Trey Lauderdale is chief innovation officer of Voalté.

Tell me about Voalté.
We are a startup located in Sarasota, Florida. We develop communication software and solutions for point-of-care physicians. Our whole goal is to integrate voice over IP, alarms and notifications, and internal text messaging, all on the next generations of smart phones like the iPhone and other devices.
My background is with Emergin in the alarm management world. I worked there for a few years, primarily in sales. At Emergin, you view the world as input systems, or systems that send you alarms and notifications to your middleware server. Then, output systems, or systems that we can dispatch those alarms and notifications.
Just stepping back and being new to healthcare at the time, I looked at it and did an analysis of the market. What I realized was the input systems were really going through this growth period of somewhat revolutionary change where systems were becoming more and more advanced. If you looked at the infusion pumps from 5-10 years ago compared to infusion pumps that were being sold at that time, you have these smart pumps coming out that were producing more information. Physiological monitoring systems, nurse call — they were all becoming more advanced.
We received all that information, and there was more and more information we were receiving, but then I’d look at the output systems and the phones that the nurses, the docs, and everyone else were carrying. A lot of times, we’d go in and we’d be integrating this unbelievably complex physiological monitoring system to a pager and it was just a line of text coming across, no variable ringtone, or, these legacy kind of either DECT phones or voice over IP phones.
The nurses and the docs would keep complaining and saying, at that time, “It’s 2008, why do we have to carry this bulky phone, these antiquated pagers?” They would bring in their own personal PDA because they wanted to run all these different applications that were coming out on their BlackBerry or iPhone or other device.
In March of 2008, Apple released the iPhone software developer kit. It just so happened that same day I was at a meeting at Miami Children’s Hospital where the nurses asked me to come in. They were looking for a voice over IP system to purchase for their hospital. I did a quick presentation — these are all the devices Emergin can send to. There was just a look of disappointment on the clinicians’ faces and they weren’t happy with their selection.
That night, I went home and read about the iPhone SDK and a light bulb went off. Why can’t clinicians have one device, one of these smart phones, to handle all of their communication needs, built specifically for their workload model?
A few months later, I ended up leaving Emergin and creating and starting Voalté, August of 2008. At the time, it was me. I found a software developer and we started the company. We took the leap of faith and I quickly realized how unbelievably difficult it is to start a company. Of course, my luck — August 2008 was right when the economy completely tanked out.
I was talking to hospitals. I was talking to angel investors, venture capitalists, and everyone said, “We love your passion. We love the idea you have.” At the time, I was 26 years old. “We’re not going to trust you to start a company. You will not be successful. You’re not going to get this to work.” After about three months of trying to get things going, I was at a point where I didn’t think it was going to work. I was going to have to get a job. I had burned through all my savings. I was living off credit card debt.
Through a mutual contact at the Center for Entrepreneurship at University of Florida, I was put in contact with Rob Campbell. Rob is an interesting individual. He can best be described as a serial entrepreneur. Back in the day, he actually worked for Steve Jobs at Apple back in the late ‘70s. He was part of the marketing group and he helped build the entire market for Apple’s software division. He then left Apple and created a company that founded a couple of products — one is PowerPoint. He started up a lot of companies that have been very successful.
I pitched the idea of Voalté to him. I didn’t know why at the time, but he agreed to come on board as our CEO and help guide us through this progression of the building of the company. He came on board in November of 2008. By December, we were able to raise our first round of financing. We were able to open up our office in Sarasota, Florida. It was really the start of Voalté and the creation of the company.
At that point, Rob was new to healthcare. I had two years of experience, so I was relatively new as well. We went around and — included in this was you — we pulled a number of what we considered ‘industry influencers’, or people who had a good pulse on what was going on in healthcare. We talked to a lot of CIOs that I knew from my previous relationships at Emergin and we asked, “We’re a small startup organization. We’re building our company. Can you point us to someone that we should model our company after? Our services, our support, our software? Who’s the Southwest Airlines of healthcare? Who’s the Starbucks or the Disney of healthcare?”
Surprising to us, we asked about twelve CIOs this and only one of them was able to give us an answer. A lot of them would say, “Well, it used to be XYZ Company until they were acquired by someone.” Or, “It used to be this company, but not any more.” The one CIO that did tell us a company, they told us Epic. It just so happened they just purchased $150 million worth of Epic, so I’d assume that they’re going to say it’s Epic no matter what.
I didn’t realize at that time, what Rob was really doing was analyzing the market. From at least the customers we talked to, no one was taking that vision of the Disney of healthcare IT. So, we started building the organization. One of the first things we knew was we wanted to provide a compelling customer experience, end user experience, to our clinicians and to the people that we provided our software to. We engaged, and lucky enough, Sarasota Memorial right here in our back yard, we were able to meet with Denis Baker. We talked to him about our solution and what we planned on building and he agreed to enable us to work with Sarasota Memorial as our first ‘Development Partner Program’.
I know the term gets tossed around a lot, but what we really proposed to Denis and Sarasota Memorial was, as an organization, we need a hospital to work with to get feedback. Not only from an IT perspective on how we design our solution, but from a clinical perspective of what the nurses need and want for a communication solution at the point of care. From the very beginning when we were designing the user interface, the way the solution was going to work, we pulled in feedback from the nurses at Sarasota Memorial. We brought in nurses for a nurse focus group. We had a big whiteboard up on the wall and we drew out exactly how the application was going to look and we mocked up drawings. The nurses told us word for word, “This is how we want Voalté to work for the voice communication, the alarms, and the internal text messaging.”
But, we also knew that a lot of times your end users don’t really know what they don’t know. We put a button inside our application called Voalté Feedback, which would let any one of the nurses, the clinicians, the end users to hit that button and send a message to us. Things like, the buttons are too close or, this feature isn’t working, or that function is bulky. Before we know it, we went live with the pilot in June, and within a month we received over 90 feedback messages. These clinicians were telling us non-stop all of these problems with our solution from a text messaging perspective, the way things looked. We took all that feedback and we completely refactored our iPhone workflow.
A great example that was told to us was, a lot of the nurses came back and said, “We love the text messaging functionality. It’s fantastic, but I can’t read the text. The font size is way too small. You have to make it bigger.” No problem — we made the font size really big. Then we got a message back the next day, “The font size is way too big. I want to see everything on the screen.” I went to the engineers and said, “Guys, we’re stuck. We’re caught in a Catch-22. There’s no way.” They said, “Well actually, we can. It’s an iPhone.”
What we created was a variable font size so nurses, on the fly, can change their font. Also, we save that to their user profile so when they pick up an iPhone, they log in to start a shift, and we load up that component of their profile. It really, at that moment, struck us that we can’t just build a vanilla-flavored application and push it on everyone. We need to take this feedback and customize it for each one of the individual end users. From Day One at Sarasota Memorial, we took that feedback to build our application.
Since then, we’ve expanded the pilot at Sarasota Memorial. We’re out to an additional four units there. We have an enterprise agreement, and we’re going to be rolling out across the whole hospital. We signed a second hospital out in California, which was Huntington Memorial. They went live in December with a similar solution to what Sarasota had. We signed our third hospital that we’ve installed and we’re not allowed to announce yet, but it will be coming out in the next few months. We’ve recently signed hospital number four; and I’m currently waiting for a phone call which will hopefully be hospital number five, which should come in this afternoon.
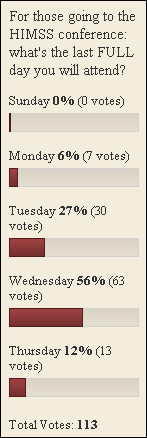
From our perspective, it’s a really exciting time to be in this industry. We think we have a lot of momentum heading into HIMSS, and we’re real excited.
I did a survey when the iPhone first came out. Most readers didn’t think it would really have any healthcare impact. What did they miss?
I would really think that again, just looking at your reader base — which obviously, I have a tremendous amount of respect for — I think that they were all looking at a fad from a technical perspective; the technical components of the iPhone and if it will work, or won’t work in healthcare.
Apple has a way of making products that are unbelievably easy to use. I think that’s really what the game changer was. They reinvented the way you interact with a phone, from the swiping, the pinching, the zooming, and Apple just does a fantastic job of paying attention to very specific details. If you look at everything they build, down to your little icons on your MacBook — how they bounce up and down, the little blue dot appears. It’s just an unbelievable amount of attention to user detail and what users are going to look for, in regards to interaction with the device.
I think the compelling thing that was overlooked was just the user interface and the user experience that Apple is able to provide. I think that was probably the missing component, if I had to guess.
Do you think working on the Apple platform with Apple developers forces you to think more about usability than the average software developer working on a client server-type application?
Off the bat, in the Apple SDK, there’s actually whole sections dedicated to keeping and conforming to the Apple user interface. They provide a lot of guidance and feedback on how to make all the applications look and feel somewhat the same. When you’re applying to the apps store, they actually go and review… I don’t believe they’ll reject you for moving away from your standards, but they try to greatly encourage you to move down that path, so all the applications somewhat look and feel the same.
If you look at our application, it looks great. When we go into some of the hospitals and we install or we go live and we’re there training; if a nurse has an iPhone on their own, they really don’t need Voalté training. Our phone application looks just like the iPhone application, our text messaging looks exactly like the Apple text messaging, the SMS application. We actually had to stop users from being able to access our application during training or else the first class we let them go into it, they went wild using it. It’s just so intuitive.
I think it does, to a degree, force developers to kind of rethink what they can do. You always hear people complain about multitasking, and you can’t run background applications on the iPhone. Having one application open and some of the limitations that Apple puts on you are actually mixed blessings; it makes you think, “Well how do I use all the real estate on the screen, and how do I make sure my current application that’s running is making the most of what tools I have available?”
On the flip side, the iPhone developers probably don’t have much healthcare experience. Is that a problem?
I don’t think it’s a problem, because what we see happening right now is a number of large companies that have a great deal of healthcare experience are just going out and picking up either iPhone developers, or iPhone consulting groups to develop their applications for them.
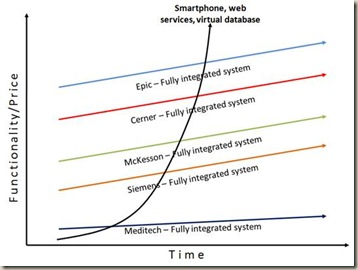
Epic has released Haiku as their EMR application. Allscripts, they released an application last year. I’m sure Cerner and the rest are following suit. I doubt that they had their own internal developers build that. They probably went out and hired iPhone developers and provided the healthcare expertise. I do think that there are not a lot of startups in this space that have created iPhone applications. Specifically, iPhone healthcare-focused companies like we’ve done, but I see that changing in the next few years.
Overall, I think right now Apple claims 700-800 medical-focused applications. I think the platform in healthcare has an unbelievable amount of momentum, and with the iPad coming out, that’s going to continue to grow. Both the iPad and the iPhone run on the same development environment, so even though right now there might be a shortage of iPhone healthcare-specific developers, I think that number is going to continue to grow exponentially. You don’t need to be a healthcare expert to develop on the iPhone. You need to be an iPhone developer, and there are plenty of those out there in the field right now that can get picked up by healthcare companies to help develop the application.
How do you help solve the problem of both device and information proliferation for doctors and nurses?
I think the first component is really understanding the workflow of where that information’s being generated from and the different criticality of the information. If you look at where these pagers and devices were receiving the alarms and notifications from, you had a wide degree of things being blasted to caregivers. An example might be they’ll carry one pager, which is their code blue pager or their rapid response team pager. Then the next device will be a pager that goes off for TeleTracking if they have a patient coming into the floor.
I think the key is understanding all of the information that’s getting blasted to the nurse, and from what different systems it’s getting blasted. Then, creating a workflow model of “these are all the alarms, notifications, phone calls, text messages, that are being received,” and then building and orchestrating a plan around the three components of communication — which are really voice, alarm, and text messaging.
There are things like; we can associate specific ringtones for different types of alarms. For example, at Sarasota Memorial Hospital, some of the devices they were carrying would go off for a nurse call — a call bell alarm — then another device would go off for a bed call. They had Stryker Smart Beds.
What we actually did was on the iPhone, we have different ringtones for the different types of alarms. For example, if someone hits a nurse call alarm and it goes off on the nurse’s iPhone, we play the exact same ringtone in .wav file that will be played at the central station. A very subtle beep, beep, beep, and they know OK, that’s a call bell alarm. We blast it across the whole unit, and we play the Stryker Smart Bed .wav file of what the noise is supposed to be when there’s a bed call. We have unlimited customization and configurability to make sure that ringtones are played for the right different types of information.
Again, you want to be careful with that because you don’t want this device with 20 ringtones. It’s that careful balance of getting the right amount of ringtones and different types of notifications, but not overburdening the nurse with all this different information they have to memorize.
Do customers perform ROI justification to buy your product?
I think there’s a couple components that they can look at for ROI. Off the bat, we can replace a number of devices. The first would be what we considered a legacy voice over IP phone. We could take that price, and there’s usually the hardware costs associated with that; the charger cost, the external battery cost, and typically, there’s a software license cost associated with that device.
Next are all of the different pagers that are going off. Just off the bat, it’s consolidation of devices. You take a PDA, the pagers, the voice over IP phone; combine them together into one device.
But beyond that, when you look, there’s a number of studies that have been done; specifically by University of Maryland. It showed that overall, the average 500-bed hospital will waste approximately $4 million a year in wasted communication, which is the telephone tag back and forth between caregivers and people not having the right information to act, or the hunting and gathering of different caregivers.
The second area where we would see a return on investment is a better utilization of the nurse and clinician time. Nurses could access the right information at the right time through our solution so they could therefore, be more effective at their job.
The third area that hospitals are interested and where there’s more of a long-term ROI, is improvements in Press Ganey and HCAP scores. Through our solution, any pilot that we roll out in, or any hospital that we install in, we go and we do an analysis of the hospitals; specifically, in Press Ganey and HCAP. We look at noise in and around the room, and response time to call bell.
We look at those metrics before Voalté goes live. Then after Voalté goes live, we do an analysis to see if we were able to produce an improvement in those scores. In the long term, that should overall, greatly affect the hospital’s ranking from a patient satisfaction and a patient safety score, which would make them a more prestigious hospital and hopefully, bring more patients in to the facility.
I would think caregivers think it’s pretty cool that they get to turn in their analog pager and be given an iPhone in return.
Definitely. There is an angle of nurse retention. You go into a hospital and you tell the nurse that they’re going to get iPhones. I’d say 90% of the nurses are thrilled, they’re excited. They can’t wait to see it, but you get the flip side of that as well. About 10% of the nurses will actually step back and say, “No way.”
I’ll never forget this. It was one of the most memorable points at Sarasota Memorial, our first installation. We went in for training and I was part of the training team. I love going in and talking with the nurses and getting that end user feedback interaction. We were doing training and there was one nurse who was kind of in the corner while we were doing training. I went and said, “Are you excited? What do you think?” She looked at me and said, “I don’t even use e-mail. There is no way I am using this iPhone.” She puts the device down and said, “I’m not going to use it.” I tried to convince her and she just said… I think she was a few years from retiring and had no interest at all in learning this new technology.
Later that night, I was there during go live. I looked and I saw her and she looked frustrated. She was picking up the phone and she kept dialing a number and she’d slam the phone. I went over and I asked her, “Is everything OK? Is there anything I can help you with?” She said, “Well, I’ve been trying to reach the floor pharmacist all night and I can’t reach him.”
For their workflow model, they have a floor pharmacist who covers a whole tower. At night, you have to send a page to him and you don’t really know if the page got out or if he’s going to be able to respond. I said, “For this pilot, we actually provided the floor pharmacist with a Voalté iPhone. Why don’t you try sending him a text message?” She looked over at me, kind of with a sly face and she grabbed the device. I walked her through, she hit the Quick Message button, and she sent it out in a couple of taps. About two minutes later, she got a response and it was the floor pharmacist saying, “I’ll be there in five minutes and I’ll drop off the meds.”
Typically, it takes her a few hours to find that caregiver. She looked at me and said, “Well, I guess it’s not that bad.” So, I don’t consider it a complete victory, but it’s finding the specific users and spending the time to educate them on different examples of how to use the technology. Even though she didn’t fully embrace the solution afterwards, I think that we were slowly starting to win her over. I think that’s one of the areas, as a company, which we’re really attempting to differentiate ourselves in the whole customer experience and our end user experience.
Remember at the beginning of our conversation I talked about Voalté feedback? Originally, when we built that, our whole focus was we need to get the best features, the best ideas, from our end users. We want to have unfiltered feedback, from a feature standpoint, from our end users. Then what we realized during the pilots was the nurses started sending us messages back from a support standpoint. They’d send us a message like, “I forgot how to turn myself into busy mode,” or, “How do I add a custom quick message?”
It dawned on us that this is the absolute perfect tool for end user support. The way it works is the nurse, again, they could hit that button Voalté Feedback. They send a message. We actually have our own Voalté server in the cloud that receives that message, dispatches it to my personal iPhone or our support team’s business iPhone. We receive that message and we can login to the Voalté server remote and establish bidirectional support communication with that individual caregiver. So off the bat, any user of our software, at any moment, 24/7, could have instant communication, from a support standpoint, with one of the Voalté support employees.
Also, from a technology standpoint, you’re trying to drive innovation, new features. We have unfiltered feedback from every single one of our users, which is huge. It’s kind of the same concept of Twitter. Our Southwest Airlines, Starbucks — they all have a Twitter account and if you complain at (@) them on the Twitter account, they’ll respond by responding at (@) you. We’ve got that same philosophy, that same methodology; but we’re applying it inside healthcare to receive feedback, but also support the nurses in the field.
Beyond that, what we’ve also done, from a remote monitoring standpoint is we’re actually able to track not only that the message was sent on the device, but any trouble that happens down to the device level — remote monitoring of servers. That happens all the time, where people can monitor a server. If something goes wrong, you receive an alarm or notification. We, obviously, do that. We keep a VPN connection to every Voalté install server. If any one of the adapters, any one of the components fails, we get notified.
But, we can actually take that down a further level to the iPhones. We’ve customized and designed our solution so we could actually look and see if there are trouble tickets or trouble logs in the iPhone. All the nurse has to do is plug it into the charging station. We can connect to that device and we can reset the firmware. From a remote monitoring standpoint, what’s happened is the platform of having these smart phones at the point-of-care has enabled us to do things like have unlimited feedback from our nurses, from our end users. Have really, unlimited remote monitoring down to the device.
When we first started the company, it was all about the platform enabling the perfect trifecta of communication, which is voice, alarm, and text messaging. But as we’ve been out in the field and learning from our customers, we’ve realized it’s not just about the technology. It’s also about the customer experience, the end user experience, and we finally have the perfect platform to provide that level of end user experience that the nurses really need, such as the Voalté feedback and the remote monitoring down to the actual device.
We’re pretty excited. I guess you could consider us one of those overly aggressive startups that, you don’t start up a company just because you want to drive a little bit of change. You start a company because you want to make a dramatic difference with your customers, with your end users. We not only want to have awesome technology that’s built specifically by our end users, we want to provide and overall amazing end user experience to our customers.
Definitely, I probably sound like a naïve, startup, 27-year-old guy, but I think that passion is really well conveyed in the way that we speak about our company, we speak about our products, and we talk about our customers. If you talk to any one of the Voalté hospitals we’ve installed at, from the end user, the nurses, to the CIO, they’ll tell you that engaging with us, as a company, is a lot different than any other organization.
I think the reason we’re able to do that has really been subject to the influence Rob Campbell, and also, our Chief Experience Officer, Oscar Callejas, bring to the table. Where you have Rob, who’s more of a Silicon Valley startup guru; but Oscar, when we brought him on, his background is in hospitality. He’s worked in hotels for the last 15 years managing these high-end hotels and organizations. When he came in, he brought that whole view of “it’s about the customer experience.”
When I started the company, that really wasn’t on my mind. I was all about the technology, integrating the iPhone; but they brought that flavor to the organization and I think it’s all coming together really well. I’m really happy with where we’re at as a company.
Last question, and this is the one you knew was coming. Pink pants at HIMSS?
Oh, absolutely. Not only pink pants at HIMSS, we wear pink pants at every single installation. It’s part of the customer experience. We come in and we are the pink pants company. It’s part of that whole thing I was just talking about, where we don’t want to look like other healthcare IT companies, we don’t want to talk and act and feel like them. We want the whole experience that customers and nurses and hospitals go through to be different.
When we walk in for the first day of Voalté training, its Voalté day. We come in and we take pictures of the nurses to put in the application, we’re wearing pink pants. During clinical training, we’re in pink pants. Go live support, wearing pink pants. You know, people laugh at it, but the nurses know who we are. They see the Voalté person walking by; they know exactly who that person is for help and support.
At the HIMSS conference, last year we were all kind of sitting around. Little startup, Voalté. We were looking at all the booths and we saw GE with an 800×800 foot booth and dancers and DJs and everything else. We looked at each other and said, “God, how on earth are we going to get any attention at this conference? No one’s going to look at us. No one’s going to even acknowledge that we’re there.” Someone said, “Well, why don’t you wear pink pants?” Everyone kind of laughed, but we looked around and said, “Why don’t we wear pink pants? What do we have to lose?”
We actually e-mailed Inga because I was kind of worried. I was the only one who had actually ever been to HIMSS before, so I know it’s a suit and tie event. I was thinking, “Are we not going to be taken seriously?” Then, Inga threw it up on your blog so we really had no choice, so we did it. Believe it or not, it’s kind of become a rallying cry for the company. The pink pants, in a way, symbolize what we’re about. We’re different. The experience is different and it’s a lot of fun. You’d better believe the pink pants will be there.

















































Thank you for your comments on Amazon. Agree 100%