Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…
Monday Morning Update 5/14/18
Top News
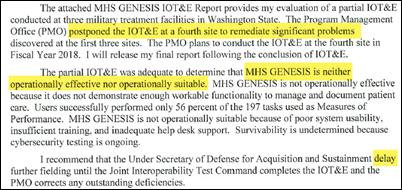
A newly declassified April 30 Department of Defense evaluation of the military’s four MHS Genesis pilot sites concludes that the system “is neither operationally effective or operationally suitable” and says it is inadequate for managing and documenting care delivery.
The DoD’s Director of Operational Test and Evaluation Robert Behler – a retired major general with executive experience in software engineering and consulting — found that the Cerner-powered MHS Genesis isn’t scalable enough for a full DoD rollout. Pilot sites experienced ongoing response time and downtime problems that worsened as each new site was brought online.
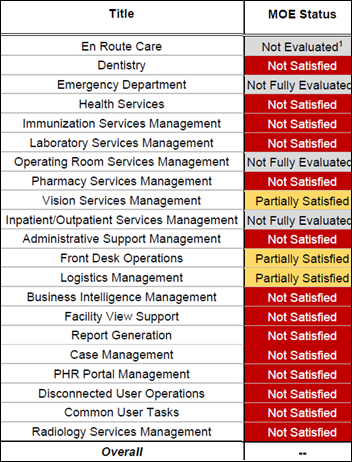
Some items from the report, which was published by FCW:
- 156 critical or severe incident reports were filed.
- Drop-down selection lists include options from all four pilot sites, requiring users, for example, to search through every provider from all four sites to book an appointment.
- User were only able to complete 56 percent of the 197 performance measurement tasks, leading the auditors to report that MHS Genesis “does not contain enough functionality to manage and document patient care.”
- Users questioned the system’s interoperability with medical and peripheral devices.
- Uses rated the system’s usability at 37 on a 100-point scale, far short of the 70 percent minimum target. They also lowered their scores as they gained experience with the system, the opposite of what would be expected.
- Seven long downtime events occurred during the three go-lives, with users unable to log in for hours at a time or one pilot site being down for several hours due to another site’s go-live.
- Help desk personnel were overwhelmed by the 14,000 tickets that were opened from January through November 2017.
- Testing at the largest of the four pilot sites, Madigan Army Medical Center, was postponed because of poor results from the first three sites.
- Prescription fill time at pharmacies increased from 15-20 minutes to 45 minutes or longer and pharmacists had to perform manual workarounds due to interface problems. The system does not support the use of NDC drug numbers or NPI provider IDs, requiring pharmacists to perform manual searches to select drugs and prescribers.
- Providers were unable to review radiology results because radiologists couldn’t match patients to images due to interface problems.
- The Joint Legacy Viewer did not always display critical MHS Genesis patient data.
- The report found that, “Essential capabilities were either not working properly or were missing altogether (e.g., referral requests not processing, lab results not showing, oral surgery apps not launching). To compensate for missing functionality, users relied on lengthy and undocumented workarounds (e.g., telephoning to check whether referrals had been received). Additionally, ineffective or non-existent workflows (e.g., the inability to flag certain patient records, insurance eligibility inaccuracies, appointments tracked to the wrong clinic) caused some users to create their own workarounds. Actions that used to take one minute to complete were taking several minutes using MHS GENESIS. Users reported that, even under conditions of proper functionality, actions required up to three times as many mouse clicks than before. User comments accompanying the IRs and user interviews indicate that MHS GENESIS increased patient encounter times to the point that providers were seeing fewer patients per day, despite some providers working overtime. Users also noted operational incidents (e.g., system freezes, lockouts, login errors) that caused mission failure or delay.”
Politico reports that DoD officials said in a Friday briefing that improvements have been made since the review ended in November, allowing visit and prescription volume to increase significantly. It quotes a White House spokesperson who noted that Senior Advisor Jared Kushner wasn’t involved the DoD’s bidding process but still believes that it’s important for the the VA to use the same system.
Reader Comments
From El Mariachi: “Re: fellowships. I was surprised by your comments. My organization’s fellowship does not require extra application fees, extra dues, or mandatory CE.” I don’t know what AMIA will do with its new FAMIA fellowship beyond requiring AMIA membership, peer recommendation, and AMIA involvement, but HIMSS doesn’t charge applicants directly either upfront or ongoing, although previous HIMSS participation is required. CHIME’s fellowship is attainable only if you’re a CHIME lifer since it requires 10 years of membership plus heavy participation in its activities. AHIMA requires 10 years of HIM experience and previous membership and levies a $250 application fee. All of these fellowships are a combination of loyalty points and industry experience. None of these appear to charge renewal fees or impose mandatory education once the credential has been earned, which I think is unlike medical fellowships such as FACOG and FACC. The terminology could be confusing since scholarship-based “fellowship” and the resulting F-letters to a doctor, academic, or researcher means obtaining additional specialty study and practice, which is vastly different than just sending in a reformatted resume to a membership organization and becoming labeled as its loyal fellow in return. Even more confusingly, AMIA already offers FACMI, conferred by simple voting (17 of those fellow designations were awarded in 2017). The “pro” argument from AMIA is that members who work in a hands-on informatics role should have a way to “celebrate their accomplishments” that are “evident in the settings in which they work.”
From Darth Vader: “Re: EHR vendors. With Elliott making a play for Athenahealth, how long until Optum uses its deep pockets to acquire an EHR vendor?” I would hope that Optum is too smart to spend money buying an EHR vendor in an era of declining product demand, vendor consolidation, and questionable profit potential. It will be interesting to see if Athenahealth sells out to the aggressive (some say ruthless) Elliott Management, stays the course, or entertains new interest from other potential acquirers. Lots of companies have lost fortunes thinking they could crack the code selling EHRs. Probably the biggest financial winner but operational loser in this drama is Jonathan Bush, who owns around $70 million worth of shares (and who would benefit from the company’s change-in-control golden parachute that was enacted in October 2017) but who is in the crosshairs for not making improvements until the activitist investor stepped in and who is now prepared to put his money where his mouth is. Elliott’s challenge would be deciding whether it can leave Bush in charge (he was already stripped of his board chair role because of Elliott’s pressure) since much of the company’s success and identity was the result of his charismatic engagement with Wall Street, customers, and employees. Athenahealth without Bush would be a lot less interesting.
From Alhambra: “Re: the DoD’s analysis of MHS Genesis. It’s impossible to know whether the two competing teams would have performed better, but Cerner is failing in one of the most important areas – Military Medical Readiness. I hope the pause allows Leidos / Cerner to fix this critical component. As for me, I’m ticked that the DHMS PEO PR machine touted deployment and operational success for months and it turned out to be lies.” The people associated with projects, either on the vendor or user side, have a vested career interested in making their work appear to be successful regardless of reality, but the DoD’s scathing review of MHS Genesis is stunning in the extent of the rollout’s problems, even for a huge project like this one. I don’t know how a review could be much worse. Nor could the report’s timing, which comes out just before the VA is set to sign a White House-pressured, no-bid contract with Cerner, which also contains a massive risk that nobody is talking about – the DoD and VA implementations would be occurring simultaneously and thus would compete for resources and vendor attention, not to mention that Cerner would be the VA’s prime contractor versus its role as a subcontractor under Leidos with the DoD. There’s also the unlikely scenario in which the VA signs a $10 billion Cerner contract and then the DoD bails out (note to VA: get that in the contract). VA and DoD technology implementation projects share the common theme of disappointing outcomes despite wildly high costs, a decades-long trend that won’t end any time soon regardless of whether the software is developed internally, by consulting firms, or by commercial vendors.
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor Sansoro Health. The Minneapolis-based company’s API solution provides real-time data exchange between EHRs and digital health applications. Its supports chart retrieval (medical records requests, prior authorization, release of information, quality reporting, risk adjustment); advanced analytics; telehealth; surveillance; and clinical workflow that improves user satisfaction and patient outcomes with intuitive, mobile, and voice-driven interfaces. The Emissary real-time RESTful API solution allows information to be exchanged securely across any EHR platform within days rather than months of setup time while avoiding data-mapping exercises and time-consuming maintenance. It eliminates copy/paste and system toggling to provide a better user experience and improve patient outcomes. Co-founder and CEO Jeremy Pierotti is an industry long-timer, having spent time at Leidos Health, Stanford Health, and Allina. Thanks to Sansoro Health for supporting HIStalk.
This YouTube explainer video describes Sansoro Health’s Emissary API solution.
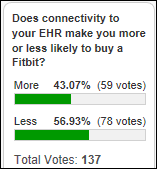
Poll respondents aren’t too interested in connect their Fitbit to an EHR, with comments suggesting a lack of added value and concerns about privacy.
New poll to your right or here: what is your reaction to seeing a fellowship credential such as FHIMSS, FCHIME, or the upcoming FAMIA on someone’s bio or business card?
Responses to last week’s “What I Wish I’d Known Before” question were thoughtful in relaying both good and bad examples of physician participation in technology projects.
This week’s question is for anyone who has worked for a solo medical practice in any capacity.
Webinars
May 16 (Wednesday) 1:00 ET. “You Think You Might Want to Be a Consultant?” Sponsor: HIStalk. Presenter: Frank Poggio, CEO/president, The Kelzon Group. Maybe you just got caught in a big re-org and don’t like where things are headed, or, after almost a year of searching for a better opportunity your buddy says, “You’ve got decades of solid experience and you’re a true professional, you should become a healthcare IT consultant.” Now you start thinking, “This could be my ticket to success. I know the healthcare industry and can show people how to do things right. The sky’s the limit!” Not so fast. Consulting offers many advantages, and many pitfalls. This webinar will discuss both the rewards and the risks of moving into a full-time consulting role, as an independent, or part of a large firm. It will present a checklist you can apply to assess whether consulting is a good fit for you, and present the ground work necessary to be a successful consultant.
May 24 (Thursday) 1:00 ET. “Converting Consumers into Patients: Strategies for Creating Engaging Digital Experiences People Demand.” Sponsor: Healthwise. Presenters: Antonia Chappell, director of consumer solutions, Healthwise; Josh Schlaich, senior product manager, Healthwise. Nearly three-quarters of US adults use a digital channel to manage their health and the internet to track down health information. It’s clear that consumers have come to expect online interactions as an integral part of their overall patient experience. In fact, the Internet may be the first way people come in contact with your organization. They have more choice than ever on where to get healthcare services, and their decisions are increasingly influenced by how well organizations connect with them in the digital space. This webinar will show you how to create engaging digital and web experiences that convert casual consumers into patients and keep them satisfied throughout their entire patient journey.
June 5 (Tuesday) 1:00 ET. “Increase Referrals and Patient Satisfaction with a Smarter ‘Find a Doctor’ Web Search.” Sponsors: Phynd Technologies, Healthwise. Presenters: Joseph H. Schneider, MD, MBA, FAAP, retired SVP/CHIO, Indiana University Health; Keith Belton, VP of marketing, Phynd. A recent survey found that 84 percent of patients check a hospital’s website before booking an appointment. However, ‘Find a Doctor’ search functions often frustrate them because their matching functionality is primitive and the provider’s information is incomplete or outdated. Referring physicians need similarly robust tools to find the right specialist and to send the patient to the right location. Attendees of this webinar will learn how taxonomy-driven Provider Information Management improves patient and referrer satisfaction by intelligently incorporating the provider’s location, insurance coverage, specialty and subspecialty, and services offered that can be searched via patient-friendly terms.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
Spartanburg, SC-based retail pharmacy technology vendor QS/1 lays off around 30 employees in a restructuring.
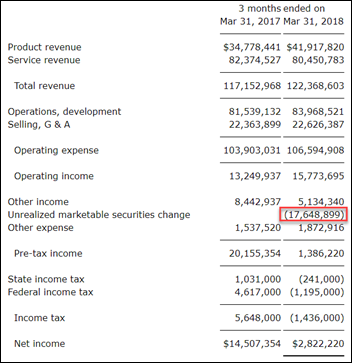
Meditech reports Q1 results: revenue up 4.5 percent, EPS $0.08 vs. $0.39. Product revenue jumped 17 percent quarter over quarter. Accounting changes involving unrealized marketable securities makes comparisons to previous quarters mostly irrelevant – the company’s operating income actually increased by 19 percent quarter over quarter but net income took a major hit due to the $18 million expense entry.
Cumberland Consulting Group acquires EHR-focused managed services firm LinkEHR, expanding its consulting and services offerings into Epic-focused help desk, application break-fix, maintenance, physician concierge support, and build / optimization.
Vision insurer VSP Global makes an unspecified investment in PokitDok. VSP’s innovation lab has been testing PokitDok’s blockchain solution and says blockchain technology will be implemented quickly in healthcare for claims adjudication, supply chain management, and interoperability with EHRs.

Venture capitalist and early Theranos investor Tim Draper says founder and CEO Elizabeth Holmes was “bullied into submission,” adding that he is “thrilled at what she has done” despite SEC charges that the company was a massive fraud from the beginning. Draper previously called for the Wall Street Journal to fire reporter John Carreyrou, whose investigative reporting (“like a hyena going after her”) triggered CMS investigations and sanctions. He also blamed worried competitors and the federal government for causing the company’s problems, saying last week, “I think it was a great mission and she did a great job … We have taken down another great icon.”
Decisions
- Johnson Memorial Hospital (IN) went live with Cerner supply chain management software in August 2017.
- Sagecrest Hospital-Grapevine (TX) will change from a long-term acute care hospital to a short-term acute care hospital by the end of 2018 and plans to construct surgical suites.
- Matheny Medical and Educational Center (NJ) will go live with a Yasasii healthcare information system in May 2018.
These provider-reported updates are supplied by Definitive Healthcare, which offers a free trial of its powerful intelligence on hospitals, physicians, and healthcare providers.
People

T-System hires Steve DeCosta (Research Now) as CFO.

Cedars Sinai hires Anne Wellington (Techstars) as managing director of its accelerator program.
Announcements and Implementations

Intensivists at Western Australia’s Royal Perth hospital will monitor the ICU patients of Emory Healthcare (GA) overnight, exploiting the 12-hour time difference by using Philips eICU remote monitoring.
Privacy and Security
Two California hospitals announce that the information of 900 patients was inappropriately viewed by a former employee of its medical transcription vendor Nuance.
Other
A coroner in Australia urges medical providers to stop using “antiquated technology” after a hospital faxed a patient’s lab results that suggested chemotherapy complications to the wrong number. Without the information the second hospital gave the patient another round of chemo. He died four days after. The coroner couldn’t say for sure that the lack of communication killed the patient, but said it was “difficult to understand why such an antiquated and unreliable means of communication (faxes) exist at all in the medical profession.”

In England, an 88-year-old computer programmer creates Doctor Tick-Tack, an Android app that helps doctors communicate with patients who don’t speak the same language.

A Hong Kong man credits his Apple Watch with saving his life after it warns him of an elevated heart rate, sending him immediately to the ED where doctors diagnosed him with coronary artery blockage that required angioplasty. I’m not sure that the diagnostic power of non-baseline, first-episode, asymptomatic tachycardia is good enough to warrant emergency medical evaluation in every case, but it worked out for him.
GeekWire profiles Seattle-based MultiScale, a joint venture between Providence St. Joseph Health and a life sciences computing vendor whose product extracts EHR data into a secure cloud to allow building apps, creating dashboards, performing analytics, and sharing data with third parties.
Google’s new AI-powered Duplex voice system for making appointments is so realistic that it has raised ethical concerns, forcing the company to add a notice to the call recipient that they are in fact talking to a computer.
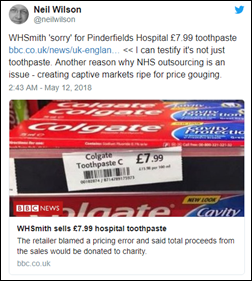
In England, chain bookstore operator WHSmith blames a computer glitch and apologizes for pricing Colgate toothpaste at $11 in one of its 129 hospital outlets, more than triple the price it charges at its other stores. A 2015 BBC investigation caught the company marking hospital prices up heavily on items ranging from bottled water to notepads, reports of which led to government pressure that forced the company to lower prices in its hospital locations.
Sponsor Updates
- Liaison’s Alloy Platform now exceeds GDPR compliance standards.
- National Decision Support Co. will exhibit at the Society for Pediatric Radiology Annual Meeting May 15-19 in Nashville.
- Netsmart will exhibit at the MHCA Spring Conference May 15 in Savannah.
- Clinical Computer Systems, developer of the Obix Perinatal Data System, will exhibit at the NOHIMSS Spring Conference May 18 in Warrensville Heights, OH.
- The Technology Association of Georgia recognizes Patientco with its 2018 Advance Award.
- Pivot Point Consulting will exhibit at the Oregon Chapter of HIMSS 2018 Annual Conference May 17 in Portland.
- Surescripts will exhibit at Centricity Live 2018 May 16-18 in Las Vegas.
Blog Posts
- Executive Spotlight, Kelli Mangino, Community Connect (Optimum Healthcare IT)
- Think Outside the Box to Tackle the Healthcare IT Staffing Crisis (Liaison Technologies)
- 3 Blogs to Celebrate National Nurses Week (Meditech)
- Phoenix Children’s Hospital realized $1M in cost savings with the help of clinical documentation technology (Medicomp Systems)
- Does Your Revenue Cycle Technology Pass the Test? (Navicure/Waystar)
- The biggest priorities for perioperative EHR optimization in 2018 (Nordic)
- How Northwell Health cut claim denials by 50 percent in four years (Experian Health)
- PatientPing Success Story: HCR ManorCare (PatientPing)
- National Nurses Week 2018 – Moments Mean Everything (PatientSafe Solutions)
- Nota Bene – or Not (PatientKeeper)
- HIMSS18 and the future of clinical communications (PerfectServe)
- Let Nurses be Nurses (Qventus)
- HL7 Standards: The Implementation Process, Unique Challenges, and Solutions (Redox)
- Healthcare Artificial Intelligence Outlook: Benefits, Projected Growth & Challenges (The SSI Group)
- Sunquest helps labs respond to healthcare market forces and lab challenges (Sunquest)
- A Training Revolution: Visage 7 Powers UF Health’s SIMulation (Visage Imaging)
- The power of pink pants. (Voalte)
- Inspire, Innovate, Influence: This Is How Nurses Lead (Vocera)
- The Ultimate Checklist for PT, OT, and SLP New Grads (WebPT)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.






Leidos is doing a good job finding a way to make more money for themselves. Tough to screw up that bad.
“It quotes a White House spokesperson who noted that Senior Advisor Jared Kushner wasn’t involved the DoD’s bidding process but still believes that it’s important for the the VA to use the same.”
Happy mothers day
Wasn’ t it a no bid contract? And is Jared now an HIT expert? Just wonderin
The DoD made its selection by bid, with Leidos/Cerner beating out IBM/Epic and CSC/HP/Allscripts. The VA’s proposed contract would be a no-bid agreement using the government’s questionable “only this contractor can meet our very special needs” argument that has spawned a lot of overpriced government projects in the past few years.
Re:MHS Genesis. Is delivery of care really all that different in the DoD than in the private sector? Sure the patients suffer from different issues than at traditional hospitals. But the way care is ordered and documented? I don’t think so. Could it be that Cerner/Leidos quest to customize Genesis to DoD’s spec is what’s causing the failures? I’ve witnessed countless EHR implementation failures because the vendor is too timid to insist on best practice based configuration. I always push to save customization for post implementation, and more times than not the customization isn’t needed. Hard for new users to know what they’re asking for when they don’t know the new system.
With significant health IT tech and project management expertise, both Cerner and the DoD ignored frequent inquiries for any type of involvement.
I am going to stock up on marshmallows and popcorn and enjoy watching the VA / DoD Health IT project burn.
It’s sad that our military and vets are getting screwed.
In response to It’s All Good:
An alternative hypothesis is that most civilian or “traditional” hospitals have or have had the same litany of problems and disasters, but have been mum for innumerable reasons, not the least of which includes contractual obligations.
Might it just be that these problems plagued all deployments but were the public reporting of them was quashed?
Thank you military for drawing attention to these problems.
That’s a sound point. Some/many hospital implementation projects — especially pilot projects — would fare poorly if subjected to rigorous DoD review like this one. Hospitals and vendors have a mutual interest (and sometimes a legally obligated one) to avoid airing their gripes publicly or pointing fingers internally. The point of a pilot is to find and fix problems (software, infrastructure, and training) before a large-scale rollout, so in that regard, the DoD knows what needs to be done, and they built in upfront a lengthy project pause to do exactly that.
“a lengthy project pause” …
Sorry Mr. histalk, but IMHO the issues mentioned in the DoD report necessitate rewriting the base code of Genesis, from scratch.
That may become a lengthy project pause…
But then, I may be missing on your subtler sense of humor and British understatement.
The one-year pause was built into the DoD’s project plan from the beginning — it called for four pilot sites to go live, ending with go-live at Madigan Army Medical Center in October 2017, then a delay of up to a year to have an assessment performed to determine how / if to continue the rollout beyond those pilot sites. I don’t know if this particular report is the independent assessment that was mentioned, but I suspect not since MHS Genesis wasn’t working well enough to evaluate its performance at Madigan (not too surprising since it went live there in late October 2017 and the analysis was performed in November even though the report just came out).
It perhaps should be noted that while Cerner provides the core system, many other vendors, contractors, and systems are involved under prime contractor Leidos. There’s also the issue of scope and project management on the DoD’s end. It’s likely not as simple as saying Cerner’s system is the problem.
Those with long memories will recall the UK’s expensive and failed NPfIT, where the vendors seemed decent enough, the planning was thorough and tough, and yet the project went down in flames with none of the parties involved accepting the blame, leading to the postulate that massive governmental IT projects rarely succeed no matter how much money is thrown at them.
My experiences from the McKesson saga(s) tell me that a C Suite and the VP’s at a hospital who went to the board for the money to install an EHR will do everything in their power to make it work. Going back to the well 3-6 years later to ask for another 10-20 million (or more)with egg all over your face isn’t something that is done unless you are told support will stop on a set date as was the case Horizon. Most of the Paragon shops are right in the wheelhouse for the arranged marriage of an Epic farm out from an academic or larger chain. They can sell it as it will be good for the patients and the hospital instead of owning up to a poor choice or just bad luck that they picked the wrong horse.
Millennium and Community Works aren’t going anywhere soon so with Cerner for non DOD hospitals it’s in for a penny in for a pound. It isn’t just theses mythical gag clauses that keep the bad marriage afloat. Divorce is way too expensive and only happens for those who can afford it or reach a breaking point where they can’t afford not to. The DoD deal for Cerner was like getting married to one of the Karashians. Once it went south like we all knew it was going to there was going to be a very ugly public divorce and there would be vultures lining up to create as much personal gain from picking over the carcass. The new fall season has begun and the production company just got budgeted for 14 new episodes. The worst part of this for Cerner is politicians can now make it look like they are caring for veterans at the same time. That sells.
How come the Cerner Genesis long list of inadequacies took so long to come to the public’s attention ?
Maybe the fact that thousands of physicians, nurses, pharmacists and hospital IT personnel are under either an explicit or worse – an implicit gag clause related to any and all their EHR issues.
While the above is by no means limited to Cerner, from past experience, with Cerner specifically – there was and still is an unfair, unreasonable and unhealthy pressure on hospital employees to shut-up and try to live with the demon…
Yes, you can bring issues up the chain of command, but eventually one either gets tired or gets fired (if persistent).
Finally Cerner met a group of individuals at the DoD, who don’t give a damn about Cerner famous HR hypersensitivity and PC – which usually was used as a way to deflect, delay and postpone any work intended to repair a bug or improve their sub-optimal code…
I can’t see how DoD / VA can move forward with Cerner Genesis – after this report…
The Big Winner here is Leidos which holds the contracts for the DoD in place systems (CHCS the current EMR which Leidos/SAIC says it claims proprietary IP rights and won’t let any other company touch) and other third party applications. Contracts for development, support and sustainment.
So, the Big Whiner is Cerner.
Why? Because it’s in Leidos’ best interest to slow play the DoD as long as humanly possible.
The MHS Genesis project will run horribly over budget and Cerner will take a black eye and whine about it the whole time.
Leidos, like it did with Epic at the Coast Guard, will play the careful edge of maximizing the negative effect of general government incompetence and may occasionally put it’s thumb on the scale should it look like Cerner is close to a break through.
If you review SAIC/Leidos history with the military as a contractor, you’ll see this patter play out well beyond healthcare.
I thought that Cerner milked millions more after the initial contract to host Genesis by Cerner. Did that end up happening? If so, downtimes like the ones listed in the report are embarrassing, pilot or not.
Re Sam Lawrence:
So Yes and No is the answer to your question. Yes, they had to go back to the DoD for I think it was another $60 Million for Hosting services but that was NOT to actually host the entire EHR for the DoD. There are certain parts of Cerner, Like HealtheIntent for example, that have to run out of Cerner’s data centers so that it can be fully utilized. It cannot run in a 3rd Party data center. So, the original language of the contract had some of these “bolt on’s” scheduled to run in the Gov’t Data Centers but it was then realized they could only run out of the Cerner Data Centers.
So, the majority of the new EHR is being held in Government owned/operated data centers and certain parts, like HealtheIntent, are being run via Cerner Data Centers.
I suspect, if there are some hosting issues, it is the Data Centers essentially not talking to each other very effectively. I think people need to remember the amount of Legacy Systems that are still in play here and the 100’s of interfaces that have to be created.
The truth is, we can all bash Cerner as much as we want, and they have earned their fair share of the blame, but the fact is, it didn’t matter who won this bid, we still would have had major issues using a commercial product in the Government arena. At its core, the problem isn’t Cerner, Epic, or any of the actual technology vendors…its the Federal Government, an organization that continues to go unchecked..
It would be interesting to see a similar report on the Epic Scheduling pilots for the VA…
Re anyone getting good money out of HIT takeovers…Reminds me of Vista Equity Partners acquisition of Greenway Health a few years back comes to mind…wonder how well that’s working out for them. They bought them in 2013 and usually sell in 4-5 years at a significant multiple of what they paid. Somehow I doubt that acquisition is working out super well.
Epic is probably counting its blessings at this point. The obvious culture clash aside, makes you wonder if Epic, or any commercial EHR, could have overcome all of the technical challenges. DOD projects are notoriously difficult (see Epic’s USCG project) and this one is proving to be the same.
When I was at Epic, this is why I didn’t want Epic to win the bid. There is no way Epic could’ve gotten the level of control they normally have over the project, which is still (unfortunately) necessary to get decent results. Just look at the amount of agency Epic had with the Coast Guard to have a successful go-live (not). Any failure would be associated with the vendor, even if unwarranted, and the entire thing would be a distraction for them.
Normally, I’d say the issue is less with the software (Cerner, Epic, or other) and more the decisions that were made, but some of the issues described in the report point to a lack of basic functionality. There’s no way Cerner could NOT have the ability to do those things…right? I know their interoperability doesn’t just work the way Epic’s does, but even if we ignore other healthcare organizations, NDC and NPI are very standard. And how can software get more difficult to use with more experience?! That reminds me of jokes about getting dumber after interacting with certain things.
I read through the report again looking for the section on how CommonWell is performing. Turns out, there isn’t one!
Or maybe that’s a section that’s still classified?