Top News

Microsoft and GE Healthcare complete the formation of Caradigm, their 50-50 joint venture that will be led be CEO Michael Simpson from GE Healthcare. Lauren Salata (Care Innovations) joins as CFO an Michael Willingham (Philips Healthcare) assumes the role of quality assurance and regulatory affairs executive.
Reader Comments
From LesserEvils: “Re: what uninsured un/under-employed do. They have several choices. They can wait until they are really sick and visit an ED, which just makes the cost of care even higher. Or they can become self pay, which in many cases translates to no pay, which we all end up paying for in some way. Or, they file for bankruptcy. Something like 60% of personal bankruptcies are due to the un/underinsured being unable to pay medical expenses.”
From Paul: “Re: Cerner. Featured in Investor’s Business Daily. Feels like an optimistic PR announcement, but I see solid stability with their hosted offering and decent improvements on the ambulatory side.” IBD quotes analysts who like the fact that Cerner shares have done well lately, bucking past experience in which any one HIT vendor that reported bad results (like Allscripts) dragged the whole sector down. They also like Cerner’s chances to offset eventually declining EHR sales with revenue from medication dispensing cabinets, medical devices, and outsourcing services. It says that although Epic wins most of the high-profile hospital deals, Cerner’s win rate has improved in the last couple of years.
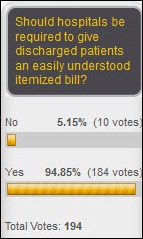
From AcuVedder: “Re: patient right to access and correct their health information. The Office for Civil Rights posts a video explaining patient rights.” I don’t know if it will help or hurt hospital foot-dragging (long delays and high per-page costs involved with giving patients copies of their own records), but at least the video sends a signal that the government sides with patients, in theory anyway. If it’s so time-consuming and expensive to give patients a copy of their records, imagine the disarray that must be involved with providers trying to access and use those same records for treating those patients during their stay. Or at least that’s how I would see it as a patient. Imagine a garage that isn’t able to provide estimates, sells services ordered by third-party mechanics over which it has limited control, and expects customers to just pay their bills afterward with no explanation of what was done or how their car should be driven or serviced in the future.

From Izzie: “Re: Accretive Health. Are hospitals more or less likely to hire them as their RCM vendor since their dispute with the Minnesota attorney general?” I would expect that’s the case since nobody wants bad press, but let’s ask their customers and prospects: have the headlines changed your plans involving Accretive? How? Tell me. I’ll keep you anonymous.
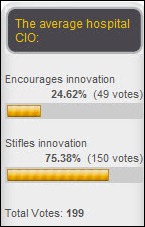
From Nurse Informaticist: “Re: help! I work for one of the big vendors that thinks a nurse is a nurse. They have no idea what my specialty certification in informatics is or what it means. How about a shout-out for the fact that nurses specialize and have expert knowledge to contribute to system design? Long time, die hard fan!” I’m not an expert on ANCC certification, but I recall that it requires passing a test and clocking a bunch of hours working in any kind of informatics role. Vendors may see that as more of an indication of interest rather than of specific, value-added skills since anybody can call themselves an informatics nurse and lots of nurses make their living doing informatics-like work (training, consulting, support, etc.) with no higher education or certification at all, just applied informatics experience (which is often true of other professionals as well.) Then there’s the Epic model, where they’d rather have impressionable, cooperative (read: young) licensed people who have recent frontline care delivery experience and no IT connection. Finally, some vendors have a warped view of the provider food chain in thinking that physicians can intelligently speak for nurses, therapists, pharmacists, etc. and don’t seek other clinical expertise. I’ll poll HIStalk’s readers again: are nurses with informatics education and/or certification adequately involved in system design and implementation by your organization? Why or why not?

From Not Very Innovative: “Re: CMS’s $10 billion Center for Medicare and Medicaid Innovation program. In a WSJ editorial, Steven Greer MD says Congress should dismantle it since it’s a poorly conceived, politically motivated system that is unlikely to deliver innovation or ROI.” He should know – he was chairman of its grant review program, concluding from his experience that it is “nothing but a pork program that diverts untouchable Medicare entitlement funds to political cronies in key states.” The first millions went to a Chicago group run by the President’s golfing buddy and a program that eventually subcontracted the work out to IHI, formerly run by Don Berwick, who was running CMS at the time. He concludes, “The newly created CMMI is nothing but a stealth stimulus plan to help job creation and politicians’ careers, just like the extremely ineffective ARRA ‘stimulus plan’ was in 2009. The ARRA did nothing to reduce unemployment, and neither will the much smaller CMMI.” It probably doesn’t help Dr. Greer’s credibility that he is a UFO contactee who has accused the government of an alien cover-up, not that there’s anything wrong with that.
HIStalk Announcements and Requests
 Life got in the way of mentioning HIStalk Practice highlights last week, so here are a few don’t-miss items from the last two weeks: Dr. Gregg discusses intriguing new bedside monitoring technology from Blnk Medical Technologies. David Wellons muses on the next generation of healthcare informatics. Over the last decade, more widespread use of EHRs has contributed to a 17% increase in the use of the two highest-level codes for established office visits. Consumer Reports adds ratings for Massachusetts primary care providers. eClinicalWorks treats employees to ice cream in exchange for donations to the troops. I have resigned myself to the fact that I will never catch Mr. H in terms of the number of LinkedIn connections, Facebook friends, or Twitter followers. The only thing that keeps me from falling into a deep depression is seeing lots of visits to HIStalk Practice and new sign ups for the e-mail updates. Thanks for your support, which is far more effective than therapy.
Life got in the way of mentioning HIStalk Practice highlights last week, so here are a few don’t-miss items from the last two weeks: Dr. Gregg discusses intriguing new bedside monitoring technology from Blnk Medical Technologies. David Wellons muses on the next generation of healthcare informatics. Over the last decade, more widespread use of EHRs has contributed to a 17% increase in the use of the two highest-level codes for established office visits. Consumer Reports adds ratings for Massachusetts primary care providers. eClinicalWorks treats employees to ice cream in exchange for donations to the troops. I have resigned myself to the fact that I will never catch Mr. H in terms of the number of LinkedIn connections, Facebook friends, or Twitter followers. The only thing that keeps me from falling into a deep depression is seeing lots of visits to HIStalk Practice and new sign ups for the e-mail updates. Thanks for your support, which is far more effective than therapy.
Acquisitions, Funding, Business, and Stock

Streamline Health reports Q1 results: revenue up 31%. EPS $0.05 vs. –$0.03.
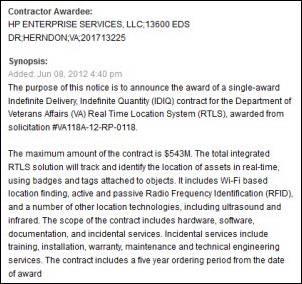
Stanley Healthcare Solutions, a division of Stanley Black & Decker, acquires RTLS provider AeroScout. We reported that rumor on May 18.
Veritas Capital completes its $1.25 billion purchase of the Thomson Reuters Healthcare business, which will be known as Truven Health Analytics. You may recall that Veritas sold government healthcare IT contractor Vangent to General Dynamics for $960 million last August, making a 240% profit on its investment.

Ringadoc receives $750K in an angel-led seed round, with the participation of Practice Fusion CEO Ryan Howard and LA-based technology incubator Curious Minds. The company offers virtual visits from its physicians at a cost of $89.99 per year and $29.99 per call, with three free calls per year. Fast Company just profiled Ringadoc, saying that it’s operating out of Practice Fusion’s San Francisco offices and using its EMR. The company says it has 1,600 registered users and will soon launch a service that will allow physicians to use its technology in their practices.
Allscripts creates an incentive program based on earnings-per-share performance for 10 of its executives, but CEO Glen Tullman was not be included for unstated reasons. The company also amends the employment agreements of Glen Tullman, Lee Shapiro, Diane Adams, and Laurie McGraw to require that they resign within 10 days of a change in company control to earn their cash payment for not being retained.
Discharge planning and readmissions software vendor CareInSync gets $1.6 million in Series A funding from HealthTech Capital. Above is a video of staff from Marin General Hospital talking about their use of the company’s Carebook transitions software.
Athenahealth launches a “More Disruption Please” program that will sponsor hack-a-thons, invest in startups, and open up the athenahealth platform via APIs.
An Israel business publication cites sources claiming that iMDsoft is talking to a private equity fund about an $80 million sale of the company. I didn’t realize that its three founders also founded population management systems vendor CareKey (sold to TriZetto for $60 million in 2005), and two of the three also founded consumer telehealth systems vendor American Well.
People

Consultant Karlene Kerfoot, PhD RN joins API Healthcare as VP of nursing.

Lifespan (RI) names Ian Hyatt (GTECH) VP/CTO.

ZeOmega appoints Christopher Mathews MD (Community Health Network) SVP/CMO and adds Anne Wilkins (Healthways) and Anna Haghgoole (Sandbox Industries) to its board.

Santa Rosa Consulting names Patrik Vagenius (Dell Services) as EVP of sales and marketing.

Larry Stofko, formerly SVP/CIO of St. Joseph Health System (CA), has been promoted to EVP of the system’s Innovation Institute, which will design, develop, and commercialize potential solutions; create and manage a venture fund; and convert delivery opportunities into business units.

CareCloud appoints Joseph P. Sawyer (American Well) as VP of marketing.

MediRevv names Holly Krueger (CureIS Healthcare) as director of sales.
Acuo Technologies hires Barry Gutwillig (Virtual Radiologic) as senior director of business development.
Vocera appoints Steven Soderberg (Force10 Networks) as CIO.
Orange Regional Medical Center (NY) hires Sujatha Ramanathan (Pain Centers of American) as its director of ambulatory EHRs.
Announcements and Implementations
NY eHealth Collaborative announces that three RHIOs and three HIE vendors will participate in the state’s HIE.
RadNet, an operator of 232 outpatient imaging centers, implements eRAD’s RIS, PACS, and report generation solution.

The Advisory Board Company launches its 2012 Patient Engagement Blue Button Challenge to encourage the creation of apps for improving care by sharing health data. The prize is $25,000 and submissions are due August 6.
The EntryPoint module of PatientOrderSets.com earns ONC-ATCB certification.
MyHealthDIRECT wins ONC’s discharge follow-up appointment challenge, earning the company $5,000 and the opportunity to run a pilot project.
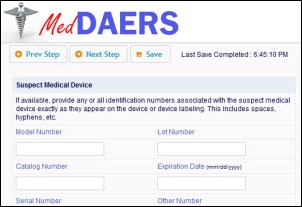
A team from IOSTREAM wins another ONC challenge, this one for creating the MedDAERS portal that providers and consumers could use to report adverse events and other problems with medical devices.

EXTENSION announces the release of Version 3.0 of its clinical alerting system.
Anthem Blue Cross and Blue Shield in Colorado announces that providers can access Availity’s Health Information Network to verify eligibility, submit claims, and review clinical histories and care alerts.
Government and Politics
HHS posts recorded streaming video of the Health Datapalooza plenary sessions. For celebrity watchers, Jon Bon Jovi goes on at the 1:43:00 mark of the Tuesday morning video. He muffs some lines when reading the script, but then ditches it and speaks really well. He mentions his “pay what you can afford” JBJ Soul Kitchen restaurant in Red Bank, NJ and his corralling of Aneesh Chopra outside a White House men’s room to talk about apps that can find available shelter beds and medical providers in real time.
The Congressional Budget Office says that if lawmakers do what they usually do to address budget problems (i.e., make them worse), healthcare entitlement spending will in 25 years make up 10% of GDP, pushing the country’s red ink to 200% of GDP.
The House passes a bill that would repeal PPACA’s medical device tax that is intended to subsidize the cost of providing insurance coverage to 30 million new people. The bill isn’t likely to pass a Senate vote and the President says he will probably veto it anyway. Device manufacturers will pay 2.3% of gross sales starting in January, and several of them have already announced layoff plans to offset the new expense.
The Federal Trade Commission files charges against electronic payments and collections vendor Checknet, whose customers include healthcare providers, for leaking consumer data. Checknet’s COO installed file-sharing software on his computer, exposing the health insurance and medical information of 3,800 patients to anyone using the same peer-to-peer software.
A proposed Michigan law would create a Peace of Mind Registry, an online database where patients can record their advance directives for review by providers.
Other
 If you are a vendor looking for a cool trade show give-away, here is something better than a tee shirt, stress ball, or even a warm chocolate chip cookie. Pong Research announces a $120 iPad case that not only provides protection, but boosts the iPad’s 4G reception up to 10x, the Wi-Fi reception up to 9x, and range by 2x. Plus, it reduces exposure to electromagnetic radiation. The trinket bar has been raised.
If you are a vendor looking for a cool trade show give-away, here is something better than a tee shirt, stress ball, or even a warm chocolate chip cookie. Pong Research announces a $120 iPad case that not only provides protection, but boosts the iPad’s 4G reception up to 10x, the Wi-Fi reception up to 9x, and range by 2x. Plus, it reduces exposure to electromagnetic radiation. The trinket bar has been raised.
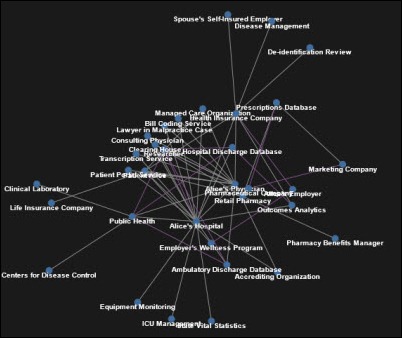
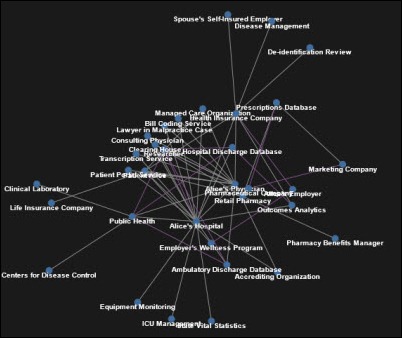
Harvard Professor Latanya Sweeney PhD announces theDataMap, a crowdsourcing project to map the flow of personal data in the US. She says her early attempts to document the ever-increasing flow of patient information into more and more corporate hands elicited gasps every time she showed the graphic.
Two of New York City’s biggest health systems, NYU Langone Medical Center and Continuum Health Partners, announce plans to merge into a super-system that would cover the most affluent Manhattan neighborhoods and flank Mount Sinai Medical Center. The reaction of Princeton health economist Uwe Reinhardt: “Economists have for some time now worried about the ceaseless consolidation on the supply side of the health care market, facing a much more splintered payment side with less market power … So a hospital can literally tell an insurer you either take our prices or you take a walk, and that’s what’s happening. Both sides always justify that, not on the basis of crude market power — we want more market power to get better prices — they always find some kind of high national purpose.”
Rapping 10-year-old twins star in a hand hygiene video for caregivers that was developed by All Children’s Hospital (FL), where one of the twins had been a patient. The video won an award from an infection control group. Now I can’t get “scrub-a-dub-dub” out of my head.
Mostly unrelated except for a medical clinic mention: the best graduation speech in history, even better than the one Steve Jobs gave at Stanford. The message to rich kid high school graduates: you’re not that special – we all are.
HealthLevel Script Object Notation, an open source HIE standard based on JavaScript Object Notation, seeks board members to steer what it says will be the most widely used HIE standard in the world. Nominations are due June 30.
An Oklahoma doctor asks in The Atlantic, Are Computers Getting Between You and Your Doctor? He says doctors are starting at computers instead of listening to and touching patients, are copying/pasting medical information without adding any value, and are forced to ignore the patient and click screen after screen to justify their payment. He concludes, “On my best days in practice, it seems as though all of my patients are savvy, engaged, and connected: e-patients. On the bad days, I feel like an overcompensated data entry clerk.” Check out the hideous stock photo used to illustrate the article (since nobody reads anything unless there are pictures, even unrelated ones): the monitor looks like it was made in around 1997, there’s a keyboard but no mouse, and the office furnishings look a lot more like a lab in Bulgaria than a US doctor’s office.
A doctor’s former receptionist is arrested in Connecticut for using the practice’s computer system to create narcotics prescriptions for herself.

iPhone/iPad EMR vendor Drchrono adds the ability for practices to process patient payments using the Square credit card reader. Square just announced that its reader will be sold at Walgreens and Staples stores or can be ordered at no cost from its site, with swipe card transactions charged at 2.75%.
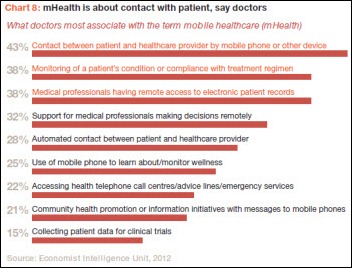
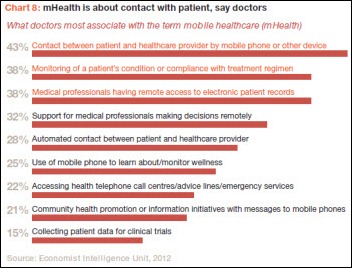
A PwC report concludes that patients want mobile health to provide convenience or save them money, while doctors have less interest unless it can improve care, ease patient access, or reduce in administrative time. The report also predicts that change-resistant providers will slow mHealth adoption as everybody tries to protect their own turf, with the best chances for adoption being developing countries, and that the entitlement attitude of patients means that vendors need to appeal to payers.
eHealth Saskatchewan finds a computer problem that prevented diagnostic imaging results for about 100 patients from being faxed to their doctors for several weeks.
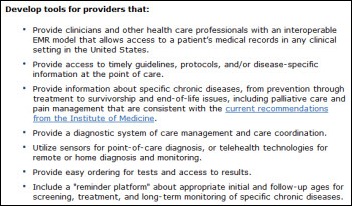
A group of high-profile healthcare CEOs and the Institute of Medicine develop a 10-point checklist of actions that can reduce costs and improve care. Among them: program hard stops into the CPOE system for duplicate lab test orders, requiring the prescriber to call the lab to override the block.
An editorial in the local paper by Mark Herzog, president and CEO of Holy Family Hospital (WI), talks up the hospital’s EMR. He goofs in his description of the one specific benefit by saying that in bar code medication verification, nurses “scan prescription bottles.” I would hope isn’t the case because only clueless hospitals dispense medications in bottles instead of unit dose packages, but I figure he dumbed it down for the lay folks.
Weird News Andy says clinicians must have had a flaccid response to this patient. He’s suing a Yale-New Haven Hospital emergency facility, claiming that staff watched a baseball game on TV instead of treating his priapism.
Sponsor Updates
- Black Book Market Research ranks Certify Data Systems third out of 20 private core HIE system vendors.
- HealthMEDX’s Bridgette Leonard offers advice on auditing EHRs to reduce readmissions.
- The California Health Information Partnership and Services Organization awards Family Health Care Network of Visalia (CA) $573,750 to advance its use of MED3OOO’s EHR.
- CTG Health Solutions releases CTGTALK 4.0, which allows users to manage the application via mobile devices or PCs.
- Nuesoft announces that its NueMD Android EMR app will be available this summer.
- RelayHealth launches RelayAnalytics Pulse, a comparative analytics solution for hospitals and health systems.
- Practice Fusion releases a 10,000-record HIPAA-compliant dataset and launches a data challenge to solve public health issues
- Western Kentucky Orthopaedic & Neurosurgical Associates selects SRS EHR for its 11 physicians.
EPtalk by Dr. Jayne
The HIMSS Virtual Conference & Expo began this week. Keynote speakers included MedVirginia CEO Michael Matthews and political commentator Jonathan Alter.
When I’m teaching students and residents, I often challenge them to use non-medical search engines such as Google in addition to “traditional” platforms for finding medical information. A recent study in the Journal of Medical Internet Research found that identical searches performed using multiple search engines will produce different results. Since two-thirds of physicians and an even greater number of patients use standard Internet search engines to find medical information, the doctrine of caveat emptor becomes increasingly relevant.

In follow up to my piece on goat farming, a reader shared this story about a pediatrician’s frozen yogurt shops along the Jersey Shore. I know a lot of primary care physicians who have left medicine (or who have gone part time) and can’t help but think that if the pay were better the impending primary shortage would look different.
I wrote last month about medical schools compressing coursework for students choosing primary care careers. The American Board of Family Medicine, the Association of Family Medicine Residency Directors, and TransforMED are now working in cahoots to expand family practice residency training to four years. I don’t disagree that it will provide additional educational opportunities to trainees, but extending training (which translates to lost lifetime income for family docs) to an already-depressed specialty isn’t going to help recruit new family docs.

CMS keeps e-mailing me with reminders that Version 5010 Enforcement is almost here. The discretion period ends June 20, 2012 and practices that are still experiencing issues should work with clearinghouses and payers to resolve any problems. I’ve asked my trusted source Bianca Biller to provide a summary of her 5010 experience, but it appears she’s so busy fighting fires that she hasn’t had time to write.

Travis from HIStalk Mobile shared a link on Twitter that discussed whether so-called “sunshine laws” really work. These laws require drug and device manufacturers to disclose payments to physicians. I don’t see drug reps any more, but recently encountered this with a medical device manufacturer rep who wanted my NPI and state license number before buying me a drink. Since I’d already authorized purchase of tens of thousands of dollars in hardware, I didn’t think one Cosmopolitan celebrating the closing of the deal was going to cause an ethical lapse. Although I know my state license number from memory, I was particularly glad that my OCD had led me to store my NPI in the contacts section of my phone.
Speaking of phones, MSN reports that nearly 20% of smart phone users are sexting or otherwise sharing explicit photos or text messages. The most common age groups are men aged 18-34 and women aged 35-44. The report states, “only 3 percent of American adults who are smart phone owners say their biggest concern about losing their phone is that their inappropriate pictures or text messages could be exposed… this number is shockingly low when you consider that 69 percent of smartphone owners have lost their phone.” Grammatical issues aside, I find the quote surprising. If I ever lose my phone, I hope the finder is titillated by the sassy acronyms found within: CCHIT, ONC, HIPAA, EDI, PCMH, and HL7.
Have tantalizing news? Let me know on Twitter @JayneHIStalkMD, on Facebook, or if you’re old-school, e-mail me.

Health Datapalooza from the Eyes of an Entrepreneur
By Dan Wilson

Our company, Moxe Health, was invited by HHS to attend the Health Datapalooza (HDI Forum) because of a product we designed during the Milwaukee BuildHealth Hack-a-thon seven weeks ago. Triage.me was our response to a challenge posed by Aurora Health Care: "Reduce the number of ED visits for non-emergent care in Milwaukee County."
I first learned about the Datapalooza listening to Todd Park’s presentation at the HIMSS conference. We had no idea we were going to be participating until a month ago. Talking with other folks around the event, our experience wasn’t unique. In a sense, Datapalooza is a large-scale agile conference. Hosted by the government. For healthcare. It’s pretty wild.
The last conference I went to was HIMSS. The Datapalooza is definitively not HIMSS.


As an exhibitor, we had the same amount of space as IBM, Aetna, and SAS. Specifically, an 8×8 booth, with nothing allowed to hang overhead and no swag over $10. It was refreshingly low key. Also, startups didn’t pay for their own booth (thanks, HHS!) That’s Mark and me in the Moxe / triage.me booth. We were among the first to set up on Monday. Really nice convention space.
This is the closest you’ll see to the government holding a startup event. They pulled it off, and a lot of respect is due to the folks at HHS and the ONC. Todd Park deservedly gets a lot of the attention, with some folks (HHS Secretary Kathleen Sebelius) even referring to it as the "Todd Park Roadshow." But the event was much bigger than that, and it’s clear there’s a lot of momentum propelling it event forward.
As further evidence of the underlying focus on innovation, one of the most anticipated sessions was held in a side room to make sure the Wednesday afternoon app demos could be simulcast online. While two youngbloods from Wisconsin (and the other code-a-thon winners) were presenting their product on the main stage being simulcast across the nation, Atul Gawande and Farzad Mostashari were facilitating an ACO breakout in a relatively small, overheated room with spotty Internet connectivity. We’re not sure if this was by design or by accident, but the it reinforced the statement that the only thing bigger than the technologists innovating things at the HDI was Bon Jovi (who aside from his noble work for the homeless, also innovated the technological wonder that is "Living on a Prayer.")
Even the ACO event panelists were made up of a number of small, yet terribly innovative companies. One example I learned about was Forward Health Group, a 20-employee company that’s coming up with awesome ways to connect and visualize data. They’re now working with the Guideline Advantage program, which is a collaboration of the American Heart Associate, American Cancer Society, and the American Diabetes Association.
From our standpoint, the event was a huge success. As a young company, we gained incredible insight and valuable contacts from ONC, HHS, and private enterprise leadership. I’m excited to see where the Datapalooza goes next, and I’ll be doing everything I can to stay involved.
Random Musings
- The bow tie is in vogue around the ONC.
- The new Healthdata.gov site launched. I spoke with one of the guys who helped program it. His take is that structurally, the site is a step forward and a good foundation for releasing better data. He also felt that the currently available data/APIs weren’t much changed and there’s still a ton of work required to make sure the data being opened up is both valuable and usable.
- Kathleen Sebelius mentioned that another 150 ACO organizations are slated to start in July.
- VC investment is up 60% in the HIT sector since 2009.
- From Kathleen S.: a recent diabetes study showed patients cared for by a doctor using an EHR had a 600% better chance of receiving the right care.
- I think Bill Frist summed up the focus of the conference well: "The goal is to turn data into discovery."
Dan Wilson is CEO and Mark Olechesky is CTO of MOX eHealth, LLC.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.


































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…