Monday Morning Update 5/5/14
Top News
Blue Cross Blue Shield of North Dakota partially blames its poor 2013 performance on newly implemented EHRs of providers that delayed their insurance claims submissions, which it says caused it to underestimate the value of those claims. I didn’t realize until reading the CEO’s discussion that Noridian Healthcare Solutions is a subsidiary of BCBS of North Dakota. Noridian built the failed Maryland health insurance exchange and was fired from its $193 million contract in February. Maryland has hinted that it may sue Noridian in hopes of getting back some of the $55 million it has already paid toward Noridian’s five-year contract. North Dakota’s insurance commissioner says the agency is watching BCBSND to make sure it doesn’t try to increase insurance premiums in the state to cover Noridian’s projected $17.8 million loss. Every time I hear that name I think of Veridan Dynamics from “Better Off Ted.”
Reader Comments
From Guillermo del Grande: “Re: CIOs. Here’s a list of “A Few Things CIOs Should Know (Or Think About).”
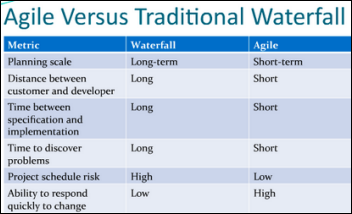
- If you want the FDA to regulate EMRs but have a service level agreement of two days for major fixes, you may want to learn about software development models. If you have to ask what a software development model is, how did you get to be a CIO?
- FDA requires waterfall development. This is not Niagara Falls.
- How many of the good EMRs use waterfall any more? Here’s a hint: not many. Most are agile. EMRs are more complicated than a medical device. How many different medical devices connect to your EMR? Do you even know? Do you feel like testing every scenario per medical device that connects to your EMR? Do you think your vendor does that?
- Are you afraid to let developers and your IT people watch healthcare and the software in action? You’re not agile. You’re going over the waterfall in a barrel.
- If your SLA is two days, but you require a change control meeting that only happens every two days, and then a software testing process that takes two days, and then another change control meeting, and then only migrate changes once a week, you may have a problem.
- How long does it take your vendor to fix a minor issue? You should be asking this question before you buy.
- What makes you think your IT staff can fix a problem in a SLA period when you don’t know if it’s something your IT folks can do or it’s something the vendor has to do?
- Do not try to manipulate an IT staff or a vendor into repairing your highest priority by only reporting that item. IT staff have lots of end users. Vendors have lots of customers and sometimes will fix issues only if lots of different customers are seeing them.
- If you think a problem made it to the field because the software testers at the vendor didn’t find the issue, you don’t know much about how software companies. Remember that story about the guy who had his heart burned out of his chest a few years ago because of a bug? If not, look it up on HIStalk — it was a known issue for 10 years. Ask your vendor how many known issues they have in their tracking system. Hint: they’re not all reportables.
- The Supreme Court is reluctant to take new cases and software developers are reluctant to fix bugs for many of the same reasons and use some of the same processes.
- “Not a customer workflow” is heard at many a vendor to defend not fixing a bug, often before there are any customers.
Thoughts on FSMB’s “Model Policy for the Appropriate Use of Telemedicine Technologies in the Practice of Medicine”

The Federation of State Medical Boards is a Euless, TX-based non-profit trade association that represents all US medical boards that license physicians. It does not make regulations directly, but state boards usually adopt its recommendations.
Key points from its report include:
- Telemedicine is defined as requiring videoconferencing. Encounters conducted via telephone or email are not telemedicine.
- Physicians must be licensed in the state “where the patient is located” because physicians are licensed by individual states.
- A physician-patient relationship must exist, but it can be established using telemedicine technologies.
- The physician must document the patient’s history. Having the patient complete an online questionnaire doesn’t count.
- The physician should obtain the patient’s informed consent, including a description of the security features of the telemedicine technologies being used.
- The physician must make themselves available following the encounter.
- The physician may not promote services for which they are receiving payment or benefits.
The intention of the group is clear. It wanted to prevent providers from selling prescriptions online. Nearly all of the wording restates requirements that are already in effect for traditional physician-patient encounters, clarifying that those requirements hold true for telemedicine-based encounters. The policy attempts to prevent online-only practices by prohibiting misleading websites, undisclosed financial relationships, and running an online consultation service simply to sell drugs online.
The only significant (but unsurprising) recommendation is that physicians must hold a license in the state where the patient is physically located during the encounter. That also is no different for traditional medical practice – an ED doctor in Florida can see vacationing patients from anywhere in the world from a Florida-based hospital, but he or she can’t travel to those other states to treat the same patients at their homes unless licensed there.
The most positive development for telemedicine supporters is that the model policy allows patients to be managed entirely by telemedicine without an in-person component.
The negative aspects of the model policy are:
- FSMB isn’t a particularly transparent organization and didn’t disclose the members of the work group or who it consulted to develop its proposed policies. It also did not provide a way to incorporate industry or patient feedback.
- Doctors already diagnose and treat patients by telephone and email, but those options are not considered telemedicine in the model policy, although it doesn’t limit or prohibit them. That would suggest that nothing changes for those visits, although future questions may come up involving payment for services.
- Doctors must be licensed in the state where their patients are located, which isn’t even accurate in some cases (military physicians.)
- It doesn’t address the desirability (nor should it have, most likely) of national rather than state-by-state licensure of physicians or an expanded reciprocity program that would make it easier to practice across state lines. That’s the biggest clash between telemedicine proponents and state regulatory boards, whose revenue and power come from overseeing in-state professionals and (arguably) protecting them from competition.
- It calls for requirements that exceed those of non-telemedicine encounters, such as prohibiting randomly assigning patients to physicians (which EDs, walk-in clinics, and other services do routinely) and requiring that the medical records of patients be reviewed before treating them (which urgent care providers can’t do by definition.)
The conclusion is that telemedicine proponents wanted a policy that opened up state borders and encouraged innovative care, while FSMB’s goal was to prevent unethical doctors from running pill mills and online medical scams.
HIStalk Announcements and Requests
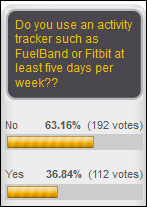
A commendable 37 percent of poll respondents use an activity tracker at least five days per week. New poll to your right: should doctors be licensed nationally instead of state by state? It’s an important question if you think telemedicine can improve the efficiency and geographic reach of physicians.
Thanks to the following sponsors, new and renewing, that recently supported HIStalk, HIStalk Practice, and HIStalk Connect. Click a logo for more information.
Upcoming Webinars
May 7 (Wednesday) 1:00 p.m. ET. Demystifying Healthcare Data Governance. Sponsored by Health Catalyst. Presenter: Dale Sanders, SVP, Health Catalyst. Challenged with governing data? This vendor-neutral discussion will cover the need to develop a data governance strategy, including general concepts, layers and roles, and the Triple Aim of data governance (quality, literacy, and exploitation.)
Acquisitions, Funding, Business, and Stock

Vocera announces Q1 results: revenue up 10 percent, adjusted EPS –$0.14 vs. –$0.07, beating expectations for both. VCRA shares were the second-largest NYSE percentage losers on the news, shedding 14.7 percent. From the conference call:
- The company released the Vocera Collaboration Suite and an expanded Vocera Care Experience in the quarter.
- It opened a development shop in India.
- President and CEO Brent Lang called hospital spending “challenging” as hospitals wait to see where changes in patient population and healthcare reform go.
- He quoted a report that says 97 percent of hospitals don’t believe their nurses have the right tools to determine the availability of caregivers and that consumer-grade smartphones aren’t working well for hospitals.
- Lang mentioned a tentative US Army study in which use of Vocera’s system provided a 12-month payback.
- The alarm management system it gained with its mVisum acquisition in January 2014 will be launched this summer.
- Lang said the company will pursue more acquisitions.
Evariant, which offers a patient marketing platform, raises $18.3 million in a Series B funding round.
Hc1.com says it will create 175 jobs in central Indiana over the next five years, having just received $3 million in state tax credits. I can’t really tell what the company is selling since the site is a mess of buzzwords and vaguely feel-good statements behind one of the worst company names I can imagine (shades of 1999), but it seems to be a customer relationship management system for outreach labs and radiology practices.
General Dynamics will lay off at least 645 Utah-based call center employees it had hired under a CMS contract to take Healthcare.gov related inquiries about insurance.

CPSI announces Q1 results: revenue up 5 percent, EPS $0.69 vs. $0.63. From the conference call:
- The company installed financial systems in nine hospitals and clinical systems in 12.
- Add-on sales made up 26 percent of total revenue
- The company expects to gain ground with MU Stage 2 as “a number of our competitors continue to struggle with obtaining certification for their software, as well as struggling with the installation and usability of their software in the small hospital market.”
- Its new ED module will GA in Q3.
- CEO Boyd Douglas says that while Epic and Cerner talk about moving into smaller hospitals, CPSI isn’t seeing much of that, mostly just their usual small-hospital system competitors (Meditech, McKesson Paragon, and Medhost, I assume.)
- The Leerink Swann analyst managed to say “sort of” four times in one question, also using that annoying verbal crutch twice in a follow-up question.
Sales

The Defense Health Agency awards Leidos a $70.7 million, sole-source contract to support its EHR systems for the next 11 months.
Nashville-based MindCare Solutions signs the first customer for its tele-behavioral platform and provider network, Genesis HealthCare, which will offer remote psychiatric services to its 400 skilled nursing facilities.
Announcements and Implementations
New York State Immunization Information System will use Blue Button to make records available to the parents of patients.
AMIA calls for nominations for its 2014 awards for informatics leadership, nursing informatics, informatics health policy contributions, and informatics innovation. Winners won’t necessarily be the best, just the best who pay AMIA dues: a key selection attribute is “demonstrated commitment to AMIA through membership.”
The Boston Business Journal profiles Alere Accountable Care Solutions, mentioning that it will offer its care management, connectivity, and analytics systems in Europe. I interviewed CEO Sumit Nagpal in October 2013.
Government and Politics
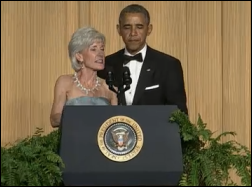
President Obama makes fun of Healthcare.gov at the White House Correspondents Dinner on Saturday, saying that he has replaced his campaign slogan “Yes We Can” with “Control-Alt-Delete.” Near the end of his presentation, he pretended to have problems with a video and former HHS Secretary Kathleen Sebelius got a cameo as she rushed to the podium to fix it. The President’s last words of the evening, after thanking the press and uttering the obligatory “God Bless America,” were “Thank you, Kathleen Sebelius.” Other than following the party line, I question whether the fired Sebelius did anything worthy of that level of adulation.
Other

A Minneapolis cardiologist, intrigued by the use of scribes in the ED, tries them in his cardiology clinic. The four doctors he studied were spending all but two minutes of their average 13-minute patient visit working on the computer. Turning that work over to scribes shortened the visits to nine minutes, but beyond that efficiency gain, patients got seven minutes of that as face-to-face time, nearly four times as much compared to non-scribe visits. The doctors saw 60 percent more patients using scribes, boosting revenue by $206,000 in 65 clinic hours. Patient satisfaction was unchanged, which is nice for making a case for scribes but not so nice for the doctors — all that extra face time apparently didn’t impress patients.

Dr. Andy’s HIStalk Practice rant on the problem list is drawing interesting comments from his physician peers. Example: why can’t the problem list attribute cause and effect, or allow attaching meds to specific problems (or more than one problem?)

The dean of the new Dell Medical School at the University of Texas (I wonder who paid for that?) says that while Austin is behind in a competitive biotech industry market, “Areas like digital health and informatics, no one owns that right now. That is an area that’s rapidly growing and ultimately it will win and be a huge area … Companies who handle personal data see that health is a huge frontier and represents a huge economic engine, but no one has been able to innovate the platform that scales to a huge field … There are companies waiting to do that, but no one is inviting them in. We can do that.”

Mineral Community Hospital (MT) reports to its board that its NextGen implementation resulted in unplanned upgrade-related downtime and a 45-day delay in sending bills out for the 25-bed hospital.
A man Googling for CPAP machines for his sleep apnea notices that unrelated Google searches start displaying ads for those devices, leading him to complain to the Office of the Privacy Commission of Canada that targeting ads based on a health-related search constitutes a privacy violation. The office agrees after an investigation, determining that the practice not only violated its advertising guidelines, it also violated Google’s own policies that state the company won’t use health-related browser cookies to target ads. Google blames some of its advertisers and says it will improve its training and monitoring programs.
New York State Insurance Fund blames a software upgrade after the medical records of 20 worker’s compensation patients are to the wrong attorneys.

Bizarre: a mother is awakened by the sound of a man’s voice in her sleeping 10-month-old daughter’s room screaming, “Wake up, baby.” She runs into the room and sees the camera of the video baby monitor turn toward her as the hacker who is controlling the camera starts screaming obscenities at her. The woman’s Foscam IP camera had been updated to fix a security flaw, but she didn’t know about it. The conclusion is that the Internet of Things will give hackers a lot of household (and hopefully not hospital) gadgets to play around with.
Sponsor Updates
- The Health IT Quality Solutions Program of Quest Diagnostics certifies iPatientCare’s EHR as a Silver Quality Solution.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.

















I'd never heard of Healwell before and took a look over their offerings. Has anyone used the products? Beyond the…