Readers Write: The Learning Healthcare System Starts with the Vendor-Neutral Archive
The Learning Healthcare System Starts with the Vendor-Neutral Archive
By Larry Sitka
The Office of the National Coordinator for Health Information Technology, commonly referred to as ONC, recently released “Connecting Health and Care for the Nation, A Shared Nationwide Interoperability Roadmap (DRAFT Version 1.0).” Inside the 166-page framework description, ONC introduces the need for a platform called a Learning Health System, which it defines as “an environment that links the care delivery system with communities and societal supports in ‘closed loops’ of electronic health information flow, at many different levels, to enable continuous learning and improved health.”
The ONC document is designed to be a 10-year roadmap that describes barriers to interoperability across the current health IT landscape, including a description and proposal for a desired future state of healthcare IT. It introduces an architecture overview for a learning healthcare system and what is required of such a system.
In the report, ONC states that “by 2024, individuals, care providers, communities and researchers should have an array of interoperable health IT products and services that support continuous learning and improved health. This ‘learning health system’ should also result in lower health care costs (by identifying and reducing waste and preventable events), improved population health, empowered consumers and ongoing technological innovation” through coordinated care plans.
The report states that in the future, “all individuals, their families and health care providers should be able to send, receive, find and use electronic health information in a manner that is appropriate, secure, timely and reliable. Individuals should be able to securely share electronic health information with care providers and make use of the electronic health information to support their own health and wellness through informed, shared decision-making.”
While the vision and future state put forth by the ONC is sound, as healthcare professionals, we must ask ourselves, “Where do we begin?” and, “What can we do today to begin reaping some of the benefits of interoperability and providing the foundation for the next 10 years?”
As with any technology revolution, certain technologies mature faster than others and begin to provide a glimpse of the future landscape. In the case of interoperability, the vendor-neutral archive (VNA) is a mature technology that is already playing a leading role in evolving the current healthcare ecosystem toward a learning healthcare system and providing a means for real-time healthcare delivery.
The foundation for a learning healthcare system is the basis of what a VNA provides today. Leveraging and thinking of a VNA as merely an imaging storage tool is shortsighted. Why not envision the VNA as providing the pathway and functionality for a patient-centered healthcare discovery tool? The VNA already has the capability to provide an IT interoperability framework that enables many applications to work in unison to learn the context of a patient, inside or outside the current healthcare organization. By leveraging a VNA in this context, suggestive results can be provided to the healthcare organization’s clinicians, physicians, and, most importantly, the patient in a passive or real-time manner.
The VNA is an effective means for improving patient outcomes through interoperability and for moving healthcare organizations beyond the traditional product sell. The ONC report states, “Consumers are increasingly expecting their electronic health data to be available when and where it matters to them, just as their data is in other sectors. New technology is allowing for a more accessible, affordable and innovative approach. However, barriers remain remain to the seamless sharing and use of electronic health information.” The VNA has all the elements necessary to establish a learning health system foundation.
In the construction of a building, every project begins with the foundation. A solid and stable foundation is critical and must be carefully planned. It is the most difficult structural element to change. The foundation of a learning healthcare system is built around two key components—patient context and the healthcare delivery organization (HDO) context. Taking ownership of the data and focusing on HDO interoperability through standards are essential pillars that must be cemented into this foundation.
From an HDO perspective, ownership of clinical content on behalf of the patient is a mandatory requirement. An assumed role of the HDO, on behalf of the patient, is the holding of collected patient content for future use in the continuum of care. The HDO must define and build a foundation by which secure sharing of patient content is inherent. This environment must be capable of not just storing content but also dynamically finding, moving, and distributing content in real time.
This content is linked and possibly moved into a learning healthcare system independent of the organization’s affiliation. The content is either linked on demand or covertly as information is discovered, further extending the patient longitudinal record. The goal of content aggregation is to provide suggestive access to patient information for the healthcare worker who is responsible for delivering a better patient outcome. The patient outcome is the evidence by which the HDO shall be paid.
From the patient perspective, ownership of the data by the patient is now something we vendors must enable and that HDOs are legally bound to steward. HIPAA, for example, can appear to vendors as restricting and controlling. It attempts to define who and what content can be accessed along with the purpose of accessing that content. However, it is actually HIPAA that finally gives ownership of the content back to the patient. It is the first piece of legislation specifying to the HDO and its vendors that true ownership of results and supporting documentation belongs to the patient and not the healthcare organization, the insurance company, or the product vendors.
Once the foundation of a learning healthcare system is created, the framing comes next. Framing requires exact measurements and sizing using standards-based products. With the cutting and coercion of the materials comes a custom fit per the requirements in a blueprint. Such is the case of a learning healthcare system, where the HDO must begin by demanding standardization of not only structured content but also unstructured content. Standardization assures interoperability and a canonical data model that is based on industry standards and site-specific requirements, not proprietary vendor specifics. Standardization or canonicalization of the metadata to be used and exchanged in a learning healthcare system is exactly what a true VNA platform provides.
Simple problems come with very complex solutions in these cases. For example, patient names, IDs, and study descriptions have become as complex to the HDO as the Y2K problem. Can you imagine the chaos that would ensue from an IT infrastructure not based on wireless or Ethernet standards for physical connectivity? Simply put, what if we all drove on an Interstate without painted lines? What if the map we used for guidance did not include a legend?
Such is the case for the HDO when it comes to delivering a standards-based form of patient content. Of course, there are DICOM standards, HL7 standards, and the XDS framework, but HDOs must demand that vendors actually support and utilize these standards, participating in annual Connectathons to validate their ability to interoperate. More importantly, HDOs must contractually demand interoperability following those exact standards. In short, an HDO must stop purchasing solutions that are unique to its own internal, proprietary standards.
The deployment of the electronic medical record (EMR) to capture and attempt to hold unstructured content, at least inside a data warehouse application, is a step in the right direction. Unfortunately, the EMR only solves half of the problem by providing a collection point. To test this, try and share the unstructured content between EMRs and between organizations. This has become a next-to-impossible task. EMR providers that claim to be able to share unstructured content typically come up far short of expectations.
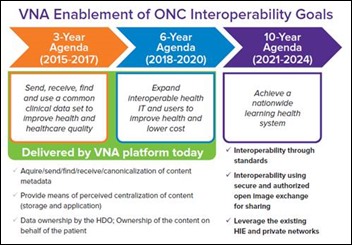
The idea of sharing an electronic record is what initially drove EMR adoption. But now we have a large volume of unstructured content that must feed the learning healthcare system. The VNA is a capable platform for achieving this goal. The chart above indicates where the VNA is already meeting three-year and six-year interoperability objectives set forth in the ONC report.
The final steps in a construction process are completed by selecting the best products, with the best look and feel, to meet the needs of the owner. Such is the case in creating a learning healthcare system, which demands the ability to select the best products and functionality to deliver the best patient outcomes. Different departments and healthcare settings, much like physicians, have different needs and requirements. Why be limited to only one selection? More importantly, don’t be forced into “one size fits all” in the selection of applications. Give HDO users the flexibility to select the applications that best suit their workflow and objectives. For example, a radiology-centric viewer will not work very efficiently for wound care or treatment planning.
When connecting the building to the outside world, each location typically has its own utility providers that are part of a grid. The same is true for a learning healthcare system, where existing healthcare information exchanges (HIEs) are the on-ramps. The HIE and image or content exchange, which are typically not profitable today, are expected to evolve into much more in the future. Difficulties often arise when seeking cooperation among different, unaffiliated organizations for patient informational access. Vendors, of course, find it difficult to build any product today around something that is not profitable, not to mention being a very difficult sell to HDO executive teams. Tomorrow’s HIE technology inside the learning healthcare system, however, will not only be a necessity but will be integral in making sure image and content exchange is included in the VNA as an embedded feature. Sharing patient content across the private sector, HIEs and government organizations will become commonplace within the next decade, all driven by patient outcomes.
But, more importantly, the business and legal perspective. The VNA selected should support an HIE inherently. An image/content exchange is a mandatory requirement of a VNA and is the basis of a learning healthcare system for moving released content in a secure manner. It is also critical that an image/content exchange within a learning healthcare system provide the business process and verification steps, including automation of steps that include BAA approval and appropriate patient release form access and approval.
The data demands of a learning healthcare system will far exceed anything an HDO has seen to date. Typically, the sizing of a VNA is done by traffic volumes requested by concurrent users, or study volumes. However, the oncoming big data analytics applications (a necessity inside a learning healthcare system) will far exceed any current traffic volumes requested by humans. A learning healthcare system will be in a continuous mode of finding, aggregating, and coercing information relevant to the patient in context. This is also a necessity to building out the patient record.
Once found, the information is persisted in the learning healthcare system whereby the analytics and other applications, including natural language processing (NLP), will access the information. NLP will give the data better context and perception around the patient, allowing the healthcare worker to have better informational access and decision processing through new clinical support applications. Support for these demanding applications will require an infrastructure that can scale on-demand, both horizontally and vertically. These applications will leverage your VNA for more than just “basement storage,” where content becomes cluttered and inefficient while never being used again.
The learning healthcare system will be an integral part of improving the way the healthcare ecosystem works and how patients, providers, and payers interact within that ecosystem. Achieving the complete vision of the learning healthcare system will be a gradual process and lessons will be learned throughout the journey. There are important actions we can initiate today, however, to begin building the necessary foundation for this vision. VNA technology is the foundational cornerstone mature enough to begin solving some of the greatest challenges and to remove some of the obstacles to a fully interoperable healthcare system.
Larry Sitka is principal solution architect with Lexmark Healthcare of Lexington, KY.



Sounds reasonable, until you look at the Silicon Valley experience. Silicon Valley grew like a weed precisely because employees could…