Healthcare data sucks - that song turned my Friday to Friyay!!! Gave me the much needed boost to get through…
News 8/7/19
Top News

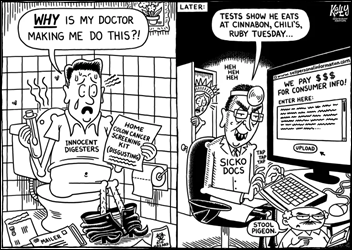
Duke Clinical Research Institute will work with Cerner on a pilot project in which de-identified data from University of Missouri Health Care and Ascension Seton will be analyzed to seek insight on the treatment of cardiovascular disease. The resulting Cerner product will be called Cerner Learning Health Network, which will aggregate de-identified patient data from both Cerner and non-Cerner EHRs.
The project’s results will be published with drug company financial support.
The work will use Cerner HealthDataLab to convert the de-identified patient data into formats that can be analyzed with predictive models and algorithms.
Cerner SVP of Strategic Growth Art Glasgow, who was previously CIO of Duke Health, said in the announcement, “At Cerner, we’re committed to taking four decades of digitized data and transforming it into insights that can help clinicians make more informed treatment decisions. We have an opportunity to use clinical research and data-driven insights to develop an intelligent network of health systems that can truly improve health experiences and outcomes for patients.””
Reader Comments
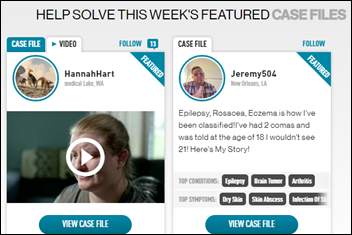
From John R. Brinkley: “Re: ‘Chasing the Cure.’ Any interest in watching it?” The TBS/TNT 90-minute program, which airs live in its Thursday night premiere, features a small panel of doctors that reviews the records of a patient with “unsolvable” medical issues who has submitted their “case file” (a handful of paragraphs of self-description, kind of a Kickstarter for illness, is what is displayed online) ,after which viewers are invited to weigh in using the program’s online community. My reaction:
- I haven’t watched a non-streaming show in many years (easy for me since I don’t watch sports), so I won’t be tuning in. Netflix has spoiled me for being able to watch whenever I want without the intelligence-insulting commercials that take up a third of any program’s time slot.
- I bet quite of the few advertisers are drug companies.
- This concept goes back to the misconception that a bunch of people looking at minimal patient information can be stuck by a “House”-like moment of diagnostic brilliance in figuring out an obscure condition that has escaped their actual doctor.
- People of unstated credentials are already offering advice to the case studies of individual patients on the show’s site, which shows the problem of having everybody and their brother playing doctor from their couches. A woman with joint weakness and pain has been advised to: (a) “eat clean;” (b) get a lumbar puncture; (c) have a contrast MRI; (d) obtain genetic testing; (e) seek stem cell therapy; (f) take a specific brand-name supplement; (g) take B12 shots; (g) get copper and mercury levels tested; (h) have tooth fillings replaced, and (i) try a gluten-free diet. Imagine the plethora of ideas – some wacky and ill-informed, some likely accurate due to a similar experience – that will be offered once the show actually airs. Then a the patient’s real doctor has to waste time sorting out the mess.
- I would prefer having the patient’s doctor review and/or present the case, show the comments of vetted clinicians after the program airs, but display laypeople comments only after the patient’s doctor has reviewed them to make sure viewers aren’t recommending dangerous actions or wasting everybody’s time with bizarre suggestions that stray into “fake news” territory. People with way too much free time who confidently spout bizarre, ill-informed nonsense about everything from politics to unsolved crimes can now give health advice to people desperate enough to make a public plea on TV (note to malpractice and personal injury lawyers – this could be good for you).
- My biggest question is, then what? Even if the armchair diagnosticians eventually turn out to be correct, how does the patient proceed from the show’s airing to resolution? Who’s paying for all the diagnostic work? Does the doctor who couldn’t figure out the problem originally get to explain why they missed it, allowing everybody else to improve?
HIStalk Announcements and Requests
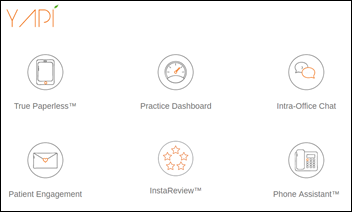
The dental hygienist told me today that she knew that I had arrived for my cleaning and how long I had been waiting because she gets alerts from YAPI, dental practice software that integrates with their Dentrix practice management system. It includes the tablet-based paperless check-in and records update that I had completed upon arrival, a room and patient dashboard that flags patients who are running over or who have waited excessively, team chat, appointment reminders and confirmations, a portal for communicating with patients and checking their appointments, a text message-based review function that routes negative responses to the practice and positive ones to social media, and pop-up patient information displayed with incoming calls from the patient’s phone number. Now I know why I suddenly feel so engaged with the practice, with “send C to confirm” appointment reminders, a follow-up review text message afterward, and not having to explain who I am when I call.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Sales
- Delta Regional Medical Center (MS) will implement MEDarchon’s Quarc for secure messaging and collaboration.
People

Cameron Memorial Community Hospital (IN) promotes Scott Hirschy, RN to CIO.
Announcements and Implementations
Epic will host its second day-long unUGM in Verona on October 3, where C-suite executives of non-Epic using provider organizations can learn how to connect with their Epic-using peers. Registration is open and costs $100.
Optimum Healthcare IT announces the opening of OptimumTech, a Nashville-based IT staffing division.
Other
Eric Topol, MD says in a New Yorker op-ed piece says that doctors need to organize to push back against EHRs, HMOs, and RVUs to improve burnout. He says, however, that the medical profession has been balkanized by the AMA’s decreased influence as members drop out in favor of joining specialty-specific member organizations. Topol discloses that he’s not paying his American College of Cardiology dues because the organization ignores patient needs, functioning instead as “a trade guild centered on the finances of doctors.” He’s also unhappy that medical associations pursue business themselves – the AMA has endorsed products, the American Heart Association “rents out its name” to use its logo on food products, and the American Academy of Family Physicians took Coke money to fund consumer education about its sugar water (he would have a field day with HIMSS). His overriding point is that medicine is being increasingly run by the non-physician bosses of doctors, as the number of healthcare administrators has grown by 3,200% in the past 40 years.
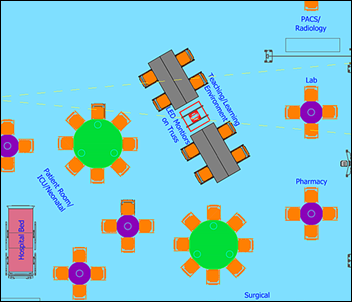
Medical Device Village will open Thursday as part of the Bio Hacking Village of the DefCon cybersecurity conference, expanding from the tableful of medical devices offered in past conferences to a 2,600-square-foot, mocked-up hospital’s radiology, pharmacy lab, and ICU departments full of devices for hackers to attack. A capture-the-flag like competition will be offered and reps from 10 medical device manufacturers will be on hand. The conference also invites attendees to “Bring Your Own Medical Device” for security research.
Psychologists find that while most individuals feel economically threatened when they hear about others losing their jobs to technology, they would actually rather lose their own jobs to impersonal tools like robots and AI instead of having another person take their place.
The Onion weighs in on “Data Dump.”
Sponsor Updates

- The CoverMyMeds team serves meals to families staying at Ronald McDonald House Charities of Central Ohio.
- Artifact Health will exhibit at the 2019 CTHIMA Annual Meeting August 16 in Rocky Hill, CT.
- Burwood Group staff help out at the Boys & Girls Club of San Diego’s annual “Stuff a Bus” back-to-school event.
- Meditech offers its Fall Risk Management Toolkit to users in Canada.
- Fortified Health Security releases its midyear healthcare cybersecurity report.
Blog Posts
- MEDITECH Celebrates 50 Years of Healthcare Technology Innovation (Meditech)
- A Former Nurse Looks Back on the Problems Caused by Paper (Access)
- 5 Overlooked RCM Systems & Processes to Boost Your Bottom Line (AdvancedMD)
- Five Things Your Healthcare Company Should Do After a Data Breach (Fortified Health Security)
- Your top questions on the Radiation Oncology Model, answered (Advisory Board)
- How AI Can Ease the Pressures of MA Risk Adjustment Compliance (Apixio)
- Physician Burnout: A History of the Not-So-Recent Phenomenon Plaguing Clinicians (Spok)
- Quantifying the Value of Contact Center AI (Avaya)
- CarePort Granted Innovator Status by CMS, Creating One of the Nation’s Largest Post-Acute Data Sets (CarePort)
- Recap: American Hospital Association Leadership Summit (Collective Medical)
- Measure Harmonization: Getting in Tune (Diameter Health)
- Remote Work, Is It Right for You? (Divurgent)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.




Again, why is Eric Topol not brave enough to say it? If you are hospital administration, the group that collectively lobbies for you is called the AHA. If you are a small business owner-physician, the group that collectively lobbies for you is the AMA. If you are an employee of either of those two, the group that collectively lobbies for you is called a union. Ask a nurse to explain it to you.
Sometimes, there are no words.
Cerner SVP of Strategic Growth Art Glasgow, who was previously CIO of Duke Health, said in the announcement, “At Cerner, we’re committed to taking four decades of digitized data and transforming it into insights that can help clinicians make more informed treatment decisions. We have an opportunity to use clinical research and data-driven insights to develop an intelligent network of health systems that can truly improve health experiences and outcomes for patients.
Except for this little blip from the same article: The project’s results will be published with drug company financial support.
Every digital health startup and mature market health IT vendor is looking for deep pockets since patients don’t pay, employers remain unconvinced of the value they receive, and providers have spent all their money on Cerner, Epic, and others. Some hope to pick the deep pockets of insurers (in questionably beneficial or promising population health plays), while others hope to sip from the raging stream of drug company (i.e., “life sciences”) excess profits. That’s about the only way a health IT company can pacify impatient investors who are demanding that they scale quickly.
Understood. The “why” isn’t really the shocking part although, maybe for all of the reasons you stated, it should be? I guess let’s wait and see how Janssen Pharma positions the outcomes. At the end of the day, it will be most interesting to see how the insights hold up to peer review, particularly after published.
“de-identified patient data”
We need a law that says that they can’t play around with “re-identifiable data.” At this point we’re all aware that de-identified really means “not immediately identified”, or “you have to put in some work to make identifiable again.” De-identified should become un-identifiable. Of course in order to do that, you’ll probably be destroying whatever value they’re getting out of it. But they shouldn’t get to call it de-identified, it’s still PHI/PII unless mathematically provable that you can’t use that data to get to the identity of the people.
The proliferation of endless databases, online and otherwise, that can be joined together has made “de-identified” a far cry from “un-identifiable.” Much of that matching is performed using date of birth or ZIP code, which could possibly be blurred further by using just the birth year and a broader geographic identifier except in cases where neighborhood environmental impact is being reviewed.
I don’t know if a standard “hard to re-identify” data set has been defined, or even whether every data vendor uses the same fields and formats (and if not, why not?) It would seem that this might be a good role for the federal government given the privacy and commerce implications of just allowing everybody who possesses patient data to publish it however they want and use it in ways that are motivated by profit rather than patients (see: IQVIA and its customers). Researchers like getting the entire medical record, but could get by with skimpier demographic information that would make it harder to re-identify patients.
I’d be really disappointed if the “de-identified” data set contained full birth dates or zip codes. That doesn’t seem to be allowed by HIPAA. From the list of verboten items: (https://www.hhs.gov/hipaa/for-professionals/privacy/special-topics/de-identification/index.html#standard)
“B) All geographic subdivisions smaller than a state, including street address, city, county, precinct, ZIP code, and their equivalent geocodes, except for the initial three digits of the ZIP code if, according to the current publicly available data from the Bureau of the Census:
(1) The geographic unit formed by combining all ZIP codes with the same three initial digits contains more than 20,000 people; and
(2) The initial three digits of a ZIP code for all such geographic units containing 20,000 or fewer people is changed to 000
(C) All elements of dates (except year) for dates that are directly related to an individual, including birth date, admission date, discharge date, death date, and all ages over 89 and all elements of dates (including year) indicative of such age, except that such ages and elements may be aggregated into a single category of age 90 or older”
While we’re at it, I sure hope they aren’t giving pharma companies any data that they don’t make available to the individual patients. Just ’cause, well, fairness & all.
Your observation about the dentist’s system supports what I have found over the years. Since the patient is the payer, even those with insurance, the systems are more customer focused.
Absolutely. I even joked with the hygienist that I wish medical practices were equally concerned about who had checked in and how long they had been waiting. She agreed it was pretty funny that they don’t really seem to worry that you might head off in a huff and find a new doctor. I’m sure it is efficient for the dental practice to send text message appointment reminders with the option to confirm, cancel, or reschedule at least 24 hours in advance to avoid a fee, allowing them to offer the spot to someone else instead of leaving a gap in their schedule. They had already gotten rid of the HIPAA nightmare known as the patient sign-in sheet and it may be that the tablet-based check-in may replace the equally HIPAA-compromising receptionist desk conversation.
This practice, which is far from being boutique in any way, replaced film with PACS before most medical practices and uses the chair-side monitors to show you how your teeth have changed via images and your dental chart, including a new option last time to whip out a pen-sized camera to give me a real-time look into my mouth.