Monday Morning Update 7/23/12
From So SARry: “Re: Epic stock ownership. My information is a bit dated, but here’s how it used to work, anyway. Two classes of stock were issued – A and B. Judy owned all the B stock, which I suspect is how she controls the company. In the beginning, anybody could own A stock, and there actually is some stock floating around privately that’s never been owned by an employee, but selling stock like this was discontinued a long time ago. Employees received stock as well, but originally, there was no rule to sell stock when you left. Shares still trade privately, but later employees must sell their stock when they leave the company. At some point, they must have hit the 500-shareholder limit or foresaw this and created Stock Appreciation Rights. New employees from that point got SARS. While they advertise that they are the same as stock, the rules are quite different, mainly in that you can only hold a SAR for so long, which limits its appreciation. Pretty scammy, actually. Employees getting SARS get pretty small numbers. No new employee gets stock, and with the older employees leaving and being forced to sell their stock in most cases, the ownership of the company is increasingly concentrated into certain long-time employees (certainly not all) who get the repurchased stock from the other employees as bonuses. They don’t advertise that, either. There are probably in the neighborhood of 150 employee shareholders or less now.”
From Ossia: “Re: Surescripts. Was offline this week.” Unverified, but above is a snip of an explanatory e-mail that clients supposedly were sent.
From Emu: “Re: MU attestations by vendor. Do you know of anybody keeping these stats up to date and publicly available?” I don’t follow it much, so I’ll defer to Inga or readers who may know.
Listening: Baby Woodrose, a dead ringer for fuzz guitar / organ / tambourine paisley psychedelic rock bands from the Sunset Strip in the late ‘60s (The Seeds, 13th Floor Elevators), surprising since it’s basically one guy from Denmark with occasional rotating backup musicians. Luckily nobody was in the vicinity when I fired up the first few tunes on Spotify because someone could have been harmed by my involuntarily spastic desk drumming. This tune ought to be hit, other than nobody listens much to real music these days. Baby Woodrose just rips it up and leaves it on the stage. I like it a lot. Similarly good but from Sweden: The Maharajas.
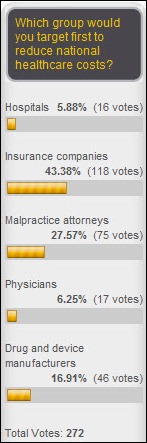
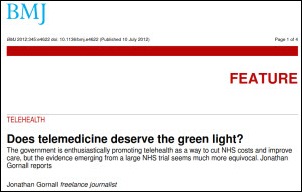
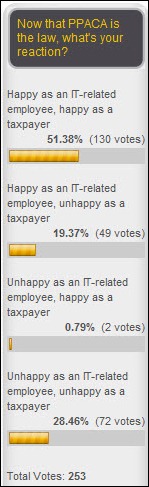
Most readers think the loosely defined “telehealth” will improve quality and costs. New poll to your right: will public HIEs survive?
Welcome to new HIStalk Platinum Sponsor Accent on Integration. As the Texas-based company’s name suggests, its raison d’etre is eliminating data silos via intelligent data exchange, giving hospitals better access to clinical information and thus helping them improve patient care. Areas of focus include interoperability (EMR integration, HIE to HIE integration, accountable care), device integration (monitors, OB and ECG systems), and systems integration (HL7, IHE, CCD, CCR, XML, Web services). Accelero Connect is the company’s enterprise-class clinical data integration platform (vendor-neutral, manufacturer-neutral, and modality-neutral) that connects patient care devices to hospital clinical systems and EMRs, an FDA-registered Medical Device Data System that passed all tests in the Patient Care Device Domain of the 2012 IHE Connectathon. Hospitals that use bedside monitoring systems from multiple manufacturers or that need to capture data from multiple modalities (IV pumps, ventilators, wired or wireless patient care devices, etc.) get a consistent message structure for sending information from those devices to their clinical systems. Clinicians can choose specific incoming data points to include in their EMR documentation (since most EMRs can’t handle a constant barrage of frequent data readings) or the whole process can be placed on autopilot by setting IHE’s device observation filter to pass through only the desired information. Stillwater Medical Center (OK) chose Accelero Connect after an ICU monitoring system upgrade to automatically integrate patient information into the EMR, reducing the time and errors involved with having nurses document manually and giving physicians a real-time view into patient condition to allow faster intervention. Thanks to Accent on Integration for supporting HIStalk.
I’ve warned a couple of times that Meaningful Use attestation is based on the honor system only to a point: HHS has said from the beginning that audits would be done after the fact. They’ve started, apparently, despite the lack of a formal announcement. Providers are getting letters from Medicare cost auditors Figliozzi and Company (check out their ultra-cheesy 1990s FrontPage site, which will shatter any confidence you may have had in them as technologically astute auditors) requesting specific MU-related documentation: a copy of their product’s certification, an explanation of how they calculated ED admissions, and supporting documentation to back up meeting the core and menu set items claimed. CMS awarded Figliozzi a three-year, $3 million contract in April to do the job.
Integrity Transitional Hospital (TX), a 54-bed long-term acute care hospital, chooses HCS INTERACTANT EMR and financial solutions.
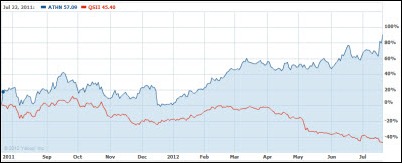
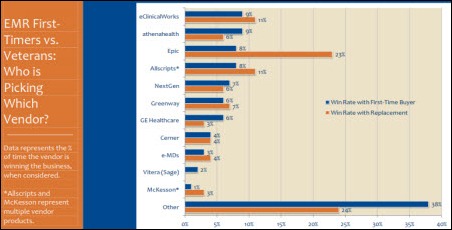
Shares in Quality Systems Inc. continued their slide this week on news that the physician network of Florida-based Health Management Associates will replace QSI’s NextGen products with those from athenahealth. QSII shares that were trading in the $45 range in mid-March closed at $23.41 Friday. Over the past year, ATHN shares are up 78% (they jumped nearly 7% on Friday alone), while QSII’s are down 48%. That’s a one-year chart above. Athenahealth’s market cap is now $3.3 billion, with Jonathan Bush holding about $29 million worth. That makes athenahealth worth only a little less than Allscripts ($1.89 billion), Quality Systems ($1.39 billion), and Greenway ($445 million) combined. You would have more than quadrupled your investment if you’d bought ATHN shares two years ago.
In the athenahealth earnings call, Jonathan Bush outlines some of the company’s strategies: Jedi (adding services such as provider credentialing and denials); Beautiful (improving the user experience in working with the company and engaging design firm IDEO on “future medical record user experiences” and design philosophy); Coordinate (not really explained except to say it’s not working yet); and More Disruption Please (working with other disruptive technology entrepreneurs). Worth reading just to pick out fun JB quotes, which must have the stock guys linting up their suits while rolling on their floors:
- “I had our Physician Advisory Board in yesterday. The biggest thing that they said is, ‘Listen, it makes perfect sense, both as a receiver and as a sender, to be on this Coordinator service. The problem is it’s not really worth doing as a sender unless there’s a lot of receivers, and it’s not worth really doing as a receiver unless there are a lot of senders.’ So I bought five chickens, and I am going to figure out how these freaking eggs get going.”
- [on the replacement system business] “Well, Ryan, thank you for bringing up one of my favorite parts of the athena hospital, the Burn Unit. No question about it, the Burn Unit is getting busier and busier across all segments. I actually saw the KLAS survey did something recently, 30% to 50% — was it 40% to 50%? — of large groups are engaged now in replacing the EMR that they rushed out to buy because they rushed out to buy the one that they knew when the Obama administration told them they needed one, and that was the software-based Flock of Seagulls-era EMR system that they had looked at and chose not to buy in the early 90s.”
- [on increasing sales rep productivity] “So you have a small group guy who’s in her 20s, shows up and she plugs into a desk. It’s like getting on a bull, and the demos come pouring in. And she’s doing demos like the Beatles when they worked at those strip clubs back in the ’60s. They do 10 to 15 shows a day. They get very good very quickly. And you see their close rates pop up into the normal sort of 20% close rate range within a quarter, two quarters max.”
- [on terms of the HMA deal] “They can all leave whenever they want, but hopefully, we don’t get boring. We keep changing our outfits, and they stay forever. We cut our hair short, we let it grow long.”
- [on competing with Allscripts] “I call it O-negative day, that earnings call from Allscripts when they became a universal donor.”
- [on competitors] “It’s our business model that’s on the side of history. Now I am not smarter than those other guys. We didn’t start out better, we’re not better people, we don’t work longer hours. We’re attracting the next generation of brilliant developer because the business model makes sense to people. So over time, we might actually end up with a better raft of people and a more inspired raft of customers. But I really think it really boils down to just the accident of our stumbling upon to this business model, lo those 13 years ago.”
- “We are a nation of shoppers. And the reason healthcare sucks so much, both from a satisfaction and a cost perspective, is nobody’s allowed to shop. It turns out, the way policy has gone, the consumer will not be shopping for a while. That was on the rise. Since the inauguration, that has been on the fall. But it turns out the doctor could shop. The doctor could be the first generation of American shopper for healthcare.”
- “I think this quarter speaks for itself. I do think that we took on, as I said in the beginning of my prepared remarks, more than we could chew. And so we won’t be done chewing by the end of the year in terms of our bolder projects. But anyway, that makes it less hard to figure out what to do next year. And we get the joy and the binding experience that comes from a little bit of failure along the way, which keeps us real because we are so much smaller than this mission we’re on, and we have so much, so much farther to go.”
NIST releases a guide on EMR usability for delivering care to pediatric patients. It’s a free download.
Weird News Andy finds this story interesting. The hospital technician who was charged with infecting at least 30 New Hampshire patients with hepatitis C (he was injecting himself with drugs and then re-using the syringes) was an agency traveler, having worked in at least six states in the past five years. He’s apparently good at sounding sincere – he was reported by a co-worker as “foaming at the mouth” while on the job, but made up a story about crying over a dead relative. What WNA liked is his response to questioning about how all those patients contracted hepatitis: “You know, I’m more concerned about myself, my own well-being.”
Visage Imaging’s server-side rendering and support for Windows, Mac, and iOS platforms is mentioned in an AuntMinnie article covering the technology approaches to developing mobile apps for medical imaging.
Political attack ads aimed at Missouri State Senator Brad Lager, a candidate for lieutenant governor and a part-time Cerner employee, challenge, “While Kinder fights Obamacare, Brad Lager profits from it. Records show a healthcare company that’s made billions from Obamacare pays Lager thousands.” His opponent, the incumbent lieutenant governor, fared even worse – an ad questioned, “Skipping work to hang out at the Horny Toad?”, referring to his admitted visits to a St. Louis strip club of that name and his rumored involvement with a stripper who was plying her trade there.
GE announces Q2 numbers: revenue up 2%, EPS $0.38 vs. $0.35. GE Healthcare contributed profits of $711 million, up from $661 million quarter-over-quarter.
Beth Israel Deaconess Medical Center (MA) notifies 3,900 patients that their PHI has been exposed after a physician’s personal laptop is stolen from hospital property. The hospital was already encrypting its own laptops, and prompted by the incident, now requires non-owned devices to be encrypted before using them to access patient information.
Philips recalls 226 of its Xcelera Connect interface systems after a hospital reports to the FDA that it was sending incomplete cardiology test data to EMRs. The company found that if a physician hit Enter in the summary section of their interpretation, any following information in the report was sometimes lost. Xcelera Connect exchanges data to and from cardiac-related modalities to hospital information systems.
Meditech cloud hosting services provider Park Place International signs on as the first client of CyrusOne, which operates a new Texas data center that it says is ideally located to minimize geographic risk, is connected to highly available electrical and cooling systems, and is hardened with physical security controls.
The 5,800 square foot Memphis house that Steve Jobs secretly bought in 2009 to prepare for his liver transplant there was owned by the University of Tennessee and used as a residence for the chancellor of its Health Science Center. It was appraised for $1.3 million, but the university, anxious to shed some of its residential real estate and spooked by the tanking real estate market and lowball offers on the property, sold the house to Jobs for $850K. After Jobs went back to California, the house was sold to his transplant surgeon.
This amuses me, but then again, it doesn’t take much.






























































... because it's a construction worksite. (It's a bit more evident from the second photo in the linked post.)