was of the on-the-job variety and a good chunk of the learnings were through the school of hard knocks. I didn’t have the opportunity to do a fellowship in the discipline, but worked my way through the major texts of the specialty through grim determination and the Interlibrary Loan system.
In second place, I’d put vendor-specific certifications. I don’t know how much they’ve really helped me with my career, but they’ve definitely helped me do the day-to-day aspects of my job better. Even though I’m in a leadership role, having the certifications allows me to speak the same language as my analysts and better understand the different features and functionalities that we’re implementing. It’s also entertaining when people discover that although you’re a physician, you have certifications in the practice management and billing portions of the application. Not to mention that I’m always happy to talk about EDI and Coordination of Benefits over a cocktail or two.
The Medical Group Management Association, in conjunction with Jackson Physician Search, releases a report on physician turnover in the US. The sample size was small at 326 physicians, but the data is recent since it was obtained in August 2022. Among the most interesting findings: 51% of physicians have considered leaving their healthcare employer in the last year, with 41% considering leaving medical practice and 36% contemplating early retirement. I wonder what percentage of those who are considering leaving medicine could be mitigated if care delivery organizations were willing to create more novel practice arrangements.
For example, I have several friends who have left medicine in the last couple of years because they didn’t want to work full time as primary care physicians. There’s a perception that having part time physicians is difficult or creates scheduling or administrative headaches, so they would rather let people leave. My former medical group was unsupportive of job-share arrangements. Although there was one highly successful physician pair who was tolerated due to their seniority, no additional arrangements were allowed. Assuming the right contractual language and appropriately paired physicians, there’s no inherent reason why a physician job-share wouldn’t be successful.
In the last two decades, I’ve been let go by two emergency department staffing groups because they made the determination that they didn’t want to contract part-time physicians. They can’t use administrative burdens as an excuse since both of them allowed part-time nurse practitioners and physician assistants, who are actually harder to schedule than physicians due to supervisory requirements in my state. Those of us who were let go each time concluded that the motivation was largely financial, although staffing groups would never admit to it.
Several of us started doing our own variations of an in-town locum tenens gig, where we provided supplemental coverage for acute ambulatory visits at peak times such as Mondays or Friday afternoons. We would also cover vacations, maternity leaves, and time off due to FMLA. There was good uptake on our services by individual physicians, but we could never quite get the big health systems in town (or their affiliated medical groups) to consider making us part of their teams. I guess they would rather see physicians scramble for coverage on their own, or worse for morale, just not take time off.
I’d love to get back to seeing patients in person and would be happy to work evenings and weekends if someone were looking for a part-time doc. Unfortunately, the only place willing to hire someone for fewer than 12 shifts per month is my former urgent care, which I wouldn’t touch with the proverbial 10-foot pole.
The MGMA report has a whole section on burnout and summarizes the results of a May 2021 look at burnout. At that time, 86% of healthcare leaders said they didn’t have a formal plan or strategy to reduce physician burnout. By August 2022, the number of leaders who admitted not having a plan had dropped to 66%. Although it’s a move in the right direction, every organization should have a plan in place to address burnout not only of physicians, but of all members of the clinical care team.
We’re living in unprecedented times and everyone is stretched to the limit. Case in point: the charge nurse in the emergency department at St. Michael Medical Center in Washington called 911 because the department’s five nurses were overwhelmed with 45 patients in the waiting room. She requested that firefighters come assist and they did, taking vital signs and helping turn over rooms between patients.
What is your organization doing to help with burnout? Or are they just keeping their collective heads in the sand? Leave a comment or email me.

Email Dr. Jayne.


I'd never heard of Healwell before and took a look over their offerings. Has anyone used the products? Beyond the…