Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
Monday Morning Update 7/19/21
Top News

The New York Times says that IBM Watson failed to achieve its goals to transform industries and make IBM successful. It says that Watson’s capabilities were oversold by IBM’s top executives – mostly former sales and services people – who ignored the warnings of the company’s scientists that it was a one-trick pony that was built purely to win “Jeopardy.”
The article notes that Watson’s healthcare “moon shot” failed in multiple health systems, as the technology was not capable of performing real-time cancer diagnosis or smart literature searches. IBM has discontinued its genomics and oncology offerings after they failed in high-profile health systems.
IBM’s Watson Health business spent $4 billion to acquire Merge Healthcare, Phytel, Explorys, and Truven Health Analytics. The company is reportedly considering selling those businesses as it lags competitors in cloud computing. Watson Health is reportedly bringing in $1 billion in annual revenue but still loses money.
NYT says Watson is “a sobering example of the pitfalls of technological hype and hubris around AI,” but says the technology has improved to the point that it can manage workhorse natural language tasks as offered by IBM’s cloud competitors, such as task automation and virtual assistants.
Reader Comments
From He’s Not Here: “Re: remote patient monitoring. Doesn’t that term contain a bit of geographic paternalism?” It does. Healthcare was historically built around the “my patients come to where I am” model, where other than for the rare house call, the provider has always sat in their building and waited for people in need to show up. I would say that in itself is not paternalistic since it’s no different than any other retail or professional business that doesn’t involve services that are provided in the home or on the road, but the idea that a patient is “remote” begs the question, remote from what? It’s the same as “after hours” care – after whose hours? Still, while some monitoring could be performed regardless of patient location, the capability must exist to react to it by dispatching humans, and that’s a last-mile problem for many patients, especially when health systems and the emergency services providers who have boots on the ground are almost always disconnected and sometimes competitive.
HIStalk Announcements and Requests
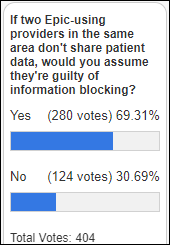
Most poll respondents presume that information blocking exists when Epic-using providers in the same area aren’t sharing patient data. My opinion is that we know that most EHRs can exchange patient data – as evidenced by at least one client of each vendor who is actually doing it – so ONC should focus on eliminating the “we weren’t aware” provider excuse via outreach and setting patient expectations to increase interoperability demand.
New poll to your right or here: Which tech company will have the most impact on US healthcare in five years? I will leave it up to respondents to define “healthcare impact.”
Dear companies – while I appreciate the option to engage with your website chatbot even though I can’t imagine a situation in which I would actually do so, please do not make it beep at me, especially every time I navigate to a new page of your site. That’s not exactly a testament to your software usability expertise.
We’re doing some pre-HIMSS summer slacking off around here lately. Jenn was vacating last week so we posted few sponsor updates, while I was day-tripping with Mrs. HIStalk Friday and elected to skip writing the Weekender. It feels good to have places to go and things to do after losing last summer to hunkering down, but sometimes having so many options available again makes me anxious that I’ll miss something.
Webinars
July 28 (Wednesday) 1 ET. “Stop running from your problem (list): Strategies for streamlining the EHR’s front page.” Sponsor: Intelligent Medical Objects. Presenters: Amanda Heidemann, MD, CMIO, CMIO Services LLC; James Thompson, MD, physician informaticist, IMO. How can clinicians mitigate the longstanding EHR problem list challenges of outdated or duplicative entries, rigid displays, and limited native EHR capabilities? The presenters will describe how to analyze current problems, create a problem list governance strategy, and measure improvement progress.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
OM1, which offers chronic disease registries and real-world data, raises $85 million in financing.
Sales
- Baystate Health (MA) expands its Cerner implementation with HealtheIntent for its physician organization and unspecified revenue cycle solutions.
People

Gary Christoph, PhD died earlier this month of Parkinson’s Disease at 76. He spent time as CIO of HCFA (now CMS), leading it through Y2K and cybersecurity and writing many of the regulations contained in HIPAA. He also led IT for NIH and Northrop Grumman’s healthcare IT group.
Government and Politics

The Senate confirms Donald Remy, JD as VA deputy secretary, its second-highest official. He will take charge of the VA’s Cerner project. Remy, who was confirmed in a 91-8 vote, is an Army veteran and COO / chief legal officer of NCAA.
A patient advocacy group’s review of the websites of 500 hospitals finds that 471 have not posted their prices as required by federal transparency rules that took effect January 1. The group says the $300 per day penalty should be increased.
Other
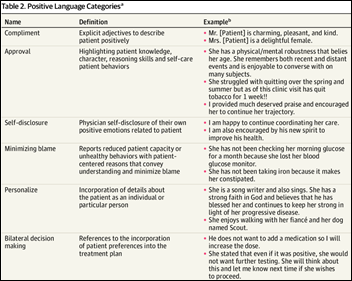
A JAMA Network Open article suggests that physicians avoid the use of “stigmatizing language” in their notes since patients may see them. The authors suggest avoiding language that questions patient credibility, indicates disapproval, stereotypes race or social class, indicates that the patient is difficult, or that conveys a paternalistic tone.

Three weeks before HIMSS21, the COVID-19 resurgence in Las Vegas causes the Venetian, Palazzo, and Sands to once again require their employees to wear masks, regardless of vaccination status. The health district is also recommending that everyone wear masks while indoors, advice that will surely be ignored by 99.5% of visitors. The Nevada Gaming Control Board has not re-imposed casino masking policies so far. The HIMSS21 “no masks required” policy remains aligned with CDC and county recommendations since all attendees must be vaccinated. COVID-19 case counts, positivity rates, and hospitalizations in Southern Nevada have returned to February levels, with 78% of those new cases being accounted for by Clark County. More than half of the state’s residents have not been fully vaccinated. The situation is so significant that the public health chief of Los Angeles has advised locals, especially those who are unvaccinated, to avoid travel to Las Vegas.
Sponsor Updates
Blog Posts
- A Revenue Cycle Guide for Private Equity Firms in Healthcare (RCx Rules)
- 10 Key Facts Hospitals Should Know About Denials in 2021 (Vyne Medical)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



What is a dollar number that would actually incentivize hospitals to post their prices? $300 a day is just over $100,000 a year which is effectively a rounding error for many of these large systems.
It’s not clear to me how much of the issue is that they don’t want to do it and how much is that it’s not easily available in a single source that’s able to be posted and updated easily. I suspect that there are elements of both but I don’t think it’s as straightforward as it sounds. Plus, hospitals are still coping with ongoing COVID related crises, backlogs of health IT projects that were put on hold due to COVID priorities, and the usual laundry list of inane requirements by CMS, Joint Commission, and others that have organizations in a constant cycle of having to quickly adjust systems to comply with the latest edict. Simply escalating penalties doesn’t solve the issues—it just pushes a different priority onto the back burner including ones that may be critical to individual patient or public health. Also knowing the price doesn’t have anything to do with what you pay after insurance and may actually disincentivize people from getting essential care.
It shouldn’t be about the dollar value. If you operate in the united states, you should do your best to follow the law. What you’re seeing here is widespread malfeasance by health systems. Regulators should come down hard on them in response.
I agree, it shouldn’t be. Sadly it appears that we aren’t going to see compliance without a larger incentive.
I feel like the question of geographic paternalism depends on parsing. (Remote patient) monitoring has the problem you cited about what the proper location is. Remote (patient monitoring) conveys that the clinician is far from the patient, which is true and doesn’t have the same value judgment to my ear.
That’s a good point. Remote patient monitoring doesn’t necessarily involve a windowless command center in Monolith Medical Center — it could even be the patient who’s in the hospital while the monitoring clinician is sitting at home in pajamas.
RE: Watson. I’ve been in HIT for 30 years, but never a competitor to IBM’s systems so this is not sour grapes. I have been an IBM ‘partner’ in 2 different companies, a position I would not wish on my worst enemy. (Their clients are their clients, and my clients are their clients type of attitude).
Ever since introduction 20+ years ago, I kept saying that Watson was a hammer looking for a nail. The main premise was its use in diagnostics, and I’m sorry but well-experienced and well-read physicians can achieve similar or better conclusions than the box with the blinking lights, which at best could only suggest possible diagnoses.
The fact it may be finally going away IMO is due to how IBM does things. The people ‘upstairs’ decide they are going to build it, they force sales on their sales teams, causing many careers to end early due to lack of making quota (because few wanted it) and guess what? All those ‘upstairs’ get their bonuses and promotions even though it was a failure. Just the last team charged with locking the door and turning out the lights may suffer career wise.
I also say that the Jeopardy competition was unfair because of reaction time to ringing in. The machine could react in a millisecond, and nearly every time a competitor was able to ring in was due to Watson not finding the answer quickly enough to green light the buzzer. The way to fix it would be to have a human ring in for Watson which would have evened the playing field.
Mr HIStalk knows my earlier positions on Kim Polese and Marimba, and most recently Theranos and Liz, BOTH of which I had corresponded about well before the crash and burn. Watson is in this same arena – except I will say that I do not accuse them of anything untoward, unethical, or illegal like those other two possibly did – but I do say IBM got out in front of their headlights big time. As we now see.
The problem with Watson? I feel that they needed to focus on something specific, some true value-add that either only Watson could achieve, or that Watson clearly did better than any other solution.
Instead, Watson was targeted at anything and everything. Even “Healthcare” is far too broad a mandate! It leaves both IBM and customers casting around, hoping to find a good fit for the technology. In effect Watson is a lab experiment. It’s a product in development. It’s a research thesis that isn’t ready for commercial deployment.
Once you find one thing that Watson is truly good at, then you can slowly broaden out the mandate and applications of this tool.
The other thing all the Watson hype did is to attach revenue expectations, and even stock valuations. Watson wasn’t even close to ready for those responsibilities.
I was hoping that IBM would be more upfront about their methods but I am just not seeing it. Using NLP and literature to conduct diagnostics is ignoring the use of boilerplates and specific clinician bias in diagnosing and recording — self damaging. There is also the problem of external organizations asking for specific data that might not have been useful to the diagnosis but are consistent none the less –external influencers (HEDIS?). How about how a particular practice administers its system or sets workflows — internal bias. And are you going to train your AI based on the solution? Each vendor has its own peculiarities that need to be addressed — baked in bias.
I can see imaging solutions being close to being ready — with a plethora of training material associated with a diagnosis the solution could train in pretty good order. But, how are you going to train it to practice oncology? It is one thing to train a system to read handwriting on an envelope, quite another to interpret and treat the multivariate problem that is practicing medicine on people.
I think that approaching something “small” like Clinical Decision Support (one attribute at a time) would have been useful. But, as we recently saw with the Sepsis Prediction Model the more complicated and multivariate the problem space the slower you should go.
IBM Watson failed while Health Catalyst succeeded. In my mind they are in the same market: consulting heavy healthcare analytics companies.
re:Watson Having worked at one of the four start-ups that IBM purchased and then destroyed, it’s prime material for a Case Study. Bringing in IBM resources (including Senior IT) that couldn’t spell Healthcare and were now in charge was the beginning of the end. No ability to focus on the right problems, selling software that didn’t exist, making promises that were impossible to fulfill, etc. etc. etc. Not aware of anyone that was there at the time that is upset about IBM losing their a**.