Top News

OIG includes “integrity and security of health information systems and data” as one of the top management challenges faced by HHS for 2013.
Reader Comments

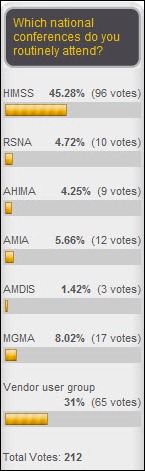
From Image Is Everything: “Re: RSNA. As a vendor, some of us had to go to Chicago the Monday before Thanksgiving and work through the weekend. The trick was to take your spouse, since the Magnificent Mile had beautiful displays, shopping, tourists from around the world, and lots of nice people. The problem was Thanksgiving dinner – think the Chinese restaurant in ‘A Christmas Story.’” I accompanied Mrs. HIStalk to a Chicago conference a few weeks ago, the first time I’d been there since the wintry HIMSS conference of 2009. We had a pretty good time this trip – stayed at the Hyatt on the river, ate at semi-touristy places (XOCO, the Walnut Room, South Water Kitchen, and the Metropolitan Club in Willis Tower), bought Frango Mints, and tried to stay warm since the temperature dropped from the mid-70s the first day to the 40s the rest of the week, ruling out the architecture boat tour. I wouldn’t say Chicago is my favorite city (I think Seattle and San Diego probably top my list), but I at least liked it better than when snow and fellow HIMSS attendees were swirling around me.
From The PACS Designer: “Re: 3D printing. TPD has posted about 3D software solutions in the past, and now you’ll become aware of a retail 3D printer called MakerBot. This company reminds TPD of when Xerox was first to introduce a new way of high quality printing decades ago. MakerBot just opened the first 3D Photo Booth in NYC, its home base, and I’m sure when the photos are viewed, word will spread across the country quickly. Healthcare could benefit by employing this 3D solution to view images of the anatomy, especially the heart, by practitioners and patients undergoing treatment.”
From Keystone: “Re: EMR. I’m involved with five practices being implemented and all are complaining that their efficiency is going backwards because of extra keyboarding. Do you think this is due to added documentation that they should have been doing all along, poor system design, or both? These are mostly primary care physicians and they are definitely seeing fewer patients per session. Also, do you know of bolt-on products to support dictation or other simpler input tools?” Readers, I’m sure Keystone would welcome your comments, which you can add at the end of this post.
From Cloud Dancer: “Re: PACS. Your blog is incredible! Was wondering about your coverage of cloud imaging solutions like Merge as well as other trends in PACS going cloud.” One thing I excel at is recognizing my innumerable limitations, among them being paucity of in-depth knowledge about imaging and lack of time to learn since I’m a full-time hospital employee. I could use an expert contributor if anyone is interested in taking HIStalk a bit deeper into that area. The other areas that people seem to want more coverage about include HIT-impacting federal policy activity, patient-centered technologies, and startups and other innovation. You might think it would be easy to find and engage experts to contribute to HIStalk, but it’s not – they’re either too busy or not all that interested in writing regularly since it’s harder than it looks.
HIStalk Announcements and Requests

 I am back from my Thanksgiving break, which included a bit of holiday shopping. I was remarkably restrained in my purchasing, though I did note quite a few items for my letter to Santa. Topping the list: Christmas tree ornaments for the shoe lover.
I am back from my Thanksgiving break, which included a bit of holiday shopping. I was remarkably restrained in my purchasing, though I did note quite a few items for my letter to Santa. Topping the list: Christmas tree ornaments for the shoe lover.

Thanks for the nice comments folks have sent about the redesign of HIStalk Connect (the artist formerly known as HIStalk Mobile). Next up: a revamp of HIStalk Practice and HIStalk, which will have a different look that’s more appropriate to longer posts. I haven’t changed the appearance of the sites since 2007, so hopefully nobody will be too jarred by the change (me included).
Just in case you have any doubts about the financial literacy of the average American, check out the lines of people waiting to buy tickets for the $500 million Powerball lottery. These are the folks who couldn’t be bothered to play when the prize was only a couple of hundred million. Does that make sense? Do you suppose a lot of statisticians are plunking down their cash given the impossible odds of getting it back? Maybe the feds should run a lottery to help pay down the smothering national debt – it’s like a tax that nobody complains about.

Welcome to new HIStalk Platinum Sponsor Innovative Healthcare Solutions. The 12-year-old Punta Gorda, FL-based company offers clinical and revenue cycle implementation services, with a focus on Epic and McKesson (ambulatory and inpatient EMR, STAR, Pathways, and Horizon, including upgrades and optimization.) They’ve been a Best in KLAS winner for the past two years in the Clinical Implementation – Supportive Work category. They also do assessment, optimization, testing, and strategic planning. Their approach is proven and cost effective, with the recognition that healthcare organizations are required to focus on both financial and clinical excellence for success. The principals have lot of industry experience – Robin Bayne was at McKesson for many years and Pat Stewart has been in healthcare for more than 30 years. Thanks to Innovative Healthcare Solutions for supporting HIStalk.
Acquisitions, Funding, Business, and Stock
Healthrageous announces that Partners HealthCare participated in its recent $6.5 million round of Series B financing.

Hello Health, which offers an EHR platform that’s paid for by patients ($5 per month, according to its site) instead of doctors, secures $11.5 million in financing.

VisionMine launches a service and Web portal that will match small startups with big companies trying to solve specific technology problems. The company will grade startups for the review of the large companies and will coordinate introductions when there’s mutual interest.
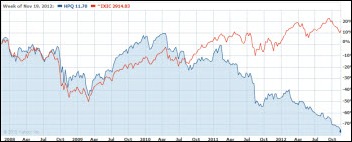
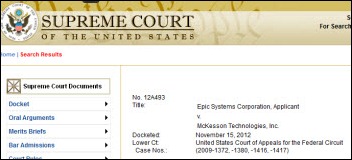
Merge Healthcare files a lawsuit against orthopedics PACS vendor Medstrat, claiming the company’s false claims and unfair business practice have cost Merge tens of millions of dollars in revenue. The suit claims that Medstrat sent e-mails and advertisements to Merge customers implying that the company’s announced plan to seek strategic alternatives was an indication of instability, tagging one e-mail with the phrase, “Why go through more pain? Converting is simple.” MRGE shares closed Tuesday at $3.31, down more than 50 percent since February.
Sales
Valley Medical Group (MA) contracts with eRAD for its PACS and speech recognition solution.
Intermountain Healthcare (UT) signs an $11.7 million, multi-year contract for Siemens Image Sharing and Archiving.
Adventist Health System will expand its use of Cerner’s P2Sentinel solution for auditing clinician access to patient data.

Virtua (NJ) implements the Vergence and proVision identity and access management solutions from Caradigm.
People

Cadence Health (IL) names Dan Kinsella (Optum Insight) CIO and EVP, replacing the recently retired Dave Printz.



Orion Health names Tracey Sharma (Baxter) sales director, Sergei Maxunov (Bell Canada) senior solutions consultant, and Health Linkletter (EMIS) project manager of its Canadian eHealth team.
Announcements and Implementations
HIMSS honors the family practice of Jeremy Bradley, MD (KY) as a winner of the 2012 Ambulatory HIMSS Davis Award of Excellence.
Cerner and telecommunications information company Global Capacity partner to deploy Cerner Skybox Connect, a high availability private network for the healthcare industry.

Children’s of Alabama implements Accelarad’s medical image sharing network to enhance care coordination with referring facilities.

Jefferson Radiology (CT) deploys Repair, a remote MPI management service from Just Associates.
NextGen Healthcare and Microsoft launch NextGen MedicineCabinet, a free app for the Windows 8 platform for the management of personal medication records.
Nuance Healthcare announces Assure for Powerscribe 360 | Reporting, which uses clinical language understanding to QA radiology reports before they’re signed.
Medsphere marks its tenth anniversary by noting that more than 70 percent of its OpenVista customers have achieved Meaningful Use Stage 1 so far.
Wellcentive announces that its Advance Outcomes Manager population health management and analytics solution has earned NCQA certification.
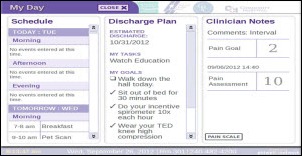
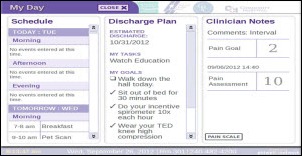
GetWellNetwork and Sharp HealthCare (CA) develop and launch what they say is the first in-room collaborative patient whiteboard. It identifies care team members, tracks visits and family questions, provides a daily schedule and plan, and allows patients to communicate with their family members.

University of West Georgia in Carrollton, GA, whose graduates make up a third of Greenway’s employees, names its new sports stadium building “Athletic Operations Building, sponsored by Greenway, Inc.” and adds the company’s logo to the building.
Cerner lists all of its customers that have successfully attested for Meaningful Use Stage 1.

Chicago-based Valence Health, which offers population management and reimbursement risk management tools and services to providers, announces that its 2012 revenue will increase by 75 percent to over $30 million compared to 2011. The announcement mentions new hires Eric Mollman (Staywell Health Management) as CFO, Kevin Weinstein (ZirMed) as chief marketing officer, and Prasanna Dhungel as VP of product development.
The Panama City, FL paper writes up the expansion of local business iSirona,which also announces that Mercy Medical Center (IA) has contracted for its medical device integration in the OR.
Government and Politics
CMS awards a 10-year, $15 billion contract to eight vendors to compete to build various aspects of a virtual data center for the agency’s IT infrastructure, including claims processing and hosting services for a national data warehouse application.
CMS picks the Kansas City Improvement Consortium, the Health Improvement Collaborative of Greater Cincinnati, and the Oregon Health Care Quality Corporation to be the first organizations to participate in a Medicare claims sharing initiative to assess provider performance.
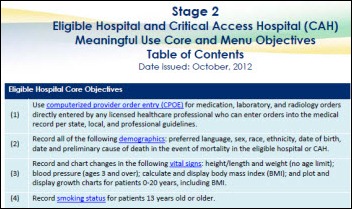
November 30 is the last day for eligible hospitals and critical access hospitals to register and attest for an EHR incentive payment in fiscal year 2012.
Tennessee’s Medicaid program requests $9 million to replace its obsolete IT system with the VA’s VistA.
Other
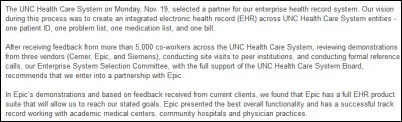
The Madison, WI paper looks at the growth of Epic and its impact on the region. Epic left Madison several years ago for Verona, which has seen huge jumps in property values, but Madison has also benefited by increased demand for rental property and more employment opportunities. Madison city officials say Epic visitors are driving revenue to the hospitality industry, resulting in a 30 percent increase in city room tax receipts from 2010 to 2012.
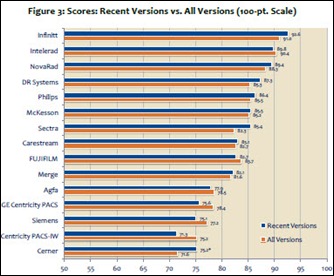
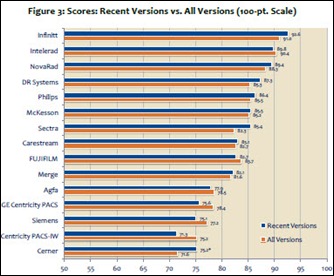
A new KLAS report concludes that the top global radiology PACS vendors vendors are those offering meaningful and timely upgrades with expanded usability. Infinitt and Intelerad rated highly as innovators, along with DR Systems, McKesson, Novarad, and Sectra.
A Weird News Andy literature review notes that two new studies conclude that “flu vaccine is a heart vaccine” since people in the study who got a flu shot experienced 50 percent fewer cardiac events and 40 percent lower heart-related mortality. I’d need to review the original research to feel good about that conclusion, about which I’m skeptical otherwise.
Also from WNA: in the UK, ministers are warned that a plan to implement “virtual clinics” powered by Skype will save billions of pounds immediately, but could leave less technology-savvy patients behind. The Health Minister expects video visits to reduce unnecessary hospital stays, saying that a third of patients can be managed without a face-to-face appointment, leaving more capacity for those who need to be seen in person.
WNA also notes this nugget: the Cincinnati-based TriHealth health system fires the 150 of its 10,800 employees who did not get a mandatory and free flu shot.
I’ve mentioned Italian brain cancer patient (and artist, engineer, and TED fellow, as it turns out) Salvatore Iaconesi several times for his “My Open Source Cure” appeal for treating his condition, much of which involves the struggle to share his records electronically with experts around the world who volunteered to help. CNN ran his story on its main page Tuesday morning. You should watch his newly published TEDx talk above on the challenges created by the medical establishment and his views on wellness and cures (the human being, not the “patient”). I don’t agree with everything he says, but he will definitely make you think, especially if you’ve been a patient with a serious condition. He is exchanging information with 15,000 people and 60 doctors and reviewing 50,000 strategies sent to him with the help of 200 volunteers.
MMRGlobal is awarded a fifth EMR-related patent, proudly proclaiming that despite having supposedly harassed companies into signing $30 million worth of license agreements for its newly-issued patents, the company is not a patent troll since the patented technology is part of products it sells itself. Or tries to, anyway – according to this month’s quarterly filings, the company’s total quarterly revenue was $346,000 with a net loss of $1.5 million, with current liabilities exceeding current assets by $8 million and only $42,000 cash in the bank as it seeks additional financing from its founder and anybody else willing to loan it money. OTC-listed shares are at $0.0147, valuing the whole enterprise at $7 million and obviously reflecting serious market doubt about the company’s banking the $30 million it claims to be owed for its newly created intellectual property portfolio.

Cleveland Medical Mart announces that it has signed Cleveland Clinic and GE Healthcare as tenants. HIMSS, which had signed on with a similar project in Nashville that went bust, has toured the facility, which is three-quarters complete and scheduled for a September 2013 opening.
The local paper in Edmonton, Alberta gets its hands on the expense records of the former CIO of the Capital Health region, whose boss there was found to have been reimbursed $350,000 for questionable expenses that included opera tickets and a butler. Donna Strating, who like her boss was billing $2,700 per day as a consultant, was reimbursed for large restaurant tabs, movie tickets, and snacks.
Sponsor Updates

- Employees of Digital Prospectors supply 30 Thanksgiving meals to the New Hampshire non-profit Families in Transition.
- MModal releases software updates to its Fluency for Imaging Reporting technology platform to support report creation and clinical documentation workflow.
- Merge Healthcare makes its iConnect Enterprise Clinical platform available through EMC Select.
- The GPO Yankee Alliance offers its healthcare members connectivity solutions from Lifepoint Informatics.
- Frost & Sullivan honors Acuo Technologies with its 2012 Market Share Leadership Award in Imaging Informatics.
- Visage Imaging announces a new video about its enterprise imaging platform, Visage 7 – Speed is Everything, at RSNA.
- Frost & Sullivan awards TeraRecon its 2012 New Product Innovation Award in Medical Imaging Informatics.
- Telus Health executives Francois Cote and Brendan Bryne are quoted in a newspaper article on the digital transformation in healthcare.
- The Web Marketing Association awards Imprivata its 2012 WebAward for Outstanding Achievement in Web Development in the Best B2B Website category.
- The Detroit Free Press recognizes CareTech Solutions with its fourth consecutive Top Workplace award in the large company category.
- Frost & Sullivan awards Humedica the 2012 North American Health Data Analytics Customer Value Enhancement award.
- BridgeHead Software releases a white paper outlining strategies for addressing concerns about image availability.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.

















































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…