Top News

SAIC announces Q2 results: revenue up 8%, EPS $0.32 vs. $0.32, beating expectations on revenue and meeting on earnings. The company announced plans to split itself into two independent, publicly traded companies, one offering technical services and the other delivering solutions. Healthcare will be part of the solutions business. Shares are up 10% in after hours trading. SAIC acquired Vitalize Consulting Solutions in August 2011 and maxIT Healthcare in August 2012.
Reader Comments
From Klinger: “Re: Epic support. I always heard it was second to none, but what I’m getting is lacking. Have other people noticed, or is it just the TSs that I have?”
From Palmetto Jack: “Re: Palmetto Health. Not an affiliate of USC.” Thanks for the correction. Wikipedia says Palmetto Health Richland is affiliated with University of South Carolina and Palmetto Health’s graduate medical education page says the USC School of Medicine is a “partner and close affiliate,” so it’s one kind of affiliate but not another. I don’t really claim to know the difference.
From Honey Badger: “Re: Cerner. Heard a rumor that they will switch to Greenway’s ambulatory clinic EHR product.” Unverified.
HIStalk Announcements and Requests
 This week’s top picks from HIStalk Practice: Consumer Reports publishes ratings on over 500 Minnesota practices. Practice administrators at large groups see a rise in median compensation, while their small practice peers experience a decline. AMA urges CMS to delay the move to ICD-10 by at least two years. Is HealthTap’s model viable in the long term? Physicians give high scores to Amazing Charts, Epic, and the VA’s ambulatory EMR. Practice Wise CEO Julie McGovern advises practices to avoid tackling other projects in the midst of an EMR implementation. We don’t have a Like button for our posts, so the next best thing is to sign up for the e-mail updates on HIStalk Practice. Thanks for reading.
This week’s top picks from HIStalk Practice: Consumer Reports publishes ratings on over 500 Minnesota practices. Practice administrators at large groups see a rise in median compensation, while their small practice peers experience a decline. AMA urges CMS to delay the move to ICD-10 by at least two years. Is HealthTap’s model viable in the long term? Physicians give high scores to Amazing Charts, Epic, and the VA’s ambulatory EMR. Practice Wise CEO Julie McGovern advises practices to avoid tackling other projects in the midst of an EMR implementation. We don’t have a Like button for our posts, so the next best thing is to sign up for the e-mail updates on HIStalk Practice. Thanks for reading.
Listening: new from Dispatch, their first new material since disbanding in 2002. The indie band hoped to draw 10,000 people to its free final concert in its home town of Boston in 2004, but instead became record-holders as the largest independent music concert in history when 166,000 fans came to say goodbye. The band’s mostly Northeastern tour starts in three weeks.

Welcome to new HIStalk Platinum Sponsor Health IT Quality Solutions, a certification program offered by Quest Diagnostics to vendors of ambulatory EHR products that support Quest’s DEX lab orders and results network. The program’s goal is to maximize lab data quality and enhance interoperability for the 500,000 patients per day that use Quest’s testing services. Three certification tiers are available based on solution capabilities, implementation processes, and participation in mutually beneficial activities. The entire program is free for vendors who qualify, with benefits that include customer satisfaction, solution visibility, faster interface approval, and priority access to Quest’s IT staff. Download a brochure and take a look at the several vendors that have already earned certification. Thanks to Quest Diagnostics and Health IT Quality Solutions for supporting HIStalk.
Acquisitions, Funding, Business, and Stock

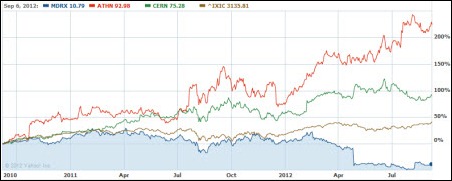
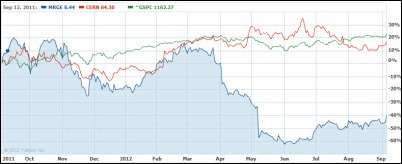
Greenway announces Q4 results: revenue up 24%, EPS $0.07 vs. –$1.09, missing on earnings expectations. The company also projected lower than expected earnings for FY2013. Shares fell 7.1% on the announcement, making GWAY the biggest percentage loser of the day on the New York Stock Exchange. Shares priced at $10 in its February IPO are at $15.27.
Sales
The 300-provider Cornerstone Health Care (NC) selects MedAptus Pro Charge Capture solution for coding and billing.
People


HealthTech Holdings hires Stan Gilbreath (Allscripts) as VP of client services for its HMS and Medhost divisions and Eric Anderton (Jackson Key Practice Solutions) as VP of new account sales for HMS.

Joe Miccio (maxIT Healthcare) joins Divurgent as client services VP.

In Canada, Nancy Martin-Ronson RN, who joined Peterborough Regional Health Centre three months ago as CIO, will also take on the role of chief nursing officer.
Arkansas Governor Mike Beebe names Ancil Lea, executive director of HITArkansas, as coordinator for the Arkansas Office of Health Information Technology.
Announcements and Implementations

The Karmanos Cancer Institute (MI) implements Versus Advantages RTLS in once of its clinics to monitor patient location, track throughput, and manage workflow.
McKesson will offer NovoPath’s anatomic pathology solution to its LIS customers.
Craneware earns CMS’s Electronic Submission of Medical Documentation certification, allowing it to offer customers the ability to electronically submit medical records to review contractors.
Government and Politics
ONC names CCHIT, the Drummond Group, ICSA Labs, InfoGard Laboratories, and Orion Register as certification bodies under the Stage 2 certification program.
Farzad Mostashari says that ONC will not allow EHR vendors to drag their feet in supporting data exchange with competing EHRs.
Other
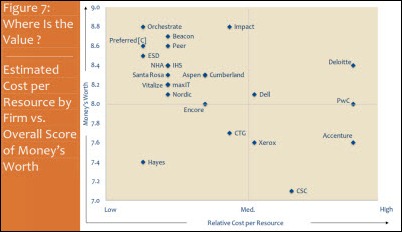
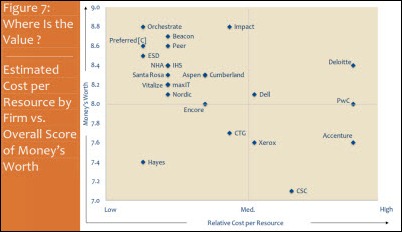
KLAS names its top-rated Meaningful Use consulting firms in three categories: Impact Advisors (enterprise implementation leadership and advisory); Cumberland Consulting (team implementation leadership and advisory); and Navin, Haffty, & Associates (team implementation leadership and staffing). Of the 51 firms identified, more than half achieved satisfaction scores of 89 or above out of 100.
SCI Solutions announces record growth for the first six months of 2012, with 82 hospitals choosing its solutions for care coordination, referral management, and scheduling.
Queens Health Network (NY) honors Congressman Joe Crowley for supporting ARRA, which will pay the hospitals and clinics of New York City Health and Hospitals Corporation up to $200 million.
Madison Memorial Hospital (ID) unblocks access to Facebook from its wireless network after patient complaints. One employee said it was “stupid” that as a patient, she couldn’t post photos of her newborn baby on Facebook. A newspaper reader was more rational: “What an inconvenience when we have to go to a hospital and we can’t get on Facebook. I guess most of us in this day and age feel entitled to more than that what we get.”
Real estate sources say that Meditech is finalizing a deal to acquire 200,000 square feet of office space in Foxborough, MA. The company abandoned plans for a Freetown, MA campus earlier this year after running into a mountain of red tape triggered by the discovery of native American artifacts on the property.
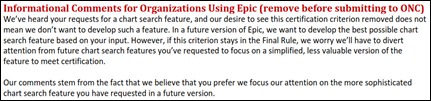
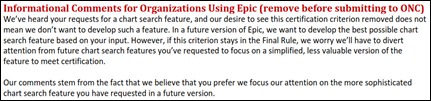
Epic not only submitted MU Stage 2 comments to ONC, it even helpfully distributed them to their customers so they could submit the same comments under their own names. David Clunie noticed this and lists the hospitals who sent in the boilerplate, including University of Miami, which submitted the same comments five times without noticing the “Remove Before Submitting” headline that prefaced Epic’s explanation of why its customers should share its opinions with Uncle Sam.
In Kenya, the country’s hospital insurance fund won’t issue insurance to a man who claims to be 128 years old because its computer system can’t handle birth years before 1890. His family says they don’t appreciate the implication that he should be dead, and until the issue is sorted out, he’s relying on the insurance of his youthful wife of 89.
Odd: a 29-year-old man sues the maker of the sexual enhancement supplement VirilisPro, claiming that the ensuing sex with his partner in a Scottish Inn damaged his manhood to the point that blood was squirting out onto the walls. A physician expert says the man’s story is “the most absurd thing I have heard of in my life,” explaining that men often arrive embarrassed in the ED with damaged sex organs and make up elaborate stories to explain their predicament. He says, “The most common one told is they walked into an ironing board.”
Sponsor Updates
- Billian offers its fellow HIStalk sponsors discounts on first-time purchases of its programs for vendors, including the HealthDATA database and prospecting portal and Porter Research market analysis.
- NextGen will integrate the TRUEresult blood glucose monitoring system from Nipro Diagnostics into NextGen Ambulatory EHR.
- Velocity Data Centers hosts an open house at its Ann Arbor, MI facility on October 25.
- T-System offers two September 5t webinars on attesting to MU with T SystemEV.
- HealthStream expands its suite of products with the addition of NurseCompetency’s exams and skills checklists.
- Cumberland Consulting Group promotes Christopher Miller to principal and Jennifer Vesole to executive consultant.
- Emdeon expands its Clinical Exchange solution to include e-prescription routing, lab orders and results exchange, care alerts, medication history, and clinical messaging.
- Worldwide Clinical Trials selects Merge Healthcare’s eClinical OS solution for data capture, processing, and reporting on clinical trials.
- ICSA Labs hosts two September webinars to help EHR technology developers understand the 2014 Edition certification criteria and testing requirements.
- A CareTech Solutions white paper offers customer insights on achieving Meaningful Use Stage 1 for the 82% of hospitals that haven’t completed it yet.
- Kareo updates its website and branding to reflect its commitment to small practices and billing services.
- TeleTracking invites hospitals to visit its new Enteprise Solution Center in Raleigh, NC to try its capacity management solutions hands on without the time challenges of a site visit.
- An informatica blog post covers Hadoop and big data.
EPtalk by Dr. Jayne
I often wonder how Mr. HIStalk does it all, balancing his day job with his HIStalk duties. He’s done an amazing job for just short of a decade, so when I run across a bit of writer’s block, I know I have no reason to complain.
The last few days have been bereft of ideas. Maybe it’s the weather (I hope all of you in storm-tossed areas are safe) or maybe it’s just the end-of-summer doldrums. I was particularly pleased, though, when an idea squeezed its way into my mind this morning (pun intended, keep reading).
Why All the IT in the World Will Not Fix Health Care
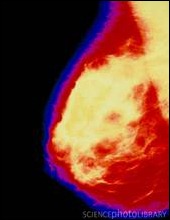
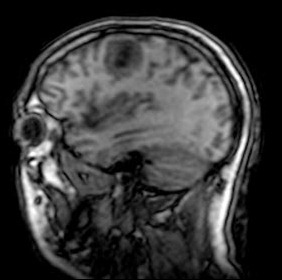
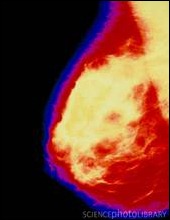
Like many women, I go every year for a certain radiologic screening test. This year’s adventure was a prime example of why technology is not necessarily the answer. There was a fair amount of hassle in my attempts to complete this testing, and it largely revolved around people failing to look at the monitors right in front of them.
First, I had to schedule. As in previous years, I scheduled over the phone. I have my films done at an independent imaging facility, which is funny being the CMIO of a pretty good-sized hospital. Frankly, despite all the HIPAA training, I don’t trust the hospital staff to not discuss employees who are patients. The imaging center also charges half the amount the hospital does, which makes sense with my insurance coverage limits. Plus, I don’t want to have to disrobe for people who I might have to later “counsel” about their bad EHR habits.
The first annoyance was when I was asked (after the staffer pulled up my account) whether I’d been there before. I chalked it up to someone just following a script without thinking about what they were asking. Knowing the billing and scheduling system they use, she should have been able to see the date of my last visit on the patient information screen.
Due to family history, I’m being screened at an age much younger than the standard recommendation. Because of this, I know exactly what my insurer will and will not cover. Luckily, I have a “pseudo health savings account” type of coverage which allows me a lump sum (no pun intended) for preventive services. I can use it as I see fit — exams, labs, tests, etc. — as long as they’re preventive in nature.
The staffer proceeded to argue with me about needing a physician order for the screening test, citing, “Your insurance won’t cover it without an order.” Being a doc (and a savvy patient), I know what they cover and how they cover it. I reminded the scheduler that I’ve never needed an order in the past (especially since my state allows women to have screening mammograms without an order).
She was insistent, so off I went to call a physician. I was tempted to just write my own order, but that would have been too sassy even for me. I just shook my head at the barriers to care that were being placed in front of a paying patient with a valid medical need.
Even though I regularly drink martinis and hang out with my personal physician, I didn’t want to abuse our friendship with something so clearly silly, so I called the office. They unfortunately are pretty early in their EHR transformation and do not yet have a patient portal (which would have been ideal for something like this – e-mail the request, get the order electronically, and be done with it). I survived phone tree hell and reached a nurse (they didn’t have a choice for “Press 3 if you need an order that you don’t really need, but it’s totally not urgent, requires no clinical skill, and you’re embarrassed to even have to ask for it.”) Luckily it was a nurse I know, who laughed with me and agreed to mail the order.
It was with my order in hand that I dutifully arrived 15 minutes early this morning. No one asked for it. After a few minutes of deliberation (while filling out the same information on a paper clipboard that I fill out every year), I decided to proffer the order. The receptionist handed it back to me kindly, telling me they already have my physician’s information on file and don’t need orders for screening tests.
For the actual testing, the imaging center has an excellent facility, caring staff, and “on demand” results, which is another key reason I go there. Who wants to wait to get results in the mail (or even from a patient portal) if you can get them directly from the radiologist while you wait? Especially for cancer-related screenings. If it’s not normal, I want to know right away, so I value the service they provide.
The technician didn’t bother to look at my record, instead asking me if this was my first screening, and if not, how many films have I had and where were they done. At this point, I was ready for a mint julep or perhaps some smelling salts.
Fortunately, the radiologist did take the time to look at the previous films and determine there was no change (which was good, because sometimes I have to have additional views and was spared that particular fun) and came in to chat. He knows I work for Big Hospital and usually has something funny to say about my not using their radiology department. I in turn tease him about the candy-colored kiosks from Merge Healthcare that I tried to get them to purchase a few years ago to spice up their lobby.
I decided to gently broach the details of my experience and my concerns about barriers introduced that might have been important to less-savvy patients. He’s an owner of the facility, so he has a significant interest in the amount of money spent on technology. He seemed genuinely frustrated that employees are using old paper-based processes rather than new ones supported by the technology at hand.
He pulled up my record and showed me that I am clearly flagged as high risk, an existing patient, and as a VIP (although apparently my VIP status is funny to his partners since I’m an exec at the competitor — it seems I’m not the only one.) He plans to address the workflow at the weekly staff meeting, which I appreciate.
Still, as a physician, patient, and payer (aren’t we all payers these days?) I find it striking how difficult it is to achieve ideal healthcare. In my dream world, patients are only asked information once (unless they’re asked to validate their existing information) and the staff uses the information at their fingertips to provide high-quality, expedited care. Even in a facility with a very favorable payer mix, well-paid staff who don’t appear overworked, engaged owners and managers, and a huge IT budget, they’re still part of the healthcare problem, and technology just isn’t going to fix it. Until we start addressing process, procedure, and performance, we’re just throwing money and technology at the problem.

On a lighter (but still feminine) note, an old friend of mine made my week by sending an article about the new Bic pens “for Her.” Of course, I had to go to the actual Amazon UK website and read the reviews for myself. In the words of one of yesterday’s reviewers, “If they made Bic for Her keyboards, I could write this so much easier! Darn my silly lady hands …”

Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.




































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…