Neither of those sound like good news for Oracle Health. After the lofty proclamations of the last couple years. still…
Monday Morning Update 9/13/10
From Slinky Nighty: “Re: JPS in Fort Worth. They have definitely chosen Epic. They attended the Epic Texas Collaborative meeting this past quarter and are moving forward and looking for assistance.” Thanks for both the info and the name imagery.
From Old IS Person: “Re: Siemens. They’ve started a second help desk for radiology and PACS products, so those of us with multiple products are supposed to use two different systems just to report problems.” Don’t get me started on vendor help desks. Like the one from one of our key vendors who brags on how fast we’ll hear from an analyst, but it takes days to weeks to get anything other than the automated e-mail response that says “I have your case and I’ll get to it when I get to it” (I’m paraphrasing slightly). Not that it really matters since 90% of the time, the answer is, “Oh, we know about that problem and it’s on development’s list,” which paraphrases into, “It’s kind of a pain for us to fix that, so we’ll just add it to an Excel worksheet that nobody ever looks at.” Do some of the issues vendors ignore in this way endanger patients? No question. I bet if they were forced to go public with their open issues list they’d be a lot more responsive.
From Tupelo Honey: “Re: CPHIMS. I got an e-mail from HIMSS asking them to send me a glowing letter about all that having CPHIMS has done for me, which is mostly nothing. I am guessing that not so many people are signing up or renewing.”
From The PACS Designer: “Re: OpenMRS. TPD has posted about the third world medical record system called OpenMRS and how it was being used in Uganda, where Brigid O’Gorman is presently trying to educate their countrymen. Now they have improved their Web site and expect to release a new version OpenMRS 1.7 soon.” I noticed they’re having their Implementers Group Meeting in Cape Town, South Africa this weekend (group pic above).
From EHR Geek: “Re: HISsies. PLEASE do those again! The ones you posted today are still relevant and hilarious! ROTFL!” Thanks. I’ll try to crank out some cynically funny stuff again since I miss doing that, although someone always complains if I write anything that isn’t just a bullet list of facts addressing only those precise news stories that interest them personally. Meanwhile, you can check out the 2006 HISsies recap or one of my phony news items, of which here are a couple for old times’ sake.
HIMSS Announces 2008 Conference to Be Held in Baghdad
(CHICAGO, IL) HIMSS has announced that its 2008 Annual Conference & Exhibition will be held in Baghdad, Iraq, following a successful 2007 stop in New Orleans. Steve Lieber, CEO of HIMSS says that HIMSS has learned that it can benefit disaster-stricken cities by flying in planeloads of attendees with large expense accounts, a concept first tested by bringing conventioneers to New Orleans shortly after it was virtually destroyed by Hurricane Katrina. "We’ve proven that we can all have a great time at a site mostly known for death, civil disorder, and senseless violence. We’re going to have a blast in Iraq, no pun intended," said Lieber. HIMSS sources indicate that the surprise speakers for the "View from the Top" session may be Saddam Hussein, Donald Rumsfeld, and Neal Patterson.
Hospital Trainer Collapses During Class
(DAYTONA BEACH, FL) Todd Cleaver, a 41-year-old computer trainer at Halifax Hospital, was stricken this morning with an apparent heart attack while leading a computer class for nurses. He is reported in stable condition and is expected to recover. Debbie Dallas, a registered nurse attending Cleaver’s electronic clinical documentation course, said he was working with her one-on-one when he collapsed. “He was starting to tell me how to make a flowsheet entry and I just reached over and did it correctly. Then, he was going into switching between Windows tasks and minimizing windows, and I showed him I could that, too. That’s when he went down.” Cynthia Roda-Tiller, education manager for Halifax, says she believes that Cleaver suffered a strong physiologic reaction upon seeing a nurse use a computer intuitively. “Usually they just stare at the screen like it landed from Mars or they start clicking everything in sight like it was Whack-A-Mole. You’re thinking, ‘they let you use medical equipment?’ I’d like to think I could have handled it myself, but it’s making me shake even now. I’m not sure I even believe she’s really a nurse, at least not one I’d want working my bedpan.”
Somebody must have gotten to the Forbes writer who wrote a generally negative article called Bribing Doctors To Go Electronic. Its implications: North Shore-LIJ and Allscripts are struggling with their $400 million to implement EHRs for 9,000 doctors, it’s taking doctors longer to get their work done, they’re pawns of the government, EHRs are a tough sell culturally, and community docs don’t like hospital-hosted EMRs because they don’t trust hospitals. Careful readers may have noted that he talked to a grand total of two docs (both recently implemented) in writing the lengthy piece. Now he’s backing off in a mea culpa that says he wasn’t trying to write a definitive article on the value of EMRs and that those complaining early adopters recognize their value because they volunteered. I guess the two pieces cancel each other out, other than the time it took to read both.
As New York, Nashville, and Cleveland race to book tenants for their medical trade center buildings, the Nashville group says it’s not worried despite not signing anyone except HIMSS for its 1.5 million square feet of space scheduled to open in 2013. Reason: it says HIMSS will bring 85 to 125 companies to lease space in their building, with a handful taking up to 15,000 square feet.
Hey, it’s only $20 million, which is a HITECH rounding error, but ONC throws more money at RECs, this time as a little extra to help critical access and rural hospitals.
Stanford’s Lucile Packard Children’s Hospital appeals the $250K fine levied by the state’s health department when the hospital waited 11 days before reporting a stolen PHI-containing laptop. They fired the employee who took it home against policy.
Ivo Nelson, chair of Encore Health Resources, joins the board of Health Care DataWorks. That’s the Ohio State spinoff whose CEO is former OSUMC CIO Herb Smaltz.
The Bethesda Hospitals’ Emergency Preparedness Partnership (Hopkins Suburban Hospital, National Naval Medical Center, and NIH) chooses Versus Advantages RTLS for patient tracking in emergency care areas during mass casualties. The Versus product met its requirement for 95% accuracy down to the room level and also links patient information to location for emergency responders.
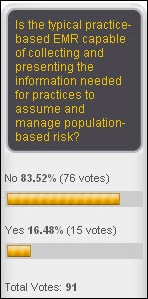
Not many folks think that the average EMR will give providers enough information to manage population-based risk. New poll to your right: if you were filling a position, what impact would a candidate’s CPHIMS credential have on your decision? Tupelo Honey wants to know.
Ken Rardin, former CEO of Merge Healthcare, IMNET Systems, and a couple of non-healthcare companies is named CEO of telemedicine provider REACH Call of Augusta, GA.
This could make a an interesting novel: the former CFO of Danbury Hospital pleads not guilty to scamming the hospital by approving phony invoices for contract management software from a software company he ran from his house. He adds witness tampering and harassment to his list of charges after e-mailing the hospital president begging him to make the charges go away despite a hospital-requested court order to keep him away for fear he would go postal. He closed his plea with, “I got no place else to go (quote from An Officer and a Gentleman)” The judge nearly put him back in jail for that, but the man’s attorney made a convincing argument: “He would have to be a total idiot to do this again.” Ever the CFO, he showed up in court with a sports coat over his jail coveralls.
One of two winners of IBM’s SmartCamps start-up competition: CareCloud, a Miami company offering physician practices a $499 per-doc-per-month practice management system with social networking thrown in and revenue cycle services optional. I’ve mentioned the company a few times previously when they won an award and were pitching at the Health IT Venture Fair at HIMSS. Points off for their latest blog entry extolling the virtues of Twitter, which they summarize in a grammatically incorrect manner as, “… us enlightened folk know that the conversations on Twitter are insightful and illuminating.” They must be living in an alternate Twitterverse than the one I’ve seen, which combines the worst aspects of text messaging and Facebook but at least allows only 140 characters of time-wasting, stream-of-consciousness preening (if they would ration the number of tweets like they do the number of characters, they’d be on to something). Do we really need to hang on the every un-profound word of vapid celebrities, self-appointed pundits, and a guy having a heart attack?
Here’s another example that healthcare is different when you have money: a new startup called ExpertConsensus will take your tough medical problem to a group of big-name doctors who will teleconference and make their collective recommendations. The company’s minimum charge: $20,000. I hated that concept until I thought about it: they’re offering convenience for those willing and able to pay, but patients on a non-$20K shoestring could find these docs on their own and pay just a consultation fee to get the same opinions (or pay Cleveland Clinic a few hundred dollars for an electronic second opinion, which I can’t believe isn’t more popular than it seems to be). ExpertConsensus offers other services seemingly unrelated except for their common denominator of buck-making opportunity: research reports, care management, on-site clinic setup, physician referrals, wellness, and personal health records.
Louisiana doctors will have to pay back $17 million in Medicaid overpayments because the state’s Department of Health and Hospitals just now got their computers programmed to handle budget cuts that went into effect 13 months ago. Said one doc who says the cut will put him out of businesses, “We’ll gut it out and when it’s obvious that we aren’t making ends meet, we’ll all retire.” I need to give docs some PR advice for those situations where they’re complaining about making less money: don’t say “retire,” but instead say “find another line of work.” People hearing “retire” assume that means you’ve milked your medical practice to the point of not needing to work any more, which doesn’t exactly bolster the “we’re poor” argument.
Interesting: doctors at McGill University in Montreal administer anesthesia electronically for a surgery being done in Italy, a pilot project for “teleanesthesia”. They managed the patient using video cameras and remote dosing computers that make up what they call “an anesthesia cockpit.”
I’ve written before about the UK’s hospital radio stations, charities run by volunteers and featuring patients and family requests. London’s Radio Marsden, which runs 24 hours a day for patients in two cancer hospitals, will move its service to the Internet this month to allow patients, friends, and families to listen together. I’m listening to Bowie’s China Girl on it right now, followed by the Talking Heads doing Burning Down the House and an announcers’s suggestion that patients ask for hospital pens and paper to write letters home. Hot on their playlist based on patient requests and favorites: Lady GaGa, 30 Seconds to Mars, Alicia Keys, Kinks, Billy Ocean, The Clash, and The Saturdays, among others. It’s kind of addictive.
Former Sun CEO Jonathan Schwartz, who replaced Scott McNealy for a short time before selling the company to Oracle, gets involved with a healthcare-related startup, Picture of Health. He’s not saying what the company will do.
A hospital ED patient is arrested for assaulting another patient and then pulling a knife on an ED nurse. The man’s occupation: minister.
A Mr. H Book Review
Safe Patients, Smart Hospitals
By Peter Pronovost, MD, PhD and Eric Vohr
A reader asked me to review this book, so I bought a copy. I interviewed Peter a couple of years ago, before he won the Genius Grant. It’s still one of my favorite interviews, with this as my favorite quote from it:
That’s the tension that we have. How much evidence do I need to give up my autonomy? We’re still uncertain about that. As an industry, healthcare is grossly understandarized. Compare that to pilots who have to use checklists or they won’t be flying. Healthcare is still very much like the Wild West or like Chuck Yeager in The Right Stuff, where we have this cowboy mentality and we’re just beginning to accept that standardization is a key principal to making care safe.
That frames up the book nicely.
My first thought when seeing the book (published just this year) was, “Hey, I get it, providers need to make lists … why do I need to buy the book since I already know the ending?” There’s a lot more to it than just making lists, however. The book is really about translational medicine, rigorous measurement of healthcare quality, and the patient harm caused by the toxic culture of hospitals and physicians. Here are the takeaway points.
- Doctors and hospitals harm patients because of poor communication, not following rules that are indisputably beneficial to patients, and not using proven research in their treatments.
- Culture dictates that doctors and hospitals pretend that they don’t mistakes and to avoid admitting them when they do.
- There is no wisdom of crowds in hospitals. Doctors are trained to be sole decision-makers and to lash out if anyone questions their decisions. Not to mention that Peter’s background is in academic medical centers, where the problem is tiny compared to community hospitals with their non-employed doctors who are always complaining to administration and trying to get employees fired for looking after the best interests of patients.
- In terms of communications, even on his own rounding team, only 5% of residents and nurses could articulate the care goals for a patient who had just been the topic of a 15-minute team discussion. You wonder what they would have concluded without the team discussion and armed only with a paper or electronic medical record, given that academic medical centers are a small percentage of hospitals and others don’t do that kind of rounding at all.
- Overworked doctors will break rules for a single patient if they think the greater good is served. Every doctor knows to wash their hands before and after seeing each patient, but only 30% actually do it because they’re busy or supplies aren’t available.
- Communication in the OR is especially bad, where the nurses know everybody’s name but the surgeons see just a sea of scrubs and have no interest in names and roles. The pecking order is inviolable.
- Some tasks or procedures can be summarized into a checklist of no more than 5-7 evidence-based items, no different than a pre-flight checklist. The list can be developed locally to encourage ownership.
- Even though Peter’s work has saved thousands of lives and hundreds of millions of dollars, most of that came from just one checklist (central line placement) out of thousands upon thousands of medical procedures and tasks. That’s either a wide-open field or a depressing commentary on modern medicine, depending on your perspective.
- Non-clinicians, like administrators and probably IT executives, aren’t usually comfortable getting out on the floors but can play a big role on offering a fresh perspective for problem-solving and in understanding how projects are financed, staffed, and run.
- Doctors practice as they were originally taught in school using the “see one, do one, teach one” model that tells them to ignore everybody else’s opinion and go with their own. Good teamwork means a nurse doing what the doctor says. Doctors are not taught to communicate or to manage stress. They do not have time to keep up with the literature. There is no standardization, even within one organization. Residents make mistakes because they don’t want to look stupid by asking questions.
- Checklists worked in aviation because the industry admitted that pilots make mistakes and took the attitude that every crash is preventable. That hasn’t happened in medicine, where hospitals and doctors refuse to admit that they are not infallible. Even Hopkins (arguably the best hospital in the country) defended its catheter infection rates (among the worst in the country), using the “our patients are sicker” argument. After using Peter’s methods, their infection rate dropped from 19% to near zero, saving an estimated eight lives and $2 million.
- Quality requires central analysis of data. You don’t know what’s working without data. No other industry would tolerate healthcare’s sloppy data practices.
- Making the list is easy. The hardest and most important parts, which hospitals always want to skip, are evaluating the culture, making sure every patient is treated using the list, and measuring the results.
- State-wide projects don’t always work. They took shortcuts, made data reporting voluntary, and let turf wars (infection control docs vs. intensivists) compromise the plan. But in Michigan, their infection rate dropped from 2.7% to zero when they swallowed their pride and followed the plan.
- Medical research gets all the funding, while patient safety research hasn’t. Part of healthcare reform is creation of the Office for Patient Safety Research.
- The only profit to be made in patient safety is for insurance companies.
I extrapolated his thoughts into IT:
- Peter said in my interview that errors will go up when CPOE is introduced because it’s a change, nothing is standardized, and CPOE is set up to look like the paper it’s replacing.
- Decision support is the real value of CPOE, but it’s not usually added until afterward.
- Every hospital has to develop its own clinical decision support rules, which is like each airport having to build its own air traffic control system.
- IT systems can support enforcing the lists and reminding providers about them.
- Use shared decision support rules to begin standardization and using best practices.
- Look at data collection, reporting, and transparency. Peter found that virtually no hospitals have the right information in their databases to be able to know their infection rates.
- Use these methods for IT project rollouts and maintenance to reduce mistakes and to remove vendor and IT pressure to do something harmful.
- Find ways to get research into practice. Why is research a science, but the practice of medicine is an art?
- For vendors, build support for lists and reminders into applications, where they can be cued by workflow.
It’s a bit disconcerting to see just how inconsistent healthcare delivery is. It’s based on science, but often is a long way from being delivered in a scientific way. The major point of the book is that nobody’s head is big enough to hold all the information about medicine and research findings, so practitioners often are endangering patients by what they don’t know or don’t practice.
Few would doubt that the book outlines incredible opportunity for improvement in every kind of patient care setting. We’re talking saved lives, not just saved dollars. The good news is that’s exactly what computers are good at. Giving providers access to lists, providing immediately usable reference material (how-to videos, audio instructions, etc.), linking to the evidence, and offering collaboration platforms could all be key elements in implementing the quality measures called for in the book.
This is an excellent book, although it will make providers question their core beliefs about the healthcare system they work in. It’s pretty screwed up, as we know, and getting worse. The goal isn’t perfection, it’s improvement, and that won’t be easy (if it were, everybody would already be doing it). Are there enough providers who can look beyond the knee-jerk reaction of just making a Pronovost list and claiming mission accomplished to actually improve healthcare quality? Maybe or maybe not, but if enough at least try to tackle their problems in a rigorous way, they’ll probably avoid killing a few patients.








Mr H, you failed to link to the Bloomberg Businessweek story on Expert Consensus so here’s the link http://www.businessweek.com/magazine/content/10_38/b4195022450592.htm
However, your failure doesn’t irk me quite so much as that of the cub reporter who called me asking for an opinion about them, used all of my suggestions about who to follow up with (none of whom she’s heard of) including Best Doctors, Cleveland Clinic Online, & Bob Wachter, and then of course didn’t mention me or quote my bon mots in the story…
To be fair, I’d never heard of the company even if I do know the management from past lives, but she honestly though $20K was a reasonable deal!
We all focus on accuracy of data in Health IT and work hard at it so I just thought the same should go for those who rate doctors and hospitals, which a bone of contention with most MDs and hospitals for good reason. Health Grades and others could use some updates on their files too in not leaving “dead doctors” out there for referrals and ratings:) I ran across this by accident but made for a good post I think, especially in view of the fact that HealthGrades put out an article on the 10 most deadly hospitals in the US not too long ago, which to me is not really good PR.
With healthcare, we all need accuracy and these folks should fall into that category too. As well as the City of Buffalo, these folks could use a copy of the Social Security Data base Death Index too.
I used my deceased former obgyn here who died of cancer 6-7 years ago and she’s still listed! By the way this might be something to look at if you are an MD to see what they have listed too.
I think we would do better to focus on the living rather than the dead with information and not mess up like the City of Buffalo did with paying premiums for 2 or more years on dead employees too- everyone needs to get their data updated for accuracy. You just can’t believe everything you see today on the internet.
http://ducknetweb.blogspot.com/2010/09/healthgrades-and-other-md-rating-and.html
In regards to your comment about vendor help desks-
I am a support analyst for a “major EMR vendor” and I shuddered when I read that as I’m sure every other support analyst did. We try to juggle up to three times the number of tickets we can handle efficiently and are constantly surprised that we hear so few complaints from our clients. My job has transformed from a fun problem-solving role to a chore related to having to constantly dance around why our development team can’t get anything done. Clients need to speak up and demand that SLA’s be built into contracts and hold vendor’s accountable. The support team is as unhappy as you clients.
[From Mr. HIStalk] I understand — I worked as a vendor senior support analyst for several years. I made a lot of excuses, pretended we didn’t know about major problems that were endangering patients at pretty much every client site, and tolerated clueless management who brought no relevant knowledge experience to their job except to demand that we close more cases, even when that was not in the best interest of our customers. As we always said back then, don’t blame the firefighters (support staff) when the arsonists (developers) set more fires than we can put out efficiently and politicians (management) who refuse to fund more firefighters.
About Checklists in medicine- every Kaiser doctor in Northern CA was just given this book: The Checklist Manifesto: How to Get Things Right by Atul Gawande (Hardcover – Dec 22, 2009) which seems to have been published before the author you reviewed…I am wondering who(m) we should be crediting with the discovery of medical checklist?
[From Mr. HIStalk] Unless Gawande’s book is different than his article in The New Yorker from which it sprang, he just added some prose and stories around Pronovost’s work, which he fully references and credits in the article. I don’t think there’s any question that Pronovost discovered the checklist and is doing a lot more with it than just publishing books, but it’s unfortunate that Gawande’s best-selling experience confuses people into thinking that he’s more than an observer of what others are doing.
“…extolling the virtues of Twitter, which they summarize in a grammatically incorrect manner as, “… us enlightened folk know that the conversations on Twitter are insightful and illuminating.”
Twitter: when you absolutely, positively, have to say nothing as fast as possible.
Thanks for the book review; as you said, it mirrors a lot of what we “already know,” but obviously does so in a convincing, informative way. I find the metaphors to the aviation industry helpful in understanding the problem (ie, comparing CDS to air traffic control), but I wonder sometimes if part of the problem is where that analogy falls apart: namely, the pilot normally has to only deal with the plane and the forces of nature, not the passengers themselves. Their “care” is handeled by others.
Obviously, no metaphor is perfect, and as I said, I think the flight one is good for many things, but the “our patients are sicker” response does have at least some grounds for consideration (even if it’s not a good excuse). Just as it’s harder in education when the majority of one’s students are already behind in a certain skill set, so working with a sicker patient base will necessarily affect how much they improve. Again, it’s not the only factor, and it doesn’t let physicians or hospitals off the hook, but it does have to be part of the equation, as much as the weight of passengers has to be factored in when putting people on a flight.
Michelle makes a good point, checklists and airplane metaphors can only go so far.
Although I strongly believe in the value of checklists, lets keep in mind that the jet plane came with million+ page spec books, operations and maintenance manuals. These are must haves in creating correct check lists.
In my case (and I am sure for many of your readers) I seemed to have misplaced the spec sheets, ops and maintenance manuals that I was born with. Mother says see remembers seeing them once in the hospital nursery but forgot to bring them home with her as was so excited to have such a beautiful baby. All of which now means that my care givers need to ‘create’ lists each time I visit with a new problem.
The solution for medicine is to create check lists after the fact based on evidence based medicine (EBM), kind of like reverse engineering that jet plane, while it’s in flight…
Mr. Histalk,
Your epiphany is notable: “Do some of the issues vendors ignore in this way endanger patients? No question. I bet if they were forced to go public with their open issues list they’d be a lot more responsive.”
While the issues are under wraps, patients are suffering adverse events, and doctors are devoting patient care time to work arounds.
Thanks for this Pronovost excerpt:
“Healthcare is still very much like the Wild West or like Chuck Yeager in The Right Stuff, where we have this cowboy mentality and we’re just beginning to accept that standardization is a key principal to making care safe.”
Incidentally, the same description could be said about HIT: the Wild West; without standardization, accountability, regulation, usability, and sans efficacy. The government has issued a blank check.
Standardization and regulation is the key to making HIT devices safe.
“Here’s another example that healthcare is different when you have money: a new startup called ExpertConsensus will take your tough medical problem to a group of big-name doctors who will teleconference and make their collective recommendations.”
Can you say “RevolutionHealth”?
Thanks for the book review, Tim. I’m a huge Pronovost fan and have been meaning to read it for months – just ordered from Amazon! I’ll note that checklists were also likely adopted in aviation because, unlike in healthcare, the pilot has the same fate as the passenger, so there’s a HUGE incentive to drive safety. Now the investor chair has been trying to think of a way to make money off checklists for years, but is still struggling. Maybe something like T-Systems?
best,
Ben
Relevant statement: “The major point of the book is that nobody’s head is big enough to hold all the information about medicine and research findings, so practitioners often are endangering patients by what they don’t know or don’t practice.”
Part of competency practiced by effective clinicians is knowing what they do not know. The IT systems are usurping head space of these clinicians with lines of clinically useless jabberwock.
When systems become devoted to patient care rather than billing and cya activities of hospitals, doctors might consider these devices to be useful.