Monday Morning Update 2/25/13
From Grizzled Veteran: “Re: Stark Act/Anti-Kickback Relief. It’s scheduled to expire on 12/31/13. What are the thoughts on it being extended or not? What happens to hospitals and practices if it isn’t?” The floor is now open. Feel free to leave a comment stating and perhaps defending your opinion.
From CPAhole: “Re: CMS. Has anyone raised the issue of the CMS PQRS site being down for days at a time just when everyone is trying to submit and there is a 72-hour turn on submissions? CMS is trying to come up with a Plan B to fix their system.” Unverified.
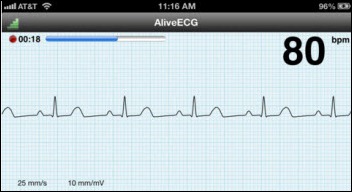
From The PACS Designer: “Re: mobile ECG Monitor. TPD is intrigued by AliveCor’s FDA-cleared Heart Monitor & AliveECG app for the iPhone. An iPhone app that can benefit both the patient and the physician brings health monitoring to a new level of care. This app will be added to TPD’s List of iPhone Apps with the next update.”
From Marrioutta Here: “Re: HIMSS hotel. Just got a call from Marriott. There was an error in their website and they are overbooked. Moving folks 35 miles away and paying for the rooms.” At least when HIMSS e-mailed this week to tell me I was bumped out of the hotel I had booked in September they put me in another one that’s a little bit closer, a little bit cheaper, and newly added to the shuttle route. I don’t like the rooms as much from the description, but it’s walkable to the convention center and closer to restaurants. Some hospitals force employee groups traveling together to share rooms or pay the different for a single room themselves, which would probably greatly reduce the number of rooms required since it’s like a commuter highway – single occupancy is the rule.
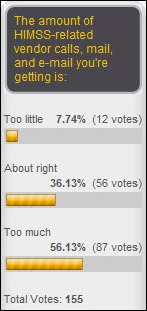
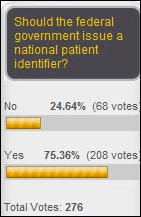
The majority of poll respondents say they’re getting too much HIMSS-related vendor contact, although a solid 36 percent are happy with the volume and a disappointed 12 folks wish they’d get more. New poll to your right: what city would be your choice for holding the HIMSS conference?
Welcome to new HIStalk Platinum Sponsor MediQuant of Brecksville, OH. MediQuant offers Data Transition Management Solutions. Almost every healthcare organization keeps orphaned systems running just because someone might need access to the data they contain at some point. MediQuant’s DataArk active archiving solution allows those systems to be decommissioned with savings of up to 80 percent (using their data center or yours), providing ongoing easy access to clinical, financial, or ERP data. It’s always a pain to work down patient accounts after a system conversion and balance-forward conversions are notoriously risky (why junk up your new system with iffy data?), but DataArk customers can still bill those accounts, post payments, add notes, defend audits, and produce itemized statements with even easier access than the retired system offered. Clinical systems conversions are equally tricky with legacy data and chances are you’re not living in a “no lawsuits after discharge” bubble that allows walking away from years’ worth of patient data, so DataArk allows moving that historical information to its clinical repository module. Turn off the old system and the cash drain required for its upkeep. Other MediQuant products include FirstComply and AccuRules for medical necessity/ABN compliance. The company’s client base includes more than 700 facilities (examples: UPMC, Baptist Louisville, Dignity Health, Kettering Health Network, and West Virginia University Healthcare.) I’m rocking out to their Legacy System Blues by The DeCommissioners on their home page. Drop by Booth #5649 at HIMSS and say hello and thanks to MediQuant for supporting HIStalk.
On the Jobs Page: Demand Generation Specialist, Sales Effectiveness Consultant, Healthcare ECM Sales Executive, Account Manager – Government.
Listening: new from Nick Cave & the Bad Seeds, lush and powerful brooding from one of music’s most tortured geniuses. New live concert video here.
Want to win a $25 Amazon gift card and be sashed on stage at HIStalkapalooza? Tell us why you have a crush on Inga, Dr. Jayne, or Mr. H. We’ll pick the best entry for each crushee and recognize them on stage with an Inga’s Secret Crush, Dr. Jayne’s Secret Crush, or Mr. H’s Secret Crush beauty queen sash as a token of our mutual affection. Speaking of “crushed,” Inga is exactly that so far because all of the entries have been for me (Mr. H). I’m on standby to pledge my affection for her and Dr. Jayne if need be. Mrs. HIStalk assembled and packaged the sashes when they came in the mail last week and was less than thrilled when she got to the “Mr. H’s Secret Crush” one. I told her it was Inga’s idea.
Encore Health Resources will announce this week its Value-based Performance Improvement (VPI), an analytics software and services program developed with Catholic Health Initiatives that includes Meaningful Use reporting, population analysis, clinical analytics for care coordination, and financial analytics. The company says the program will transform EHR data to help organizations focus on quality and performance data at a low cost of entry. Components that can be implemented individually or fully include an analytics engine, an ETL tool, and dashboards.
Georgia Regents Medical Center (recently renamed from Georgia Health Sciences Medical Center) selects Besler Consulting’s BVerified – Transfer DRG tool to identify and recover transfer DRG underpayments. It automates the required review of the Medicare Common Working File and creates workflow tasks that guide the provider through follow-up steps.
Yavapai County, AZ admits that its printing of death certificates was delayed by more than a week due to computer problems following a software upgrade.
The longest article ever published in Time magazine is this week’s cover story on high healthcare prices, Bitter Pill: Why Medical Bills are Killing Us. The basic conclusion is that the US needs to set healthcare rates in a Medicare-type national system instead of letting the so-called free market do so. Most of the criticism is aimed at hospitals, so it’s worth a read even for those of us who working in them even though we were numbed long ago to $2 Tylenol tablets and $300 chest x-rays. The fact that the author couldn’t come up with recommendations less invasive or more likely to succeed than simply letting the government run all healthcare as it does the wasteful, political, and fraud-riddled Medicare program is a bit of a letdown.
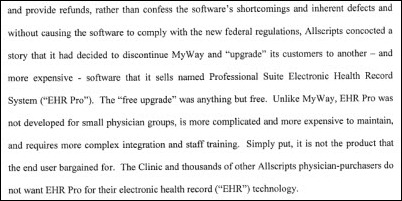
Medical practice plaintiffs who filed a class action lawsuit against Allscripts for its decision to not enable the MyWay EHR for future MU stages or ICD-10 will learn Tuesday whether they can continue with their suit or will instead be forced to accept binding arbitration. If the complaint is certified as a class action, Allscripts will be required to provide the names of all MyWay customers to the plaintiff’s attorneys, who say all 5,000 MyWay physician users would then be automatically included in the suit. Attorneys for Allscripts have filed a motion to block the suit, arguing that the doctors signed a contract requiring their differences to be settled by binding arbitration. Some of the specific complaints, remembering of course that they represent only one side of the argument:
- ”Our EHR is a piece of crap,” said an anesthesiologist and “buggy” according to others involved with the lawsuit, each of which paid up to $40,000 per physician to implement what they claim is a defective system.
- Anesthesiologists claim they were promised a pain management module that was never developed.
- A client who bought MyWay in June 2012 was assured by their Allscripts sales rep that the product would be enhanced to meet MU Stage 2 and ICD-10 requirements, with the company announcing otherwise four months later.
- Users say MyWay, originally developed by iMedica as a client-server product, was sold by Allscripts as a cloud-based offering that performed poorly.
- The lawsuit says that a “free upgrade” to the Allscripts Professional EHR isn’t an upgrade at all since it’s a different product and requires a complicated and costly conversion.
Facebook apologizes to a 104-year-old woman who found that she could not enter her real date of birth on her page. The company changed its date edits to allow birth years before 1910.
Robert Lorsch, chairman and CEO of PHR vendor MMRGlobal, briefs members of a congressional subcommittee on HITECH payouts and what he says is its failure to ensure standardization, interoperability, and PHR access. He demonstrated his company’s PHR product, telling the audience that it could be made available to all Americans for less than the money one large hospital would spend on an EMR. MMRGlobal has sent infringement letters to healthcare IT vendors and hospitals in the US and elsewhere claiming that they are violating the company’s patents that cover a variety of online services.
Vermont’s smallest hospital will lay off 15 employees, 10 percent of its work force, blaming cost pressures created by the Affordable Care Act and its new ACO relationship with OneCare Vermont. Officials with the 19-bed Grace Cottage Hospital defended spending $2 million on an EMR, saying ARRA money paid for it and it needed the system to participate in the ACO.
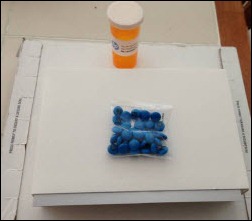
MedSnap releases an iPhone app for medication reconciliation that allows the provider to place a patient’s pills on a tray and use the phone’s camera to take a photo, which the app then analyzes to display the name and strength of each drug along with drug-drug interactions, drug-disease contraindications, and allergies based on the patient’s medical records. I would characterize this as brilliant. Future offerings include medication reminders and caregiver monitoring. The company is looking for volunteers for its Pill Mapping Project, whose submissions will improve its recognition database. Co-founders Patrick Hymel, MD and Stephen Brossette, MD, PhD founded MedMined, the infection surveillance software company acquired by Cardinal Health in 2006.
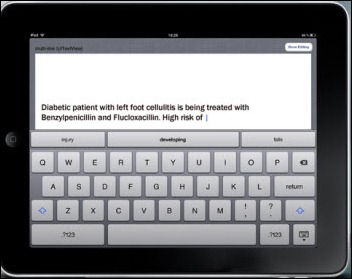
MModal and Intermountain Healthcare will jointly develop a speech-powered CPOE app for iOS devices. The app’s vocabulary will recognize terms related to the ordering of meds, labs, imaging, and nursing. They say it will be completed by fall.
Supporting HIStalk at the Gold level is ReadyDock. Everybody’s walking around hospitals carrying tablets these days, which means they’re also giving a free ride to microorganisms to spread from one patient to another. ReadyDock:UV is the world’s first solution for one-step disinfecting, charging, and securing of tablet PCs and iPads. It’s UV powered, which means no messy wiping down with disinfectant (and no voiding the manufacturer’s warranty by fluid contact). Tablets are often part of normal workflows and charging and disinfecting them needs to be equally user friendly. The device takes up a lot less space than a standard docking station, frees up power outlets, and eliminates a tangle of wires. You can see it yourself at HIMSS in Booth #3879. Thanks to ReadyDock for supporting my work.
I found this brand new ReadyDock video on YouTube featuring Louise-Marie Dembry, MD, MS, MBA, infectious disease professor from Yale-New Haven Hospital.
Thanks to a rumor report from reader Smarty Marty, we reported on February 13 that Aetna was rebranding its health and technology unit (ActiveHealth Management, iTriage, and Medicity) as Healthagen. The official announcement went out Friday.
First Databank promotes Bob Katter and Charles Tuchinda, MD to EVP following the recent promotion of Gregory Dorn to EVP/deputy group head of Hearst Business Media.
Wired profiles stealth startup Smart Scheduling, which identifies patients who are likely to be no-shows for their appointments based on past behavior. The company went through Healthbox’s accelerator program and connected with athenahealth to fine tune its algorithms. The application is being piloted by Steward Health, which uses athenahealth’s scheduling system. The software suggests the optimal time slot for a given patient based on the likelihood they won’t show up. Steward says the program is 95 percent accurate, allowing them to schedule around possible no-shows to hit their overall patient targets.
A mini-study in a Letter to the Editor in NEJM finds that about 12 percent of US physicians have attested to Meaningful Use under the Medicare program, making it likely that many practices will face financial penalties starting in 2015. Specialists have about half the adoption rate of primary care providers. Physicians working with Regional Extension Centers have only a slightly higher attestation rate at 16 percent.
The e-mail system of Ohio State University’s Wexner Medical Center was down for 42 hours through Friday morning, with “replaced infrastructure” identified as the culprit.
UCLA’s medical school is the subject of a snarky Los Angeles Times article that criticizes its cozy relationship with nutritional supplement manufacturer (and accused scam multi-level marketer) Herbalife, which donates a lot of money to the school and drops the school’s name at every opportunity to give its products the scientific credibility that nutritionals sorely lack. UCLA’s cellular and molecular nutrition lab is named for the company’s founder, or as the article says, “The lab is named after Herbalife’s founder, who died in 2000 after a four-day drinking binge — not the greatest advertisement for healthful, active living.” Several medical school faculty members serve on the company’s board, with one of them being paid $17.8 million over 10 years through his consulting firm in return for product endorsements that include his signature on the label. Both he and the company can make almost any exaggerated claim they want since nutritional products escape FDA oversight. The article concludes, “When torrents of cash fall upon people like Heber and Ignarro — especially when the payments promote interests fundamentally in conflict with their responsibilities for thorough, objective research — it’s proper to ask whether the recipients should be viewed primarily as university professors with an income source on the side, or as agents of industry exploiting their academic titles for show.”
Vince wraps up NextGen’s HIStory this week. He starts the long history of Meditech next time and welcomes your contributions.
HIMSS Conference
HIStalk’s Guide to HIMSS13
HIStalk’s Guide to HIMSS13 Meet-Ups
HIStalk’s Guide to HIMSS13 Exhibitor Giveaways
Sponsor Updates
- At the HIMSS conference, HITPC member Gayle Harrell will present a session titled “Leading Change through Health Information Technology” on Monday, March 4 at 2:00 p.m. at Sunquest’s Booth # 911.
- Edward Fotsch, MD (CEO, PDR Network) and Douglas Gentile, MD, MBA (CMO, Allscripts) will present “Turning Patient Portals into Major EHR Assets” on Wednesday, March 6 at 8:30 a.m. in Room 288 of convention center. The session will also be streamed live.
- PatientPay is named by PYMNTS.com as a finalist for a 2013 Innovator Award in the Best Debit category.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.

































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…