So your contention is that DOGE was a good-faith administrative effort? LOL! Parachuting in unqualified outsiders ought to be a…
EPtalk by Dr. Jayne 10/29/20
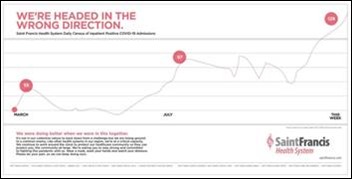
Hospitals and health systems are going on the offensive against COVID. One example is this two-page ad in the Tulsa World that illustrates hospitalizations within Saint Francis Health System.
Hospitals in my metropolitan area are approaching maximum capacity, having taken numerous transfers from rural hospitals that quickly became overwhelmed as cases surged. Our flagship tertiary care hospital has put limits on elective operative cases, not only to preserve bed capacity, but also to try to mitigate the load on care delivery staff who are anticipating a rocky winter.
One of my ICU nurse colleagues has been working with COVID patients since the beginning, spending several months in a vacant college dorm to reduce the risk that she would take the virus home to her high-risk household. In the ultimate show of compassion, another nurse from a “regular” unit offered to trade places for a few weeks so that my friend could have a break. It’s people like these that drew many of us to healthcare, those who truly set the example of service. But it’s a sad commentary on where we are right now and the concerns around what is to come. We had two more resignations at my practice this week and I fear more are to come.

ONC released a data brief this week looking at the state of interoperability among major US cities. The report looked at variation in interoperability within 15 cities, which are represented by combined statistical areas. They looked specifically at four key areas of interoperability – to find, send, receive, and integrate electronic health information with sources outside their health system. Data on HIE participation was also included.
Not surprisingly, small / independent hospitals performed the worst, with system-owned hospitals reporting higher rates of engagement across all domains. I practice in one of the areas that was surveyed and can attest to our paltry performance. The hospitals refuse to share information with independent facilities, and most of the time, my best source of information at the point of care involves the patient handing their phone to me so I can flip through their MyChart account.
The state HIE isn’t much help either since they won’t let individual physicians participate. Physicians only get access if they’re part of an organization that is sharing data. There are plenty of us that are independent, locum tenens, or contract physicians who care for patients outside the walls of a hospital or across multiple rural facilities, and it would be useful to have access to the data when those patients cross our threshold. That’s how the state’s prescription drug monitoring program works – it’s funded by tax dollars and each provider has their own login. Not sure why the HIE needs to be different.

My office recently suffered the devastating loss of a staff member, who passed away at the practice during the work day. It’s been an incredibly difficult time for everyone. The office has been closed and we just re-opened Wednesday. Based on the experience, I have a new item to add to our contingency plans for such a situation. If you have shared PC workstations, I highly recommend having someone log in to the PC that was last in use by the staffer in question and make sure that their login screen isn’t going to pop up for the next person to see. It never occurred to me that it might be an issue until I walked past a staff member who was staring catatonically at a login screen with her departed co-worker’s name, waiting for her password. The whole situation has been traumatic. This was another hurt that the team didn’t need on our first day without her.

Especially in a pandemic, there’s a lot of focus on the clinical workers at hospitals, along with those who perform essential functions such as food service, housekeeping, and facilities engineering. You don’t hear much about the unsung IT heroes, although they’re just as critical where taking care of patients is concerned.
One of my physician friends reached out to me recently about what she perceived as an IT disaster and I had to agree with her assessment. The hospital has had some significant delays in the return of pathology results over the last few months, due to layoffs and backlogged specimens. She’s been waiting for several sets of patient results to return and checking the system daily because she knows it’s a big deal for her patients. The lab director had told her to be patient, but I understand her reluctance to do so when she was waiting for information that could change her patients’ lives.
Late Sunday evening, she received a large volume of pathology results to review, some of which had been finalized and released by the lab more than five days previously. Apparently one of the interfaces had gone down and the results had been available but just sat there queueing until someone finally noticed an issue and pushed them through after restarting the interface. Her hospital recently outsourced quite a few of its IT functions and she couldn’t help but wonder if the changeover had anything to do with the failure, so called for my thoughts. My impression is that of a multi-level failure, first with the interface itself, then with the monitoring systems, then with a lack of notification to the responsible providers explaining the situation.
She had several dozen sets of results to address, but in a system her size, there may have been hundreds if not thousands of patients who were impacted. I know she felt terrible about the delays and was trying to figure out how to find time in a busy Monday office schedule to call notify all the patients. The reality is that on the other side of each one of those pathology results sits a woman who has likely been worrying about the outcome of her biopsy and that failure of the system added additional burden that she probably didn’t need right now.
It’s important for those of us in the healthcare informatics world to realize how critical our work truly is, and for the leadership that manages our departments to make sure we have the resources to do the work properly. My heart goes out to all the patients who had their results delayed and especially to those who received news that likely changed their lives.
Has your hospital cut resources for infrastructure reporting and monitoring? How does it notify patients and clinicians of similar situations? Leave a comment or email me.

Email Dr. Jayne.


Concerning hospitals and HIEs not allowing individual providers access to information in their systems…would this not constitute a form of information blocking? Maybe they could revise their policies by Monday (if the deadline is not extended).
…and hot off the presses this morning, CMS has issued an Interim Final Rule that extends the Information Blocking compliance deadlines until April 5, 2021. Other deadlines were also proposed for extension.
That is a heartbreaking anecdote, Jayne. To make all of the COVID system stress worse, it appears the Russians are currently launching a coordinated attack against all facets of the healthcare system. This seems so deliberately timed to disrupt operations at the point when the rise in cases is pushing our human capacity to the limits. It is entirely possible, even likely, that Americans will die as a direct consequence. How will we respond as a nation? Escalate to your security people immediately if you detect anything suspicious. Watch out for spearphising emails and suspicious links. Almost everyone who reads this blog is a potential target.
https://twitter.com/CISAgov/status/1321620879617478660
https://apnews.com/article/fbi-warns-ransomware-healthcare-system-548634f03e71a830811d291401651610
https://www.nbcnews.com/tech/tech-news/more-hospitals-hit-ransomware-feds-warn-about-cyberattacks-n1245292
https://www.washingtonpost.com/national-security/hospitals-being-hit-in-coordinated-targeted-ransomware-attack-from-russian-speaking-criminals/2020/10/28/e6e48c38-196e-11eb-befb-8864259bd2d8_story.html
Regarding the lab interface being down and no one noticing: I think every internal business user should have the expectation that their internal IT department will monitor functioning of business critical interfaces and similar processes like file transfers and ingestion. If you had outsourced operation of your IT to a vendor, you’d certainly cover things like that in a Service Level Agreement and you’d make plenty of noise if the vendor didn’t meet the SLA. If I was a lab internal customer, I’d ask the IT department 1) Is the interface between the EHR and the lab system monitored by tools for both up/down status and throughput? What are the performance thresholds for throughput that are considered acceptable? 2) Who is in IT is responsible for receiving the alerts from the monitoring tools? 3) What is your requirement for how quickly your people respond to an alert indicating a serious system or interface down condition? 15 minutes? 4) What do you consider prime hours for the lab-EHR interface? 7 x 24 including holidays, or something less than that? This may well lead to lots of defensiveness from the IT folks but they need to do things like this right. Both of my parents have had cancer so I may the person waiting on the biopsy results. This kind of stuff needs to be handled. It’s basic blocking and tackling for a well-run IT department.
Not a hospital admin, but my family has recently been a victim of delayed results due to a similar IT disaster. It became even more challenging when the lab and hospital began blaming each other for the delay. Since these results were the deciding factor to scheduling a critical surgery, I had to channel my best “let me speak to your manager” skills to finally discover that this labs interface to this specific EHR were down (and unknowingly, has been for some time).
This hit a bit different, as I work at Lyniate, an interop vendor, and well aware that it’s typically a standard for a hospital of this size to have some sort of monitoring, notifications, and fail-over to prevent / address these types of issues.
So with that, I agree with the importance to bring more awareness to health informatics and better holistic understanding of the technology available to the department heads. A lot is left at surface-level or boxes being checked, which makes sense if it’s not their key job function. It’s up us and the healthcare IT community to be able to highlight the ranging value from — here’s an interface to get your lab results — to, here’s a solution that helps avoid delays in patient care.