Download a printable PDF of the guide here.
Accent on Integration® (AOI®)

Booth: Interoperability Showcase, Use Case #8
Contact: Marc C. Andiel, Co-founder, President and CEO
MAndiel@AOI.biz
972.422.8609, 214.417.3618
Accent on Integration® (AOI®) enables data sharing by interconnecting disparate technology systems and patient care devices for hospitals and healthcare systems of all sizes to improve patient care by enhancing clinical workflows, eliminating error-prone processes and removing data silos. AOI’s Accelero Connect® integration platform is vendor, manufacturer and modality neutral and used to openly communicate clinical data between a multitude of systems and devices.
AOI was selected to participate in the HIMSS Interoperability Showcase and demonstrate live how Accelero Connect can integrate vital signs monitors, smart infusion pumps and telemetry beds with an HIS. At the show, AOI can be found in the demo area for Use Case No.8, which will illustrate the role integration plays as a patient moves through a hospital from the ED to ICU and then discharge.
AOI’s team of seasoned professionals is dedicated to uniting people, process and technology, and they look forward to meeting with you at HIMSS to discuss your integration goals.
Acuo Technologies

Booth 2859
Contact: Mike Dolan, Vice President of Sales
mdolan@acuotech.com
952.905.3448
Acuo Technologies® is the world leader in clinical content management and data migration technology. Our Universal Clinical Platform (UCP) is an enterprise solution built on a next-generation vendor neutral archive (VNA). UCP helps healthcare organizations achieve full interoperability across multiple disparate systems by consolidating long-term data management. UCP unlocks clinical content held captive in departmental systems, providing extreme data liquidity that eliminates migration headaches and accelerates patient data to the point of need. With VNA implementation experience that spans all major PACS vendors and storage providers, Acuo is focused on making all components of a healthcare ecosystem work better together.
In January 2013, Acuo became part of Perceptive Software from Lexmark. The combination of Perceptive’s content management capabilities and Acuo’s VNA platform provides the ability to capture, manage and access all unstructured content to clinicians exactly where and when they need it. The combined offerings provide capabilities to quickly search and extract relevant information from this captured content, and deliver it in the context of the clinical applications. It allows Acuo and Perceptive to bring “high definition” to the EMR and is unique in the healthcare space.
Acuo brings clinical content into the context of the patient record in the EMR, just as Perceptive Software brings unstructured content into the context of the EMR or other enterprise application. Together Perceptive Software’s rich process and content solutions, combined with Acuo’s Universal Clinical Platform, gives users an enterprise-wide view of all patient medical information from within the EMR system. This gives physicians immediate and convenient access to all patient information—from x-rays, ultrasounds, CT scans and more, regardless of the department in which it was conducted or the proprietary technology used to create and store it.
Access

Booth 1023
Contact: Lindsey Eaton, Senior Inside Sales Representative
lindsey.eaton@accessefm.com
913.752.9938
Hundreds of hospitals worldwide use Access solutions to integrate e-forms, electronic patient signatures and clinical data into EHRs without paper or user effort. See Access solutions in action at HIMSS Booth 1023. Oh, and we’ll have free Starbucks coffee, so that’s a win, win for you and your caffeine habit. Watch our customers’ video testimonials here: http://www.youtube.com/accesseforms. And check out our website to learn how we can help your hospital improve patient care and safety while saving you time, money and paper: www.accessefm.com.
Advisory Board Company

Booth 4669
Contact: Meghan Fassl, Manager
FasslM@advisory.com
202.266.6528
The Advisory Board Company is a global research, technology, and consulting firm partnering with 150,000 leaders in 3,700+ organizations across health care. Stop by booth #4669 to meet our team of IT experts, schedule a one on one session with analyst on your topic of choice, pick up our newly released research, attend an education session, and learn more about our Health Care IT Suite memberships.
Allscripts

Booth 3441
Contact: Ariana Nikitas, Director of External Relations
ariana.nikitas@allscripts.com
312.506.1236
The changes underway in healthcare require provider organizations to be Open. Open to change. Open to collaboration. Open to innovation. And Open to the information and insights that lead to improved outcomes. Allscripts Open architecture connects both clinical and financial data across every setting – whether you’re interested in care coordination, revenue cycle, performance management or mobility improvements. This openness brings us closer to our vision of a Connected Community of Health. Join us in booth #3441 to learn more how being Open is driving amazing outcomes across the healthcare industry.
AirStrip

Booth 1721
Contact: Kimberly Kuzawa, Executive Assistant
kimberlykuzawa@airstriptech.com
832.330.4419
AirStrip is guided by a bold vision: harness the power of mobile communications to change the way healthcare is practiced. The AirStrip™ ONE™ mobility solution can improve the quality and timeliness of care, can increase patient and clinician satisfaction, can enhance financial performance, and reduce risk. Headquartered in San Antonio, Texas, AirStrip is empowering the nation’s leading health systems to compete and succeed in today’s rapidly changing environment.
Sign up for a demo or meeting with us at HIMSS – visit www.airstriptech.com for more information. Also make sure to stop by the AirStrip booth and enter our drawing to win a free iPad.
Aprima Medical Software

Booth 6323
Contact: salesinfo@aprima.com
866.960.6890
Aprima Offers a Lifeline to Customers of Allscripts MyWay ™, including Community settings. If your organization is currently using Allscripts MyWay ™ for individual practices, or across an entire Community, you’ll want to stop by Aprima Booth 6323 at HIMSS and learn about the Aprima Rescue Program for customers of Allscripts MyWay™. With this program, you’ll be able to take advantage of free Aprima licenses – up to an $8,500 savings per provider! Plus, Aprima can easily handle your interfaces and interoperability needs. The Allscripts MyWay™ product was originally based on source code that Allscripts licensed from Aprima in 2008, so Aprima EHR and PM have the same look and feel with nearly 1,000 enhancements since 2008. When you upgrade to Aprima, you’ll enjoy a minimal learning curve and minimal to no downtime. For more information, please visit www.aprima.com/rescue or email salesinfo@aprima.com.
Aspen Advisors

To schedule a meeting:
Contact: Daniel Herman, Founder and Managing Principal
dherman@aspenadvisors.net
412.370.4900
We know that technology is a means to an end and have a razor-sharp focus on helping you make progress toward the IHI’s Triple Aim of better health, better healthcare, and lower per capita costs. From strategy to execution to optimization, we can help you:
- Develop your technology roadmap to support the shift from volume-based to value-based care
- Evaluate EMR vendors and plan for implementation
- Streamline governance and decision making
- Plan for mergers, acquisitions and other outreach strategies
- Implement clinical systems, drive adoption and achieve Meaningful Use
- Complete ICD-10 implementation and audit compliance
- Make real progress on teleHealth, eHealth and mHealth initiatives
- Implement infrastructure changes to your technology roadmap
- Leverage information and big data to create a data-driven culture
- Realize value from EHR and other systems investments
- Lead change and support performance improvement initiatives
- Optimize IT service delivery
- Plan for long-range IT workforce needs
Visit www.aspenadvisors.net to learn more.
AT&T

Booth 3727
Contact: Deborah Sunday, Marketing Director
ds823e@att.com
678.230.3440
Join the AT&T ForHealth team in Booth #3727 at HIMSS13 in New Orleans, March 3 -7. AT&T ForHealth is committed to serving the technology needs across the continuum of care – from hospitals to physicians to patients. Our suite of innovative wireless, cloud-based and networking services and applications empower clinicians by placing vital patient health information at their fingertips. Medical images are stored and shared through the cloud, across multiple care settings, highly-secure and on demand. With telehealth, patients get greater access to specialty care and physicians and specialists reach more patients. And with mobile health solutions, patients become more engaged in their own care.
Aventura

Booth 4011
Contact: Jon Cooper, VP of Strategic Initiatives, Co-Founder
jon.cooper@aventurahq.com
303.912.7623
For clinicians, technology can be a real pain in the distal orifice of the alimentary canal.And the more information clinicians need at the point of care, the worse the pain is going to get. Stop by booth #4011 and Suite #202 to see how this pain can be treated.
We know a thing or two about giving caregivers the mobility they need. It’s all about context! Who you are, where you are, and what you need. Aventura’s context- and location-aware intelligence improves the workflow of doctors and nurses by delivering the right information instantly based on clinician location and credentials.
Aventura improves clinician satisfaction, increases EMR use at the point of care, and allows focus on the quality of care. We make your EMR live up to the promises in the owner’s manual.
Awarepoint

Booth 6918
Contact: Carlene Anteau VP, Product Marketing
canteau@awarepoint.com
858.345.5000 x742
Awarepoint optimizes healthcare workflow by offering the industry’s only cloud-based, RTLS solution including software, technology, and managed services. Awarepoint’s experience, reliability and proven solutions drive positive clinical and financial outcomes. Organizations leverage current IT investments to improve communication, enhance coordination, streamline workflow, improve staff efficiency, optimize patient throughput and increase patient and staff satisfaction. Attendees should visit Awarepoint’s booth to learn how RTLS can improve patient flow in a variety of ways ranging from simple automation, such as documenting activities and time stamps based on caregiver, patient and equipment location, to complex milestone management that relates the interactions between caregivers, patients and equipment, to care ordered in the electronic medical record (EMR). The ability to interpret activities and anticipate roadblocks in the patient’s care plan supports proactive communication to drive action.
New product alert: Awarepoint will be demonstrating a new "Bed and Bay Sensor" that enables precise tracking of mobile equipment and patient and caregiver interactions in locations with tight-bed spacing, such as the emergency department (ED) and pre- and post-anesthesia care.
Beacon Partners

Booth 4729
Contact: Jeannette Pforr, Marketing Associate
jpforr@beaconpartners.com
781.681.7493
Beacon Partners is one of the largest healthcare management consulting firms in North America. We focus on helping organizations enhance operational performance to deliver the highest level of patient care. For more than two decades, healthcare leaders have chosen Beacon Partners to optimize clinical productivity and financial performance, ultimately leading to improved quality, safety and patient outcomes. Our team of industry executives, physicians, nurses, administrators, allied healthcare professionals and analysts brings a unique, multi-disciplinary approach to the challenges you face. We are healthcare professionals just like you. That’s the Beacon Partners difference. Be sure to stop by our booth to find out how Beacon Partners can help your organization.
BESLER Consulting

To schedule a meeting:
Contact: Jim Hoffman, Chief Operating Officer
jhoffman@besler.com
732.233.5008
For over 25 years, BESLER has helped hospitals recover otherwise lost revenue, increase reimbursement, ensure compliance, improve efficiency and reduce costs. BESLER’s deep domain experience in revenue cycle, reimbursement, compliance and unmatched software solutions has resulted in more than one billion dollars in additional revenue for our clients. If you’d like to discuss our products or partnership opportunities at HIMMS, please contact Jim Hoffman at 732-233-5008 or jhoffman@besler.com.
Billian’s HealthDATA / Porter Research

Booth 2317
Contact: Jennifer Dennard, Social Marketing Director
jdennard@billian.com
678.569.4872
Billian’s HealthDATA and Porter Research offer a broad spectrum of market intelligence solutions at HIMSS13:
- Provider Solutions
- ID referral partner opportunities
- Compare peer performance
- Review patient market share
- Vendor Solutions
- Broadest lead & email coverage
- Integrated health market coverage
- In-depth data in flexible formats
Need help with your go-to-market strategy? Let actionable feedback from target C-suite buyers guide you with custom market research programs from Porter Research. Schedule your show-floor demo or consultation and get a Starbucks gift card at the booth: http://ow.ly/hjHqw,
Bottomline Technologies

Booth 2619, Hall D
Contact: Michael Kortan VP, Healthcare
mkortan@bottomline.com
603.501.5185
Bottomline’s intuitive, data-driven solutions for patient access and financial process automation are used by 900+ U.S. hospitals. Customers apply our products for patient registration, mobile data and e-signature capture, and cash management to deliver positive patient experiences, improve data and operational efficiencies, and enhance organizational health. Stop by HALL D Booth 2619 for your free Data DNA test and enter to win one of our daily prizes.
CAP Professional Services

To schedule a meeting:
Contact: Bruce R. Cattie, Senior Managing Director
CAPSTS@cap.org
847.832.7700
CAP Professional Services provides best practice health IT strategies, clinical informatics, and terminology services for clients striving to achieve semantic interoperability and high-quality, robust electronic medical records (EMR).
CapSite

Booth 4929 and across from registration in Lobby D
Contact: Gino Johnson, VP, Business Development & Consulting, HIMSS Analytics; Founder, CapSite
Gino.Johnson@himssanalytics.org
802.922.9971
CapSite, now part of HIMSS Analytics, provides detailed health IT data via the CapSite Database, as well as strategic and tactical consulting services. Visit the HIMSS Analytics – CapSite booths in Lobby D and on the exhibit floor (#4929) for a CapSite Database demo to see how our pricing, packaging and positioning information can help with your capital planning and procurement processes or competitor analysis.
Capsule Tech, Inc.

Booths 3711, 3185, and 8711
Contact: Brianna Roy, Marketing and Events Coordinator
briannar@capsuletech.com
978.482.2339
Capsule is the leading global provider of medical device connectivity solutions for hospitals and healthcare organizations. Capsule enables hospitals using electronic medical records and other information systems to reduce costs, increase efficiency and improve patient care through the direct capture and delivery of patient vitals at the point-of-care. Capsule’s solutions are flexible and scalable, offering a variety of deployment options to meet the needs of any healthcare delivery organization. Founded in 1997, the Company has established strong partnerships with leading medical device manufacturers and installed enterprise-wide solutions in over 1200 hospitals in 36 countries.
For more information, visit www.capsuletech.com or call +1 978-482-2337 (US), or +33 1 5334 1400 (France). Over 1,100 hospitals have chosen Capsule for device integration because our solutions are:
- RELIED ON by nurses
- Capsule’s solution was designed with nurses, for nurses to fit current workflows and eliminate charting duplication
- WANTED by I.T. teams
- Capsule works with existing devices, systems and infrastructures
- NEEDED by patients – Capsule reduces nurse charting time allowing for greater focus on direct patient care.
Caradigm

Booth 1323
Contact: Debbie Wolti
info@caradigm.com
Formed by GE Healthcare and Microsoft Corp. in June 2012, Caradigm is a joint venture focused on enabling health systems and payers to drive continuous improvements in care. Caradigm software helps healthcare professionals across care settings to use data to gain critical insights, collaborate with each other and with patients, and to develop and implement innovative care solutions to address some of healthcare’s biggest challenges.
Come by booth #1323 to see:
- EXCITING DEMOS – Check out new Caradigm and partner offerings.
- ENLIGHTENING CUSTOMER PRESENTATIONS – Come hear theater presentations about industry trends and best practices from your peers.
- INFORMATIVE CARADIGM PRESENTATIONS – Learn about Caradigm’s vision, new products we’re delivering and plans for the future.
- CARADIGM PERSONNEL – Stop by the booth to chat with our team, get your questions answered and learn more about new Caradigm.
CareTech Solutions

Booth 1911
Contact: Colleen Hanley, Vice President, Marketing
colleen.hanley@caretech.com
248.823.0950
CareTech Solutions is a healthcare IT services company providing 24x7x365 IT support for more than 200 hospitals/health systems in the U.S.
HIMSS13 attendees should visit CareTech’s booth (1911) to experience, first-hand, the company’s Clinical Help Desk and how it resolves clinical IT issues fast – getting doctors and nurses back to what matters most, providing quality patient care. From iPad video stations, attendees can watch and listen to CareTech analysts resolving EMR application issues in a matter of seconds, not minutes.
Certify Data Systems

Booth 717
Contact: David Caldwell, Chief Marketing and Sales
sales@certifydatasystems.com
408.236.7494
Certify Data Systems, Inc., is a pioneer in health information exchange (HIE) technology. The company’s HealthLogix™ Enterprise HIE platform has been adopted by the nation’s leading hospitals, physicians and laboratories. Certify’s HIE platform provides bi-directional community-wide semantic interoperability between disparate Electronic Health Record (EHR) systems, enabling all healthcare providers to exchange essential health information in real-time. In addition to processing electronic orders and results, the HealthLogix HIE platform delivers Continuity of Care Documents and Clinical Document Architecture seamlessly across a healthcare ecosystem. Certify’s industry leading “network approach” is easy to deploy, scale, manage and support.
Visit us at HIMSS13 in booth 717. Certify is partnering with the local New Orleans YMCA chapter to support their Strong Communities Campaign. Stop by our booth to learn how you can help promote their goal of living a healthier lifestyle. For more information, please visit http://www.certifydatasystems.com. Follow us on Twitter at @CertifyData.
ChartWise Medical Systems, Inc.

Booth 1961
Contact: Michael Backus, Director of Sales
mbackus@chartwisemed.com
317.774.4414
Visit us at HIMSS to see the first and best computer-assisted clinical documentation improvement application on the market.
ChartWise:CDI brings clinical documentation intelligence to your documentation improvement program. A comprehensive web-based software solution, it utilizes innovative built-in expertise to streamline the documentation improvement process by translating clinical terms, labs, and medications into the diagnostic terms needed for coding.
Featuring electronic queries, a flexible workflow, workflow management, help screens and videos, and reference materials from Coding Clinics and DRG Desk Reference, ChartWise:CDI has all the tools a clinical documentation specialist requires. Role-based functionality, robust on-demand multi-level reporting (from the hospital system down to the nursing unit), and optional Advanced Reporting utilizing business intelligence provide the tools an administrator requires. HL7 interfacing, rigorous data security, and no software to install help ease the burden on the IT department.
ChartWise:CDI changes the world of clinical documentation improvement like no other product or service on the market today.
CIC Advisory

To schedule a meeting:
Contacts: Cynthia Davis, Marcy Stoots, or Robert Johns
cynthiadavis@cicadvisory.com
727.772.3340
CIC Advisory helps hospitals use technology to provide more effective, efficient and safer patient care. Founders Cynthia Davis and Marcy Stoots are former critical care nurses with decades of experience leading fast-track clinical EHR projects. Our methodologies result in high rates of physician and clinician satisfaction and adoption, coordinated patient care processes and improved clinical outcomes.
Call us at 1.727.772.3340 or email cynthiadavis@cicadvisory.com for your invitation to the CIC Advisory hospitality suite at HIMSS13.
Clinithink

To schedule a meeting:
Contact: Nathan Skorick, Business Development
nathan.skorick@clinithink.com
978.296.5282
Robert Miller, VP Sales and Marketing
robert.miller@clinithink.com
978.296.5282
Find out how to turn data into information…
Clinithink was founded in 2009 by two clinicians with 20 years of combined healthcare IT and EHR experience who understood what was possible if you could unlock the unstructured clinical data within an patient records and return it as structured, usable clinical information. The result of their pioneering work is CLiX, Clinithink’s Clinical Natural Language Processing (CNLP) solution.
CLiX intelligently unlocks unstructured data, while preserving its original meaning, to help healthcare organizations access the information they need to improve financial management, improve quality measures and enhance clinical and operational processes.
Cornerstone Advisors Group LLC

To schedule a meeting:
Contact: Mary Berchtold, Vice President
mberchtold@cornerstone-advisors.com
781.254.4013
Cornerstone will have experienced senior level representatives from the EPIC, MEDITECH and Advisory/Strategies consulting service lines at HIMSS. They will be available to meet and discuss services during the conference. Meeting times may be scheduled by contacting Mary Berchtold (mberchtold@cornerstone-advisors.com).
Craneware

To schedule a meeting:
Ann Marie Brown, Executive Vice President of Marketing
a.brown@craneware.com
913.548.2810
Craneware will not be exhibiting at HIMSS but will have several senior executives available to discuss the company, our products, and the role we play in helping hospitals achieve revenue integrity though data normalization.
Craneware is the leader in automated revenue integrity solutions that improve financial performance for healthcare organizations. Craneware’s market-driven, SaaS solutions help hospitals and other healthcare providers more effectively price, charge, code and retain earned revenue for patient care services and supplies. This optimizes reimbursement, increases operational efficiency and minimizes compliance risk. By partnering with Craneware, clients achieve the visibility required to identify, address and prevent revenue leakage.
Founded in 1999, Craneware’s mission is to stop the loss of legitimate revenue owed to healthcare organizations by establishing a culture of revenue integrity within these organizations. Our vision is to be the partner that can be relied on to improve and sustain our customers’ strong financial performance.
Over our history we have come a long way towards achieving this. Today, Craneware has a total of nine core products, spanning four product families: Revenue Cycle, Access Management & Strategic Pricing, Supply Management and Audit & Revenue Recovery. One in four registered U.S. hospitals has chosen Craneware products to help them optimize reimbursement, improve operational efficiency, and minimize compliance risk. To support this growing client base and the company’s future growth prospects, Craneware now employs more than 200 professionals across the US and UK.
CSI Healthcare IT

To schedule a meeting:
Kate Mays, Vice President of Sales
kmays@thecsicompanies.com
904.716.1209
CSI Healthcare IT will be hosting a cocktail reception and dinner at Broussards on Tuesday night March 5 starting at 6:00 pm. Please contact Kate Mays to join.
CSI Healthcare IT is committed to providing the highest standard of consultants and consulting services in the Industry. Our track record speaks for itself. We have a long record of supporting the Project Management, Training, Build, Report Writing, Go Live Support and Interface functions of Health systems nationwide. Today, CSI Healthcare IT has more than 500 permanent and contract staff of experienced, knowledge-based professionals. CSI has been recognized by Inc. Magazine and Staffing Industry Analysts as one of fastest growing privately held companies in the nation. Being privately held enables creativity and flexibility to meet the specific consulting needs of our clients. CSI has the ability to enact quick adjustments to accommodate the ebb and flow of our clients’ staffing and project needs.
Join us for live music and networking Tuesday night at Broussards.
CTG Health Solutions

Booth 3663
Contact: Amanda LeBlanc, Managing Director, Marketing & Communications
amanda.leblanc@ctghs.com
225.772.8865
Computer Task Group, Inc. (NASDAQ: CTGX) is an international IT solutions and services company with over 3,800 employees in North America and Western Europe. Its healthcare division, CTG Health Solutions (CTG), is a leading IT consulting firm dedicated solely to helping provider and payer clients achieve strategic, clinical, financial, and operational objectives by more effectively leveraging IT.
CTG’s comprehensive solution suite includes advisory, implementation, IT and strategic sourcing services— including planning and assessments, vendor selection, EMR implementation and optimization, clinical/business analytics, physician adoption, integration/technology solutions, revenue cycle strategies, legacy and production application management, support and upgrades, and solutions addressing regulatory requirements of ICD-10, meaningful use, and accountable care. CTG has provided technology and business solutions to more than 600 healthcare clients for over 25 years.
Visit CTG at HIMSS booth 3663 for conversations on “getting health IT right.”
dbMotion

Booth 5229
Contact: Kate Kolbrener, Director of Marketing
katek@dbmotion.com
412.802.2248
The dbMotion™ Solution is a proven, connected healthcare, SOA-based interoperability platform that enables healthcare organizations and health information exchanges (HIEs) to meaningfully integrate and leverage their information assets, driving improvements in the quality, safety and efficiency of patient care. dbMotion transforms care through the creation of a virtual patient record that integrates patient information to connect care providers and settings.This robust solution is field-proven, having been implemented in some of the world’s most demanding healthcare IT environments since 2001.
Our dbMotion™ Solution is helping clients:
- Access HIE within the Physician Workflow
- Connect the Ambulatory Environment
- Link the Affiliate Community
- Prepare for MU2 and Build an ACO
- Harmonize Clinical Data for Analytics
Come see us at Booth 5229 for a demo! www.dbmotion.com
Dearborn Advisors, LLC

To schedule a meeting:
Contact: Mary Kiley, Revenue Development Coordinator
MKiley@DearbornAdvisors.com
773.255.0749.
Dearborn Advisors would like to chat with you about what’s going on in your organization regarding physician adoption of technology. Although we have no booth, we’ll spring for Starbucks coffee and have hundreds of chocolate bars to give away. Email Mary Kiley (mkiley@dearbornadvisors.com) or call 773-255-0749.
Deloitte

Booth 1863
Contact: Samantha Gordon, National Life Sciences & Health Care Marketing Leader
smgordon@deloitte.com
212.436.4987
By imagining the possible, we help you innovate and seize opportunities. Deloitte can help you in your efforts to define a vision for your organization in the constantly changing world of health care. Through the use of analytics, we can help you in your efforts to make decisions about the future. To do things differently – or make a new way forward.
While you are at HIMSS13, stop by our booth to interact with our analytics products, including Recombinant by Deloitte, the newest addition to our portfolio. Our solution specialists will be available to discuss your pressing issues: Accountable Care, Health Outcomes Management, ICD-10 implementation, Security & Privacy, Meaningful Use, Revenue Cycle, Mobile Health and more.
Visualize clarity through analytics and innovation. For more information visit us at www.deloitte.com/us/himss13.
Direct Consulting Associates

To schedule a meeting:
Contact: Frank Myeroff, Managing Partner
fmyeroff@dc-associates.com
440.996.0051
Direct Consulting Associates (DCA) provides a broad range of IT Consulting and Staffing solutions including staff augmentation, temp-to-perm, and permanent placement for healthcare IT initiatives. Whether you’re an IT professional searching for that perfect opportunity or a client company looking for the very best IT talent, we would like to meet you at HIMSS 2013!
Direct Recruiters, Inc.

To schedule a meeting:
Contact: Mike Silverstein, Director of Healthcare IT
mike@directrecruiters.com
440.996.0594
440.667.8334
Direct Recruiters specializes in recruiting, staffing, search, placement and consulting solutions for the Healthcare Information Technology (IT) Industry.
Divurgent

Booth 5948
Contact: Keri DeSalvo, Marketing Coordinator
keri.desalvo@divurgent.com
757.213.6875
Visit booth #5948 and help Divurgent raise $5,000 to donate to a local New Orleans Children’s Hospital. All we need is your signature!
Divurgent is not the typical healthcare IT consulting firm. As a nationally recognized company, we strive to be different, to think outside of the box for innovative healthcare solutions. Our goal is simple. To transform healthcare to our clients and the communities they serve. Focused on the business of hospitals, health systems and affiliated providers, Divurgent believes successful outcomes are derived from powerful partnerships. Recognizing the unique culture that every organization offers, we leverage the depth of our experienced consulting team to create customized solutions that best meet our client’s goals. Utilizing best practices and methodologies we help improve our client’s operational effectiveness, financial performance and quality of patient care.
Elsevier Clinical Decision Support

Booth 6129
Contact: Che Dildy, Sr. Manager, Product Marketing
c.dildy@elsevier.com
215.239.3795
By integrating insight and action, Elsevier Clinical Decision Support empowers meaningful care through our world-class healthcare information technology solutions, providing a patient-centered approach for organizations to achieve the triple aim.
Emdeon

Booth 5027
Contact: Brian C. Young, Director of Marketing
bcyoung@emdeon.com
404.432.9419
Emdeon provides interoperable information exchange uniting healthcare communities to help improve business and clinical outcomes. Come by booth 5027 to discover how Emdeon can help you achieve your business goals through Emdeon Universal Exchange, and also learn how you can win one of eight iPad minis that will be given out during the show.
Emdeon is the single largest clinical, financial and administrative health information network in the nation. In 2012, we processed nearly 7 billion health information exchanges. Our network moves information between physicians, hospitals, labs, pharmacies and payers through our interoperable connectivity to their software systems. This creates opportunities for access to big data, making it possible to apply intelligent analytics which help drive key programs like care collaboration, accountable care, medical home and pay for performance – all to help you achieve improved quality of care and lower costs with less capital expense.
Emdeon will have 4 in-booth speaking sessions this year, and two iPad minis will be given away at each session!
Session 1: Epic Orders Through Emdeon: Removing the Barriers to Clean Electronic Orders Monday March 4th, 3:00PM – 3:30PM Eric Reynolds, Vice President, Sales and Strategy, Emdeon
Session 2: The Future of Coding is NOW: Maximizing Coding Efficiency and Accuracy Using Big Data and Analytics Tuesday March 5th, 11:00AM – 11:30AM Manjula Iyer, Director of Product Management, Atigeo
Session 3: Breaking the Cycle: How Big Data and Real-Time Analytics Can Help You Intelligently Manage Readmissions Tuesday March 5th, 3:00PM – 3:30PM Gene Boerger, Vice President, Product Innovation, Emdeon
Session 4: Interoperability: The Key to ePrescribing Success Wednesday, March 6th, 11:00AM – 11:30AM Lathe Bigler, Sr. Director, Clinical Services, Emdeon
e-MDs

Booth 6413
Contact: James Foster, Client Data Operations Manager
jfoster@e-mds.com
512.623.6960
Stop By e-MDs Booth Daily for a Chance to Win an iPad Mini!!!
Let e-MDs help you Master Healthcare Strategies. As a consistently top-ranked vendor, clients count on e-MDs to give them the edge they need in meeting tomorrow’s challenges. e-MDs is well-known for our award-winning integrated EHR/PM solutions and services for ambulatory healthcare providers.
We’re introducing exciting new products and initiatives at HIMSS®13 to help you make the right moves to meet the challenging healthcare landscape. Join us at HIMSS®13 where our executive management team will be available to share our vision with you. Learn more about the innovative technology and services we’re delivering that help clients achieve clinical excellence, attain interoperability, drive improvements in patient engagement, and deliver stronger quality measures that support value-based performance, PQRS and MU criteria.
We welcome existing clients, prospects, business partners and other healthcare leaders to visit with us and discuss our latest innovations.
EMRConsultant.com

To schedule a meeting:
Contact: Donna Flynn, Director of Healthcare Technology Solutions
DonnaF@EHRScope.com
888.519.3100 ext. 114
Some things in life truly are FREE! In this case, its receiving the BEST QUALIFIED EHR, PM, Billing and/or Voice Recognition recommendations for your practice, absolutely FREE. How? Use the Comparison Chart, Select Individual Consultant on EHRScope.com, or contact us today with any questions!
Enovate

Booth 7429
Contact: Kevin Dougherty, Marketing and Events Manager
kdougherty@enovateit.com
248.655.0548 ext.154
Enovate is an international manufacturer of mobile and wall mounted computer workstations for the healthcare environment. We provide multiple vehicles for medication delivery, computerized physician order entry, and the implementation for clinical documentation.
We understand that caregivers have enough to worry about. That’s why we work hard to build products that are worry-free—so that caregivers can focus on what really matters, the patient. With comfortable ergonomics, infection control and sustainable materials, Enovate’s products are setting a new standard in the Health Information Technology industry. Light weight, soft corners, and manufactured with antimicrobial materials — these are just a few of the many reasons hospitals choose Enovate products.
Enovate – advancing health information technology For more information, please contact Enovate at (877)258-8030 or visit www.enovateusa.com.
ESD
Booth 5213
Contact: Jessica St. John, Business Development Director
jstjohn@contactesd.com
419.841.3179
ESD is dedicated to assisting healthcare organizations successfully implement health information technology. Experienced, clinical professionals help make that happen thorough full-scale implementation services that assist organizations before, during and after the go-live process to ensure a successful transition to a new or upgraded software. We work with all major systems, such as Allscripts, Cerner, Epic, McKesson, Meditech, NextGen and Siemens.
Stop by and see how we can help make your system work for you!
Etransmedia Technology, Inc

To schedule a meeting:
Contact: Connie Smith, Sales and Marketing
Connie.Smith@etransmedia.com
518.283.5418 ext. 2262
Etransmedia provides comprehensive RCM platform service solutions, including an integration EHR/PM solution, patient identity tools, discrete clinical data repository, provider portal, community patient portal, analytics tools supporting financial, clinical, and quality of care reporting. Delivering RCM and Revenue Analytics services to health systems nationwide, serving 12,000+ providers and 40,000+ users.
FDB (First Databank)

Booth 4241
Contact: Denise Apcar, Brand Communications Manager
dapcar@fdbhealth.com
800.633.3453
First Databank (FDB) provides drug knowledge that helps healthcare professionals make precise medication-related decisions. Come to our booth 4241 at HIMSS13, have a cup of gourmet coffee with us, and meet with FDB specialists to learn more about:
- Achieving Meaningful Use Stage 1/ 2 criteria for medications; get our tip sheet at www.fdbhealth.com/MU2
- AlertSpace®, our latest innovation for better managing alerts within your HIS system – now includes dosage range checking capabilities (in addition to drug allergy, drug-disease, drug-drug interaction and duplicate therapy alert customization capabilities)
- Our State and Federal Controlled Substances Module to simplify compliance with regulations related to controlled substances prescribing and more
- Our High Risk Medication Module™ to identify medications with Box Warnings and/or Risk Evaluation and Mitigation Strategies (REMS)
With thousands of customers worldwide, FDB enables our information system developer partners to deliver a wide range of valuable, useful, and differentiated solutions. For a complete look at our solutions and services please visit www.fdbhealth.com.
Forward Health Group

To schedule a meeting:
Contact: Michael Barbouche, Founder/CEO
FHGtalk@forwardhealthgroup.com
608.729.7530
Let the good times and Fresh Data roll in the Big Easy! Forward Health Group, the Health Care Measurement Company, is intentionally booth-less at HIMSS13 so we can get down, roll up our sleeves and make rich, brainstorming music with health systems, payors and all you newly-minted ACOs. If your focus is population health, you’re going to need tools and help with all that messy data – call us at 608 729 7530 or email us at FHGtalk@forwardhealthgroup.com. We’re on the HIMSS13 show floor – we’ll be right back to you. Let’s have a cafe au lait, spiced with Fresh Data.
With FHG, your data is as fine as the Duck and Andouille Gumbo at Galatoire’s. No, really.
GetWellNetwork, Inc.

Booth 2363
Contact: Tony Cook, Vice President, Marketing
tcook@getwellnetwork.com
240.482.4212
GetWellNetwork provides patient engagement solutions that help health care providers engage, educate and empower patients along the care continuum. Our patient-centered platform, delivered across multiple technology platforms including mobile devices, computers and televisions, enables providers to implement a revolutionary care delivery model called Interactive Patient Care™ to improve performance and patient outcomes. The company further extends the value of existing IT investments by integrating seamlessly with electronic medical record and patient portal applications.
For the third consecutive year GetWellNetwork is recognized by KLAS® as the leader in the Interactive Patient Systems category and exclusively endorsed by the American Hospital Association.Today GetWellNetwork solutions facilitate over 7 million patient interactions.
GetWellNetwork will be showcasing it’s newest solutions – myGetWellNetwork, Interactive Patient Whiteboard and GetWellNetwork for VA Medical Centers. Giveaway – iPads!
Learn more at www.GetWellNetwork.com.
Greenway Medical Technologies

Booth 3941
Contact: Leeann Fleming, National Trade Show Manager
leeannfleming@greenwaymedical.com
866.242.3805
Visit Booth 3941 to learn about the market’s first Cerner-certified interoperability solution for health system alignment and data exchange, and the first EHR to achieve Stage 2 certification. Learn about our high-scoring PCMH service as recognized by the National Committee for Quality Assurance, and our advanced, clinically-driven RCM solutions, all part of the PrimeSUITE platform.
Please visit one of our kiosks located in the Interoperability Showcase, Meaningful Use Pavilion – booth 149/Kiosk C13, or GA HIMSS booth 5500 to receive a key and code that will be taken to our main booth for an opportunity to unlock our safe. Prize value up to $2,000.
About Greenway and PrimeSUITE Greenway Medical Technologies, Inc. (NYSE: GWAY) delivers smarter solutions for smarter healthcare™. PrimeSUITE® — Greenway’s certified and fully integrated electronic health record, practice management and interoperability solution — helps improve care coordination, quality and cost-efficiency as part of a smarter, sustainable healthcare system. Thousands of providers across more than 30 specialties and sub-specialties use on-premise or cloud-based Greenway® solutions in healthcare enterprises, physician practices, clinics and ambulatory clinics nationwide. To learn more, go to www.greenwaymedical.com, Twitter, Facebook or YouTube.
Greythorn

Booth: 5358
Contact: Mary Beth Seaman, Director, Healthcare IT Practice
marybeth.seaman@greythorn.com
425.387.8848
Greythorn is a market leading technology recruitment specialist. Founded in 1976, it has established an excellent reputation for the authoritative and personable service it provides to both its clients and candidates. Since our inception, we have grown globally to provide expertise in Asia, Australia, Ireland, North America, South America and the UK.
With demand in the Healthcare IT sector continually increasing, our commitment to providing an expert and ethical service remains strong, ensuring we remain your ‘consultancy of choice’. Greythorn is part of the global multi-brand recruitment family, FiveTen Group, one of the world’s fastest-growing specialist recruitment consultancies. Visit booth #5358 to discuss industry data gathered from Greythorn’s annual Healthcare IT Market Report, learn about our staffing expertise with various types and volumes of projects and take a moment off of your feet. We look forward to meeting you!
Halfpenny Technologies

Booth 5223
Contact: Brian Muck, Sr. VP of Sales and Marketing
bmuck@halfpenny.com
855.277.9100
Are you using CPOE for lab, diagnostic imaging, pathology, cardiology and other ancillary services? Are your results delivered separately or as one cohesive bundle? Are you able to make business and clinical decisions based on referral patterns and clinical data?
Visit Halfpenny Technologies in booth #5223 at HIMSS13. Learn how your referral base can submit orders and receive customized bundled results with Halfpenny’s ITF-HUB solution. You will gain an additional benefit from the built in business intelligence! You can leverage "true interoperability" with the multi-vendor systems you already have in place, and quickly extract key data allowing you to turn it into actionable intelligence to deliver higher-quality healthcare and gain a competitive edge.
Halfpenny offers solutions for hospitals, health plans, physicians, independent laboratories, diagnostic imaging centers, ancillary healthcare services, HIEs, ACOs and physicians. Stop by to play our “True Interoperability” game, meet our team and win prizes.
Hayes Management Consulting

To schedule a meeting:
Pete Butler, President and CEO
pbutler@hayesmanagement.com
781.414.6099
Hayes Management Consulting is a leading, national healthcare consulting firm focused on healthcare operations. This includes strategic planning, interim leadership, revenue cycle optimization, clinical optimization, project management, IT consulting, and preparation for federal initiatives such as ICD-10, Meaningful Use, and HIPAA compliance. We also provide software such as MDaudit and other proprietary tools to ensure our clients are operationally efficient.
HCI Group

To schedule a meeting:
Contact: Cherity PIerce, Marketing Coordinator
cherity.pierce@thehcigroup.com
904-224-9388
HCI is a leading provider of IT personnel and solutions to healthcare enterprises across the United States, United Kingdom, and Middle East. Our specialties include:
- EHR Planning, Implementation, & Training
- Sustaining Support Models
- Optimization & Clinical Adoption
- Go-Live Support
- Health System/Hospital Community IT Offerings
What makes HCI the best choice for your HIT project? Everything from our collaborative solutions to our rates that translate into real cost savings for your institution. Here’s how we deliver our comprehensive services and expertise:
- Strategic thinking across the entire spectrum of project engagement
- Clinical Leadership and an experienced engagement team to meet your needs in an efficient and timely manner
- Knowledge of industry best practices
- A fully dedicated recruitment team, exclusively focused on Healthcare IT to secure for you the very best resources to make your project a success
HealthCare Anytime

Booth 3869 (ICA)
Contact: Jesse Klick, Vice President – Operations
jesse.klick@healthcareanytime.com
619.243.8333
HealthCare Anytime’s cloud-based enterprise patient portal helps healthcare organizations achieve meaningful patient engagement. Our robust patient portal is delivered in a Software-as-a-Service (SaaS) model, which means we handle hosting, implementation, training, and support, thus reducing the demand on your IT resources.
HealthCare Anytime – Powering Patient Engagement Through the Cloud.
Healthcare Growth Partners

Booth 3845
Contact: Christopher McCord, Managing Director
chris@hgp.com
312.445.8750
Healthcare Growth Partners provides investment banking and strategic advisory services to small and mid-size, high-growth companies with an exclusive focus on healthcare technology and healthcare services. HGP was founded in 2005 with the goal of providing top tier strategic consulting and investment banking services to companies outside of typical middle-market investment bank parameters. Services include mergers and acquisitions, capital formation, strategy, and valuation.Since inception, HGP has closed over 50 transactions. With this focus, the firm leverages its experienced management team, strong execution capabilities, and deep network of contacts within the industry to provide efficient and high value processes for clients, all with the objective of growing companies, realizing value.
Health Catalyst

Booth 7721
Contact: Chris Keller, Marketing Director
chris.keller@healthcatalyst.com
801.230.9223
Health Catalyst (formerly Healthcare Quality Catalyst) delivers a proven, agile data warehouse platform that actually works in today’s transforming healthcare environment.
Currently 81 hospitals caring for 20 million patients utilize Health Catalyst’s Adaptive Data Warehousing platform and solutions. Founded by healthcare veterans who developed their solution after struggling for years to try to make non-healthcare data warehousing solutions work, the Health Catalyst data warehouse utilizes an adaptive approach designed specifically to address the complex nature of healthcare data.Health Catalyst’s platform combines technology solutions and clinical expertise borne out of repeated successful implementations that significantly improved quality of care and reduced healthcare costs.
Health Catalyst’s proven solutions are deployed at leading health systems including Allina Health, Indiana University Health, MultiCare Health System, North Memorial Health Care, Providence Health & Services, Stanford Hospital and Clinics, and Texas Children’s Hospital.
Health Language

Booth 4559
Contact: Marc Horowitz, Senior Vice President, Business Development
Marc.Horowitz@healthlanguage.com
720.320.6663
Health Language, Inc. (HLI) provides software for managing and updating standard and localized healthcare terminology. Health Language also offers clinical content and professional services to enable interoperability, ICD-10 conversion, web-based terminology mapping, and Meaningful Use compliance. Come visit us at booth 4559 to learn more about our robust, innovative solutions for payers, providers, government payers, and healthcare IT and EMR vendors. The HLI solution can assist with your ICD-10 conversion, analytics, and clinical research needs, as well as with pharmaceutical and international applications.
Stop by and see us to learn more, watch one of our informative demos and register to win one of our daily giveaways.
HealthMEDX

Booth 1075
Contact: Denise Johnson, Marketing Coordinator
Denise.Johnson@Healthmedx.com
417.799.6703
The HealthMEDX Vision solution provides an integrated, person-centric CRM, clinical and financial EMR, across the entire LTPAC care continuum including: Long Term Care (SNF, Assisted Living, and Independent Living), Rehab, Homecare, and Hospice. The SaaS based architecture supports interoperability with hospitals, physicians and payers to address readmission management and care coordination challenges across the continuum.
Come see how we embedded the AHRQ On-Time Readmission Prevention program into our solution! HealthMEDX Vision is both CCHIT and ONC-ATCB Certified.
Healthwise

Booth 3885
Contact: Michael Lauber, Account Executive
mlauber@healthwise.org
208.331.6995
Experience the Healthwise Difference. Get an insider’s perspective on what makes the Healthwise® Patient Engagement Solution your best choice for clinicians and their patients. Meet the people behind the Healthwise mission. Experience:
- Trusted information
- Tested interaction
- True innovation
Visit Healthwise at booth 3885. Since 1975, our singular mission has been to help people make better health decisions. Healthwise leads the way with patient-friendly education and ONC-ATCB–certified technology. With Healthwise as your single source for patient education, you meet the criteria for Meaningful Use now, and you’re well positioned for whatever changes the future brings. The Healthwise Patient Engagement Solution.
Henry Elliott & Company Inc.

Booth 3217
Contact: Ken Wagner, President
kwagner@henrye.com
781.820.6697
Henry Elliott & Company, Inc., for over 20 years, has specialized exclusively in the provision of Caché and Healthcare I.T. Professionals for staff augmentation and direct hire nationally. We are a long standing partner of InterSystems and several of our Consultants are Caché Certified Experts who represent an elite level of knowledge of InterSystems products. Our professionals are experienced with Caché based third party software. This includes Epic, Veterans Affairs VistA, Indian Health RPMS, Antrim/Sunquest, IDX(GE) & InterSystems Ensemble, CSP, Zen and others.
We also partner with large-scale Professional Services and Systems Integration Organizations in support of Healthcare I.T. and Caché based technology development and implementation efforts. Our partners provide the project management while we provide the highly skilled professionals. We have grown to 50+ technical resources and 8 Account Management and Operational personnel. Our aim is to match the skills, experience and interests of our professionals with our clients’ specifications.
Holon Solutions

Booth 4020
Contact: Worth Roberts, Vice President Business Solutions
wroberts@holonsolutions.com
678.324.2060
At Holon, we believe that a patient’s experience is improved when their care team can seamlessly collaborate on their care. We understand that information in the right hands, at the right time and place, is key to providing it. We focus on facilitating a collaborative care environment by providing access to information at the point of care – without forcing anyone in the care team to change their current systems or processes.
Visit Holon and our partners in booth 4020 at HIMSS to learn more about how we can help you build a collaborative care environment from the bottom up. Remember when the focus was on patient care? It can be again with Holon!

Booth 7459
Contact: Patricia Kellicker, Director of Marketing
patricia.kellicker@humedica.com
617.475.3800
Humedica is the foremost clinical intelligence company that provides private cloud-based solutions to the health care industry. Humedica’s sophisticated analytics platform transforms disparate data into actionable, real-world insights. Powered by the largest and most comprehensive clinical database, Humedica empowers its partners and customers to make confident, value-based decisions about patient care in a rapidly changing health care market.
Iatric Systems, Inc.

Booth 6613
Contact: John Danahey, Sr. Vice President, Sales and Marketing
john.danahey@iatric.com
978.805.4153
Join Iatric Systems in Booth #6613 at HIMSS 2013. Iatric Systems helps healthcare providers achieve success by delivering the most comprehensive healthcare IT integration. You’ll see how more than 1,000 hospitals are using our data integration, systems integration, and process integration solutions to…
- Achieve a scalable and affordable Enterprise HIE
- Meet ACO objectives
- Support Meaningful Use initiatives
Booth #6613 is going to be entertaining as well as educational, with Chef Anton – the two-time National Pool Trick-Shot Champion – lining up one amazing shot after another and giving out great prizes like Visa gift cards and Apple iPod shuffles after each show.
Make sure you visit us in the HIMSS 2013 Meaningful Use Experience booth #149 / Kiosk #6 and #21. Each day, the first 150 people to visit our kiosks can receive a coupon for $2 off at Starbucks.
Finally, we have teamed up with more than 25 New Orleans retailers to enhance your HIMSS experience by offering special offers and discounts in the area. Stop by booth #6613 to receive your slap band and discount card.
ICA

Booth 3869
Contact: John Tempesco, Chief Marketing Officer
john.tempesco@icainformatics.com
615.866.1465
ICA’s CareAlign® interoperability and informatics platform solves data and communication challenges for healthcare entities, including IDNs, hospitals, IPAs, HIEs, and payers. CareAlign delivers a flexible architecture to connect, collect, consume and intelligently distribute data through Direct, IHE, HL7, and custom methods for use in EHRs, third party applications, and ICA’s applications. Our solution and booth partners are CSC, Healthcare Anytime and Futrix Health. Visit booth #3869 for product demonstrations, and to participate in our food bank raffle. Learn more at www.icainformatics.com, and follow us on Twitter, ICA HITme Blog, Facebook, LinkedIn and YouTube.
ICSA Labs

Booths: 5613 (Verizon); 149 (HIMSS13 Meaningful Use Experience); Interoperability Showcase (IHE USA Certification)
Contact: Amit Trivedi, Healthcare Program Manger
amit.trivedi@icsalabs.com
312.882.1558
ICSA Labs, an independent division of Verizon, offers third-party testing and certification of security and health IT products, as well as network-connected devices, to measure product compliance, reliability and performance for many of the world’s top security vendors. ICSA Labs is an ISO/IEC 17025:2005 accredited and 9001:2008 registered organization. ICSA Labs is NVLAP accredited as a Health IT Test Lab and is also an ONC-Authorized Certification Body (ONC-ACB) accredited by ANSI to ISO/IEC Guide 65. Visit http://www.icsalabs.com for more.
ICSA Labs will the following presentations at the MU Experience Welcome Theater:
- March 5th @ 1:10 pm: Are You Experienced? 2014 Edition Testing – Your Questions Answered
Join Michelle Knighton, Healthcare Testing Manager for ICSA Labs for an interactive Q&A-style discussion focusing on the meaningful use testing process, guidance and tips on how to have a successful test to help your system achieve certification in the ONC 2014 Edition Health IT Certification Program.
- March 6th @ 11:15 am: Are You Experienced? Looking Beyond Meaningful Use and Incentives
Join Amit Trivedi, Healthcare Program Manager for ICSA Labs for an informative discussion focusing on helpful tips and guidance on system selection, implementation, and training to get the most out of your certified EHR technology.
iMDsoft

Booth 7729
Contact: Steve Sperrazza, VP Sales
steve.sperrazza@imd-soft.com
781.449.5567
iMDsoft is a leading provider of Clinical Information Systems for critical, perioperative, and acute care environments. The company’s flagship family of solutions, the MetaVision Suite, was first implemented in 1999. It captures, documents, analyzes, reports and stores the vast amount of patient-related data generated in a hospital. Hospitals worldwide – including 4 of the top 10 US hospitals and 13 of the top 50 European hospitals – use MetaVision to improve care quality, enhance financial results, support research and promote compliance with government, payor, and hospital protocols.
Visit us at Booth #7729 and discover myAnesthesia, our new cloud-based mobile solution for anesthesia documentation featuring a native iPad user interface. Find out about high-impact results reported by MetaVision clients, including:
- 30% reduction in mortality rate
- 100% billable anesthesia procedures
- $1.5M in financial benefits
- 100% elimination of prescription errors
Imprivata

Booth 3717
Contact: Ed Gaudet, Chief Marketing Officer
edgaudet@imprivata.com
Imprivata, the leader in healthcare IT security, enables secure access and collaboration for over two million care providers in more than 1300 healthcare organizations worldwide. Imprivata is the #1 rated SSO Vendor in the 2012 Best in KLAS and Category Leaders Report and SSO market share leader according to HIMSS Analytics. Imprivata Cortext™ is the fastest growing free, HIPAA compliant text messaging solution in healthcare.
Take #MeaningfulSteps with Imprivata at #HIMSS2013
Take #MeaningfulSteps to Imprivata’s booth (#3717) to pick up your free pedometer and enter to win a Jawbone UP every hour. At any time during HIMSS, tweet how many #MeaningfulSteps you’ve taken towards a healthcare IT initiative and you will automatically be entered to win a Jawbone UP. For example, “I’ve taken 3,433 #MeaningfulSteps towards CPOE #HIMSS13”. In addition, Imprivata will be giving away one Kindle every 30 minutes after its booth theatre presentations.
Infor

Booth 2525
Contact: Becky Adams, Director, Global Healthcare Marketing
Becky.Adams@infor.com
651.767,4257
You’ve known us as Lawson. Now, get to know us as Infor. The Infor Healthcare suite of solutions is backed by more than 25 years’ experience creating healthcare-specific technology solutions – as well as major new investments in cloud and mobile technologies that are changing the way healthcare IT works.
Visit us in Booth 2525 at HIMSS and let us show you the solutions that will set your organization on the right path, move your IT strategy forward, and prepare you for wherever tomorrow takes you. While you’re there, enjoy free custom-made espresso drinks and popcorn, and enter to win one of four iPad Minis. If you’d like to learn more about your organization’s path forward for Financials, Supply Chain, HCM, Analytics, and Integration & HIEs, visit go.infor.com/himssdemo to schedule one-on-one time with an Infor representative. When you preschedule and attend a HIMSS demo, you’ll receive a $25 Amazon.com gift card as our thanks.
Informatica Corporation

Booth 5005
Contact: Jonathan Shafer, Healthcare Field Marketing Manager
jshafer@informatica.com
650.385.4434
Stop by Informatica booth 5005 and meet Jonathan Stevenson, Director of Analytics at Ochsner Health System based in New Orleans. Jonathan will be on-site sharing how Oschner has enhanced care coordination through an investment in data. Through their use of Informatica, Ochsner is one of the very first healthcare delivery systems to migrate and integrate large volumes of historical data from a homegrown, legacy EMR into Epic, resulting in a single real-time source for complete patient records, improved visibility for providers, enhanced interactions between patients and providers and rapid and successful migration of clinical data from 38 systems into Epic.
Stop by our booth 5005 and learn why over 4,500 customers, including 84 of the Fortune 100 and hundreds of healthcare organizations have turned to Informatica to help manage their data needs.
Innovative Healthcare Solutions

Booth 3059
Contact: Laura Hudman, VP, Marketing and Sales
Lhudman@ihsconsulting.com
863.602.1787
Innovative Healthcare Solutions (IHS) provides a cost-effective, proven approach to guide and assist healthcare organizations in transitional support, implementation and management of information systems and services. Our expertise includes Planning, Implementation, Project Management, Support and Interim Transitional Services as well as System Assessment, Process & Workflow Design and Optimization for Financial and Clinical systems.
Intellect Resources

To schedule a meeting:
Contact: Tiffany Crenshaw, President and CEO
tcrenshaw@intellectresources.com
336.420.1178
Intellect Resources would love to meet with you!
Intellect Resources is proud to offer comprehensive consulting, recruiting and hiring solutions within the healthcare IT market.Our talent offerings include recruiting, project management, implementation, upgrading and optimization of EMR systems, training and go-live support and the revolutionary Big Break hiring process.Big Break is patented American Idol style audition process where candidates compete to become a healthcare IT trainer. Big Break offers hospitals systems a unique and innovative talent pool at a fraction of the cost of traditional hiring solutions.
In 2012 Intellect Resources was named to The Triad Business Journal’s Fast 50, which adds to a growing list of industry awards Intellect Resources has received including Modern Healthcare Magazine’s Best Places to Work in Healthcare, HITconsultant.net naming Intellect Resources’ President and CEO Tiffany Crenshaw as one of the Top 12 Women to Know in Healthcare IT and the London Times recognizing Intellect Resources’ Big BreakTM as the solution to the healthcare IT talent shortage. A unique approach to standard service offerings sets Intellect Resources apart and allows us to constantly find new and experienced talent.Through relationship-driven, hands-on services, Intellect Resources connects employers and healthcare IT professionals.
For more information visit www.intellectresources.com or www.irbigbreak.com.
Intelligent InSites

Booth 8025, Kiosk #10 in the Intelligent Hospital Pavilion
Contact: Marcus Ruark, Vice President
Marcus.Ruark@intelligentinsites.com
512.541.0737
If you would like to learn how we help healthcare organizations transform their operations with real-time operational intelligence—please come visit us at HIMSS13!
Stop by to experience how our enterprise healthcare software platform will be used across 152 VA Medical Centers to help improve operational efficiency, quality, satisfaction, and compliance—decreasing operational costs, reducing delays in patient care, and increasing clinical efficiencies and staff productivity.
Who we are: Intelligent InSites helps transform healthcare with real-time operational intelligence that improves care, enhances the human experience, and increases efficiency. Through its open, real-time, healthcare platform, Intelligent InSites automatically collects and processes data from multiple data sources such as EHRs, financial systems, building systems, sensory and real-time location systems (RTLS), mobility solutions, and other healthcare IT solutions—then provides actionable intelligence to achieve cost savings, operational excellence, and better care. By utilizing the enterprise-wide architecture of the InSites platform, healthcare systems can leverage all legacy, current, and future data sources to optimize their technology investments across the entire organization, then have the flexibility to meet changing organizational, regulatory, and compliance needs.
For more information, please visit http://www.intelligentinsites.com.
IMO – Intelligent Medical Objects Inc.

Booth 6223
Contact: Dennis Carson, Director, Marketing/Tradeshows
dcarson@e-imo.com
847.272.1242
IMO® – Intelligent Medical Objects will show you how to ‘Work Smarter with IMO’ through the latest developments in interface terminologies that allow clinicians to better capture and preserve true clinical intent and achieve Meaningful Use. Visit us at Booth 6223 at HIMSS13 for our presentations then enter our daily drawings for one of several Bose® QuietComfort® 3 Acoustic Noise Cancelling® headphones.
Presentation topics are:
- Working Smarter with IMO
- All About IMO® Problem (IT)®
- All about IMO® Procedure (IT)®
- Achieving Meaningful Use with IMO
- ICD-10 – How Do I Get There?
- Harnessing the Power of the Semantic Highway
Click to reserve your spot: http://www.e-imo.com/imohimss13.aspx www.e-imo.com
iSirona

Booth 6549 and the Interoperability Showcase
Contact: Peter Witonsky, President & Chief Sales Officer
peter.witonsky@isirona.com
610.772.7648
Visitors to the iSirona booth can register to win one of several Nike+ FuelBands! Stop by to learn about how we’ve been helping clients connect devices to their EMR for several years. It’s their satisfaction that has made our software solution Best in KLAS in device integration for two years running. Don’t forget to hear The Ohio State University Wexner Medical Center on Monday at 9:45! They’ll be sharing their success with medical device integration.
Kareo

Mobile Health Knowledge Center
Contact: Terry Douglas, Director of Brand Marketing
terry.douglas@kareo.com
949.856.7269
If you believe small practices power healthcare and want to see the only company at HIMSS committed to the success and health of small medical practices, then Kareo is the right stop for you! From A/R to mHealth and everything in between, Kareo is the medical office platform of the future.
Check us out in the Mobile Health Knowledge Center, online at www.kareo.com or tweet-out at us @GoKareo.
LDM Group

Booth 5022
Contact: Todd Helmink, VP of Business Development
thelmink@ldmgrp.com
312.391.4233
LDM Group, LLC (LDM), is a leading provider of behavior based prescription management programs. As a targeted healthcare communication company, LDM connects prescribers, pharmacists, and patients. LDM’s network is made up of e-prescribing, electronic medical record (EMR), and electronic health record (EHR) applications, chain and independent pharmacies, and sponsors of healthcare related educational materials. LDM provides timely and clinically relevant healthcare messaging through its patented process which serves to improve patient compliance, persistence and outcomes, while preserving privacy. For more information, please visit www.ldmgrp.com.
Legacy Data Access, LLC

Booths 4611 and 1621
Contact: John Hanggi, Director, Customer Services
jhanggi@legacydataaccess.com
678-232-7922 (cell)
With a singular focus on the healthcare industry, Legacy Data Access stores data from applications – Clinical, Revenue Cycle, ERP, Ancillary, Practice Management and EMR – that are being retired and provides secure, web-based access to the information. Our solutions support financial and clinical processes and strategies by maintaining all detail, minimizing costs, improving productivity, and maximizing ROI.
As a vendor-neutral archive provider, LDA has extensive experience in retiring numerous clinical applications including orders/results, nursing documentation, ancillary applications and in many cases provides a Legal Medical Record for the stored data. Revenue Cycle solutions include receivables functionality so that those systems may be retired earlier. In addition, LDA has retired various PM / EMR systems as well as many ERP applications.
We look forward to seeing you at our booth (4611) and our Partners collaboration booth (1621).
Levi, Ray & Shoup, Inc. (LRS)

To schedule a meeting:
Contact: Ron Peel, Technical Advisor
913.948.3646
ron.peel@lrs.com
Laurie Eldridge, HP Global Alliance Representative
610.850.1237
laurie.eldridge@lrs.com
Levi, Ray & Shoup, Inc. (LRS) is a leader in software for managing care-related documents and other business critical information. Some of the largest healthcare providers in the U.S. use LRS output management solutions. LRS provides documented and supported interfaces to integrate our proven output management software with best-of-breed EMR applications. Contact LRS to learn how we can improve your downtime reporting capabilities and streamline document-related processes to provide better patient care.
Lifepoint Informatics

Booth 7623
Contact: Vincent Gryscavage, Senior Vice President of Sales
vgryscavage@lifepoint.com
201.447.9991 x730
Lifepoint Informatics is a leader in health IT focusing on laboratory outreach connectivity, health information exchange and clinical data interoperability. Since 1999, Lifepoint has enabled over 200 hospitals, clinical labs and anatomic pathology groups to grow their market share and extend their outreach programs through the deployment of its ONC-ATCB certified Web Provider Portal and its comprehensive portfolio of ready-to-go EHR interfaces. For more information visit www.lifepoint.com.
Please Note: Hourly drawings will be made during exhibit hours with a chance to win an Odyssey Golf Putter.
maxIT-VCS

Booth 3027
Contact: Cyndi Vely Cahill, Senior Vice President
Ccahill@getvitalized.com
610.444.1233
maxIT Healthcare and VCS, wholly owned subsidiaries of SAIC, provide a wide variety of clinical, business, and IT solutions for healthcare enterprises across the United States and Canada. With nearly 3,000 consultants, we provide implementation expertise for the Allscripts™, Cerner, Epic, McKesson, MEDITECH, NextGen®, and Siemens systems. We also provide Project Management Professionals (PMP® Certified) and management consulting to assist our clients with their strategic planning and governance needs, tactical project planning, and assistance with their MU, ACO, Revenue Cycle, and ICD-10 project needs.
McKesson

Booth: 4341, Exhibit Hall F
Contact: Erin McNealy, Lead Management
Erin.McNealy2@mckesson.com
404.338.3910
At McKesson, we’re committed to better health for patients, our customers, and the nation’s healthcare system. We’re committed to helping create a new future in which the business of health is better, and the outcomes improved for all. McKesson’s Paragon® “Best in KLAS” hospital information system is an intuitive, single-database system featuring fully integrated clinical and financial applications. Learn more by visiting our HIMSS booth (#4341) or at www.mynewHIS.com.
MED3OOO – Now Part of McKesson

Booth 3068 (Medicomp)
Contact: Nicole Contardo, Corporate Marketing Director
marketing@MED3000.com
888.811.2411
MED3OOO – Now a Part of McKesson, is a leading provider of healthcare management and technology services that improve outcomes for providers, health plans, and the patients and employees they serve. The Company provides a broad array of proprietary solutions for physician groups, hospitals, health systems, health risk organizations, and state and local municipalities, enabling them to reach their maximum potential with respect to operational, financial, and clinical results. Through the integrated application of systems, operations, analytics and domain expertise, MED3OOO serves as the premier strategic operations partner for the healthcare community.
The Company’s depth of knowledge across its services, economies of scale, infrastructure, and ability to offer and manage disparate information systems provide MED3OOO with a distinct competitive advantage in the rapidly evolving healthcare industry. Each of the components of MED3OOO’s product and services suite is a critical competency for moving toward the delivery of accountable care.
MED3OOO will be giving demos of our InteGreat EHR with Quippe in the Medicomp booth (3068).
MedAptus

To schedule a meeting:
Contact: Jennifer Crowley, Marketing Director
jcrowley@medaptus.com
617.896.4030
MedAptus is the Gold Standard in the healthcare revenue cycle for achieving effective charge management, compliance and workflow efficiency. With offerings that include powerful and easy-to-use charge capture and management technologies, it is no wonder that many of the nation’s most prestigious healthcare organizations rely on MedAptus for financial optimization. Our full-scale Professional, Facility and Infusion applications increase revenue, enhance EMR investments, re-engineer manual processes and yield substantially improved productivity.
For more information, visit www.medaptus.com or call 617.896.4000.
MedAssets

To schedule a meeting:
Contact:
solutions@medassets.com
888.883.6332
MedAssets (NASDAQ: MDAS) partners with healthcare providers to improve their financial strength by implementing revenue cycle, spend and clinical resource management solutions that help capture revenue, control cost, improve margins and cash flow, increase regulatory compliance, and optimize operational efficiency. MedAssets serves more than 4,200 hospitals and 100,000 non-acute healthcare providers. The company currently manages $48 billion in supply spend and touches over $340 billion in gross patient revenue annually through its revenue cycle solutions. For more information, go to www.medassets.com.
Medicomp Systems

Booth 3068
Contact: James Aita, Product Manager
jaita@medicomp.com
703.945.2482
Back by popular demand, Medicomp Systems will once again host Quipstar, World’s Favorite HIT Quiz Show, live at Exhibit 3068. Contestants and those seated in the studio audience will have a chance to win one of fifty iPads and other prizes. Best of all, you’ll see how Quippe, backed by the powerful MEDCIN Engine, takes care documentation requirements without burdening the clinician. You can also experience the MEDCIN Engine, Using Medicomp’s new interactive MEDCIN Engine touchscreen you can also experience the MEDCIN Engine to see how MEDCIN can successfully manage the data tsunami and even make SNOWMED easy to use. Register for an opportunity to attend and play Quipstar at www.medicomp.com/quipstar-registration.
Medicomp is also the proud sponsor of HIStalkapalooza, which will be held at the iconic Rock n’ Bowl. Register at www.histalkapalooza.com.
Medicomp Systems is the inventor of clinical content, technologies, and mappings that improve EHR usability at the point of care while taking care of all documentation requirements including Meaningful Use stages 2, 3 and beyond as well as ICD-10.
MediQuant

Booth 5649
Contact: Mindy Morris
mindym@mediquant.com
440.746.2300 x245
MediQuant provides Data Transition Management Solutions that embrace healthcare’s transitory nature. Simplify your IT world and reduce the cost of system conversions with DataArk®, an Active Archiving solution that allows you to decommission old systems, maintain interoperable access to old data, and realize up to 80% cost savings. As the retirement home for the legacy data from retired systems, DataArk® allows users to easily access and view clinical, patient financial, ERP and other data that had been left orphaned in legacy systems. For patient accounting records, users may still bill accounts, post payments and produce itemized statements among other functions.
MediQuant serves a large client base across the nation, including large multi-facility IDN’s (40+ hospitals, 100+ ambulatory practices), academic healthcare organizations and community facilities. FirstComply™ and AccuRules™ are software and content solutions for medical necessity/ABN compliance.
Merge Healthcare

Booth 5725
Contact: Jennifer Jawor, Director, Segment Marketing
jen.jawor@merge.com
312.565.6825
Merge Healthcare is a leading provider of clinical systems and innovations that seek to transform healthcare. Managing over 13,000 billion images, Merge was named the world’s largest vendor-neutral archive (VNA) market leader in a recent InMedica study. As the industry’s first true standalone vendor-neutral archive, iConnect(r) Enterprise Archive has been successfully integrated with over seventy-five PACS vendors and specialty workstations at over 350 sites across the United States. And with MU2 requirements, mandating images available to the referring physician through a certified EHR, Merge’s iConnect Enterprise Clinical Platform can help organizations image-enable the EHR while improving operational efficiencies, reducing costs and increasing revenue potential.
So are you ready for the next level of interoperability? Learn more about enterprise imaging at merge.com or visit us at HIMSS in Booth #5725.
M*Modal

Booth 6647
Contact: Lisa McCormick, Corporate Events Planner
lisa.mccormick@mmodal.com
267.535.7222
Expect More. More from your EHR.
- Maximize physician adoption More time for your physicians.
- Easily capture the complete patient story More meaningful, higher quality patient care.
- Drive more intelligent, effective actions
Surprise Your Favorite Children‘s Charity. Visit M*Modal at HIMSS13, Booth #6647, and enter for a chance to win $800 in toys for the children‘s charity of your choice.
Nordic Consulting Partners

To schedule a meeting:
Contact: Natalee Cruse, Director of Technical Marketing
natalee.cruse@nordicwi.com
608.334.2998
Nordic is ranked #1 in KLAS for Epic services. We’re the largest consulting firm in the country focused exclusively on Epic. Our team of more than 225 elite consultants, two thirds of whom are former Epic, average nine years of industry experience and four certifications. We partner with over 50 clients across the country.
We pride ourselves on having high standards and a partnership-oriented philosophy with our clients and consultants, which has created great rapport and allowed us to attract the best and brightest to Nordic. We take pride in providing the right resource for a given opportunity.
Need help installing? Upgrading? Optimizing? Rolling out to affiliates? We do it all. We’re also an Epic-credentialed provider of Community Connect implementation and support. There will be a fleet of our green-shirted folks at HIMSS – come chat with us about how your Epic project is going!
For more info, go to www.nordicwi.com
nVoq Incorporated

To schedule a meeting:
Contact: Debbi Gillotti, Vice President and General Manager
deborah.gillotti@nvoq.com
720.562.4507 or 206.465.1765
SayIt(TM) from nVoq is a secure cloud-based voice recognition service that’s easy to use, easy to deploy, and has been endorsed by the American Hospital Association. SayIt works directly with your EMR to convert speech to text within seconds – no integration required. Access your SayIt voice profile whenever and wherever you need to work – no software to install on each device.
nVoq is a Boulder, CO based provider of cloud-based voice recognition solutions for the Healthcare and Customer Care industries. In business since 2000, nVoq supports a wide variety of enterprise and health system organizations through a growing channel partner network. We’re building this network daily in support of real-time (front end) dictation and embedded (back end) voice processing for mobile forms or other applications. A well-documented SDK is available for both Windows and iOS platforms.
While attending HIMSS, we welcome the opportunity to meet with organizations who buy, build or implement applications platforms for Healthcare users, and are interested in cloud-based, voice-enabled workflow at an affordable price point. Our primary focus is North America, but we welcome inquiries from other venues.
NTT DATA Healthcare Technologies

Booth 1041
Contact: Larry Kaiser, Senior Marketing Manager
lawrence.kaiser@nttdata.com
631.824.5318
NTT DATA Healthcare Technologies offers healthcare organizations a complete IT solution with applications that increase efficiency, reduce medical errors, and enhance the revenue cycle. NTT DATA’s solutions include ONC-ATCB certified Optimum, featuring one of the industry’s leading RCM solutions, comprehensive clinicals, EHR, general financials, and post-acute solutions. Healthcare Technologies that:
- Empower the Patient
- Improve Care
- Drive Outcomes
Stop by the booth for a chance to win an iPad Mini.
Nuance Communications, Inc

Booth 4025
Contact: Mark Erwich
mark.erwich@nuance.com
781.565.5000
At HIMSS 2013 Nuance will show how to improve the entire clinical documentation process, from the capture of the complete patient record to clinical documentation improvement, coding, compliance and appropriate reimbursement. Nuance will share latest information on how to prepare to transition to ICD-10, how we support Meaningful Use, how we support Mobile health and the transition to Accountable Care.
Optum

Booth 7041
Contact: Steven Loewy, Associate Director, Marketing
steven.loewy@optum.com
801.982.3468
Optum innovations, analytics and expertise help health care organizations navigate the journey from providing care to managing health. Our solutions and services are used at nearly every point in the health care system, from patient access to diagnosis and treatment; from coding and clinical documentation improvement to reimbursement; and from quality measurement and performance benchmarking to network management, administration and payment.
Every day, Optum solutions help shape how health care is managed, and how information and technology drives improvements in the system. Optum works with our clients and partners to improve the delivery, quality and cost effectiveness of health care in ways that support and empower more patient-centered, value-driven care. Visit us at HIMSS13, booth #7041 to learn how Optum can help you reduce costs, while increasing patient care quality and satisfaction.
Make your steps count at HIMSS13! For every mile you walk, Optum will donate $1 to charities that improve health and wellbeing in the City of New Orleans. Stop by the Optum exhibit for a free pedometer and more information.
Orchestrate Healthcare

Booth 529
Contact: Charlie Cook, President
charlie@orchestratehealthcare.com
877.303.3377
We focus on four core competencies: EMR Clinical Implementation, HIE Consulting, Integration and Staff Augmentation. Why? Because QUALITY is our mantra.
We listen to our clients, and our 15+ year experienced consultants are make-it-happen, kind of people that deliver on-time, on-schedule and on-budget. Without errors or excuses. Our client referrals and three Best In KLAS awards in the last five years affirm this. Come see us at booth 529 to learn more about how we can help you. While you’re visiting, check out our new pad and register to win a pair of really cool Beats by Dr. Dre. Listening has never been so much fun!
Orion Health

Booth 3161
Contact: Kristin O’Neill, Senior Marketing Manager
kristin.oneill@orionhealth.com
857.488.4740
Visit booth 3161 at HIMSS 2013 and see for yourself why clinicians, hospitals, health systems, public health organizations and OEM partners in more than 30 countries worldwide rely on Orion Health to provide solutions to their biggest health information exchange (HIE) and data integration challenges. Be sure to mark your calendar for all the Orion Health activities while at the show, including: – Joining us for morning coffee or a sweet afternoon treat at the booth. – Meeting our clients and learning how they are using our solutions. – Entering our raffle to win an iPad mini 4G. – Attending a “Lunch and Learn” session with Shahid Shah, The Healthcare IT Guy, on Data Integration and Analytics: The Future of Healthcare Information Management. – Networking with Orion Health executives over breakfast in our hospitality room.
Orion Health™ HIE facilitates data exchange between hospitals, health systems, regional HIEs, and affiliated providers, resulting in improved care coordination, increased cost savings and efficiencies, and enhanced quality of care. Orion Health™ Rhapsody® Integration Engine provides seamless connectivity between legacy and next-generation health systems, rapidly enabling organizations to deliver high-quality patient care and population health. Rhapsody provides a comprehensive set of tools to simplify healthcare integration and is easily extensible to meet the requirements of each unique healthcare environment.
Ormed Information Systems Inc.

Booth 1041 (with NTT Data Health Solutions)
Contact: Bill Hockstedler, VP Sales and Marketing
bill.hockstedler@ormed.com
512.971.2885
Ormed’s software and services are designed exclusively to continuously improve on the business processes of hospitals in the areas of supply chain management, finance, cost accounting, human capital management, decision support and systems management.
Saving time, reducing waste, cutting expenses, understanding costs, creating a positive experience and peace of mind. In the world of accountable care and new regulations, wouldn’t it be nice to have a set of tools in your hands that were always designed around expense management and accountablility. A powerful Cost Accounting system alone can make all the difference for you!
Come and see what we have to offer to make the changes ahead less stressful!
Park Place International

Booth 2674
Contact: Christine Mellyn, Manager of Product Marketing
christine.mellyn@parkplaceintl.com
508.970.8704
Park Place International provides technology integration, technical consulting, and OpSus|Cloud Services designed to help customers achieve operational sustainability with their MEDITECH Electronic Health Record. Park Place is an approved provider of technology solutions for all versions of the MEDITECH HCIS and offers the full selection of MEDITECH-certified server and storage platforms. The Park Place team has extensive MEDITECH experience and technology expertise, and is uniquely qualified to architect, deliver and support MEDITECH solutions.
Stop by booth #2674 to learn more about Park Place International and enter our raffle for a chance to win an Amazon.com gift card!
Passport Health Communications, Inc.

Booth 3310
Contact: Scott Bagwell, Senior VP, Sales & Marketing
Scott.Bagwell@passporthealth.com
888.661.5657
Founded in 1996, Passport now serves more than 2,400 hospitals in addition to more than 8,900 physicians, clinics and ancillary offices across all 50 states. The company processes more than 300 million transactions annually through its Passport eCare™ brand of patient access and payment certainty solutions. Recently ranked the nation’s third largest revenue cycle management company by Modern Healthcare, Passport was honored as the “Technology Company of the Year” by the Nashville Technology Council in October 2012. Passport’s patient access & payment certainty solutions are delivered through Passport eCare NEXT; an integrated, SaaS-based platform that can be seamlessly integrated into existing work flow. Accountable Care solutions, including ACO MemberMatchTM, can be used to manage patients’ entire course of care, from initial diagnosis through full recovery and can be seamlessly integrated into existing workflow through the Passport eCare NEXT platform.
Visit Passport at Booth #3310 to see a product demonstration and speak to a Passport representative.
PatientKeeper Inc.

Booth 2210
Contact: Kathy Ruggiero, Senior Director, Corporate Marketing
kruggiero@patientkeeper.com
781.373.6433
PatientKeeper is the leading provider of healthcare applications for physicians, with over 50,000 users across North America and the UK. At HIMSS13, visitors can see PatientKeeper software in action and speak with customers who are actively using our CPOE, mobile CPOE, physician documentation, electronic charge capture and other applications that streamline physicians’ workflow. PatientKeeper runs as a native app on popular smartphones and tablets, as well as on desktop and laptop computers. While you are at our HIMSS13 booth (#2210), enter our daily drawing for an Apple iPad mini.
PatientPay

To schedule a meeting:
Contact: David Bond, EVP, Sales & Marketing
db@patientpay.com
919.830.2798
PatientPay is a patented innovative solution that makes healthcare billing, payment and reconciliation faster, easier and less costly. PatientPay is a simple way for practice management software vendors to allow their physicians to bill patients while reducing costs, increasing productivity and patient satisfaction. PatientPay eliminates the costly and complicated paper-based billing method used by the overwhelming majority of healthcare providers. It drives down the expense and drives up the productivity associated with this activity by at least a factor of two. Since PatientPay reduces the time to payment in half, healthcare professionals realize improved cash flow and reduced accounts receivables.
PDR Network

Booth 7740
Contact: Amy Lombardi, Senior Director, Marketing
Amy.Lombardi@pdr.net
201.358.7200
PDR Network® has developed innovations to deliver critical drug information to providers within workflow that are easily integrated into partner EHR systems and deliver a better end user experience. PDR interactive drug information services allow providers to have their PDR in their EHR with services provided at no cost to partner EHRs and their providers, enhancing the overall EHR experience while supporting Meaningful Use (MU) requirements.
- PDR® BRIEF: Supporting providers by delivering the key information needed at the point of prescribing. Instead of accessing multiple sources outside of workflow, providers have access to the information they need within workflow when they need it.
- PDR® Search: This on-demand resource provides access to a host of medication-specific resources covering regulatory, provider and patient information tools, as well as aggregated manufacturer resources. Before providers would leave your environment for these tools, NOW they have integrated access to the information they need.
- RxEvent: PDR offers a quick and easy digital reporting tool that can be easily integrated into any EHR or ePrescribing system.
Ping Identity

Booth 2470
Contact: Linda Bowers, Healthcare Market Leader
lbowers@pingidentity.com
978.844.4105
Ping Identity is The Identity Security Company. Our identity and access management platform gives enterprise customers and employees one-click access to any application from any device. Over 900 companies, including 45 of the Fortune 100, rely on our award-winning products to make the digital world a better experience.
Prognosis HIS

Booth 7423
Contact: Melanie Thompson,Director of Marketing
mthompson@prognosishis.com
713.469.1501
Prognosis Health Information Systems provides an enterprise solution, including EHR and financial systems, to rural and community hospitals. At HIMSS, Prognosis is launching a new version of its highly ranked ChartAccess® EHR and unveiling our ED and ambulatory solutions. We’re introducing the new era of EHRs. Our system allows for configurability at both the organization and user level, helping every person interact with the system in the way that works best for him or her. We invite you to stop by our booth and see an EHR like you’ve never seen before.
Qlik Technologies

Booth 8121
Contact: Kerry Talbot, Event Marketing Senior Manager
kerry.talbot@qlikview.com
617.331.5284
QlikTech (NASDAQ: QLIK) is a leader in Business Discovery—user-driven Business Intelligence (BI). Its QlikView Business Discovery solution bridges the gap between traditional BI solutions and inadequate spreadsheet applications. The in-memory associative search technology QlikTech pioneered created the self-service BI category, allowing users to explore information freely rather than being confined to a predefined path of questions. Appropriate from SMB to the largest global enterprise, QlikView’s self-service analysis can be deployed with data governance in days or weeks. The QlikView Business Discovery platform’s app-driven model works with existing BI solutions, offering an immersive mobile and social, collaborative experience. Headquartered in Radnor, Pennsylvania, QlikTech has offices around the world serving approximately 26,000 customers in over 100 countries.
We will have multiple demos, videos and customer presentations in our large booth amphitheater with solutions experts on hand to answer all of your questions. Registerhere for a personalized VIP Booth Tour and be entered for a chance to win an iPad Mini!
Quantros

Booth 7940
Contact: Amy Lee, Director of Marketing and Sales Operation
info@quantros.com
408.957.3300
Quantros helps healthcare providers improve quality and patient safety by empowering organizations, at every level, with the actionable intelligence they need to improve outcomes and reduce risk. Quantros provides cloud based tools and resources for the healthcare industry in the areas of safety and risk management, quality and performance improvement, accreditation and compliance, and centralized decision support. Today more than 2,000 healthcare facilities use Quantros solutions to capture meaningful data to effectively drive the decisions that improve the safety and quality of care.
Visit our booth to learn more about IRIS and enter to win an iPad. IRIS is a leading-edge clinical quality and patient safety dashboard that leverages data from the Quantros Safety and Risk Management (SRM) solution, the Regulatory Reporting Management (RRM) solution, and your organization’s billing data. IRIS Executive presents this data via a highly configurable, role-based dashboard. The result is real-time visibility into safety and quality events and trends in your facility. This enables you to chart improvement with an authoritative source of truth.
Quest Diagnostics (Care360 Healthcare IT Suite of Solutions)

Booth 3927
Contact: Rohit Nayak,Vice President, Physician Technology Solutions
RNayak@MedPlus.com
800.444.6235
A special 2013 HIMSS invitation to all HIStalk readers: Visit the Quest Diagnostics Healthcare IT Theatre – Booth 3927.
Quest Diagnostics team members will be featuring educational presentations and industry insights from key opinion leaders on technology topics including:
ChartMaxx and Care360 with Data Exchange, part of the Care360 Suite of Healthcare IT Solutions from Quest Diagnostics, are exhibiting together to showcase the strengths of the company’s entire HCIT portfolio. EHR vendors can learn how our Health IT Quality Solutions Program benefits them through streamlined interfacing and promotion of their quality EHR solutions by us.
We are focused on “Empowering Better Health: Quest Diagnostics Healthcare IT Solutions.”
Quest Diagnostics booth representatives will be holding drawings for iPads and other exciting giveaways following each 20-minute presentation.
For more information and a schedule of the presentations, visit Care360.com.
RazorInsights

To schedule a meeting:
Contact: Reed Liggin, President & CEO
rliggin@razorinsights.com
404.578.1362
Based in Kennesaw, Georgia, RazorInsights is a dynamic healthcare information technology company. In keeping with the principle of Occam’s Razor, they have created a simplified HIS solution for Rural, Critical Access and Community hospitals. Introducing ONE (ONC-ATCB 2011/2012) — a single-database, cloud solution offering a simple user experience with cutting-edge clinical tools and industry-standardized data. Hospitals can expect to improve their performance and bottom line with ONE from RazorInsights. To register for a live product demo or for more information, visit www.razorinsights.com or call 770-308-4111.
RelayHealth

Booth 4640
Contact: Lynette Corte, Lead Qualification Manager
lynette.cortez@relayhealth.com
888.743.8735
RelayHealth is proud to be a featured exhibitor at HIMSS13 March 3-7 at the Ernest N. Morial Convention Center in New Orleans. If you plan to attend this important annual industry event, we’d like the opportunity to learn more about your goals and challenges for the upcoming year, and explore how RelayHealth can help you succeed in 2013 and beyond with the Right Connections for Better Health.
RelayHealth provides solutions that can help you satisfy requirements for Meaningful Use Stage 2, and meet your objectives for providing accountable care. As the healthcare industry continues to experience substantial change, RelayHealth is also at the forefront of developments in areas such as health information exchange, patient engagement, and readmission management. Check out the exhibition hall floor map and make plans to stop by for a visit with us in Booth #4640. We look forward to meeting with you in New Orleans.
Salar, Inc.

Booth 6754
Contact: Greg D. Wilson, Director of Sales
gwilson@salarinc.com
860.294.9877
Salar offers physician clinical documentation and charge capture solutions to hospitals and health systems nationwide. Our flagship product, TeamNotes, has recently been entirely rewritten allowing our customers to deploy the solution faster, easier, and to a wider array of devices than ever before. At HIMSS, Salar will showcase this latest release, TeamNotes v6, and within that demonstration special attention will be focused on front end computer assisted coding for ICD-10 compliant documentation, physician charges as derived by the notes themselves, care team collaboration of notes, physician hand off, and related CDI workflows.
In lieu of yet another iPad giveaway or a similar free gizmo, at this time Salar is planning to offer a charitable donation in the name of one visitor to the booth. Details are forthcoming.
Sandlot Solutions

Booth 2063
Contact: Derek Plansky, Senior Director, Client Solutions
dplansky@sandlotsolutions.com
202.747.4502
Sandlot Solutions has a proven, deployed system managing more than 2.8 million lives. Sandlot manages risk, drives clinical management and provides business analytics. All of the things that are required by MU2, and beyond and all the things an Accountable Care Organization (ACO) must do. Sandlot provides all the tools to manage against risk-based payment systems. Most application systems only use claims data for analysis – Sandlot merges clinical and claim data to manage care and manage risk. Sandlot using a Software-as-a-Service (SaaS or cloud computing platform) is very fast, built on reliable technology – system changes for your information systems and changes for any of your affiliated entities are not required . . . also connects to non-affiliated trading partners in your trading area. The combination of Healthcare Information Exchange (HIE), Care Management and Analytics makes Sandlot the Fourth Generation Technology.
Santa Rosa Consulting
To schedule a meeting:
Contact: Doug Hires, Executive Vice President, Strategic Advisory and Sales & Marketing
doughires@santarosaconsulting.com
214.546.0895
Santa Rosa Consulting is a national provider of management consulting and information technology services to the healthcare industry. Through our unique blend of strategic advisory services and technical consulting expertise across the full range of healthcare IT vendor products and systems, we deliver solutions specifically designed to address your business needs.
Seamless Medical Systems

To schedule a meeting:
Contact: Frank Grant, Vice President, Sales
frank@seamlessmedical.com
760.533.1520
Seamless Medical is solely focused on improving the patient’s experience in medical practices at the point of care. Our mission is to leverage technology in patients’ hands to simplify the front end of the practice workflow, engage the patient in the registration process, and provide the patient with educational content relevant to his/her scheduled appointment and medical conditions. Our team’s decades of combined experience in the medical, healthcare administration, and business arenas has led to the formation of the company and dedication to our solution.
Shareable Ink

Booth 3568
Contact: Suzanne Cogan, Vice President, Sales and Marketing
scogan@shareableink.com
877.572.7423 x 802
Shareable Ink is the enterprise cloud-based platform that transforms point-of-care clinical documentation to structured data and analytics. By incorporating natural input tools, such as iPads and digital pen and paper technology, clinicians can continue documenting in the fastest, most efficient manner. The resulting structured and clinically-rich output populates the EHR with discrete data, as if typed in directly. Predictive analytics give hospitals and practices unprecedented insight into their operations – from a clinical, quality, and efficiency standpoint.
Visit us at HIMSS – # 3568 – for an interactive demo of our applications that automate areas where electronic documentation has traditionally been challenging – from anesthesia to patient-generated history to ambulatory sites. We’ll also have a special unveiling of our iPad App – you won’t want to miss it! For everyone who mentions ‘LIBERATE’ at our booth, we’ll be making a donation to one of our favorite NOLA charities.
Siemens Healthcare

Booths 2640 and 2641
Contact: Roger May, Senior Director, Marketing
roger.may@siemens.com
610.219.1874
Join us to learn how a growing number of healthcare organizations—both large and small—are using Soarian® to connect top-of-the-line patient care with the bottom line. Hear the story of how Soarian unites the revenue cycle for seamless financial performance using contract-driven processing. See how Soarian helps foster collaboration by connecting clinicians to patient data and to one another with integrated clinical workflow.Learn how more people in more places can connect… with Soarian. See the new Soarian Ambulatory offering in our main booth and our MobileMD HIE in our adjoining booth.
Stop by the Siemens booth and we will make a contribution to Hope For The Warriors® whose mission is to enhance the quality of life for post-9/11 service members, their families, and families of the fallen who have sustained physical and psychological wounds in the line of duty. www.hopeforthewarriors.org
SpeechRecognition.com

To schedule a meeting:
Contact: William Holliman, Dragon Medical Adviser
William.Holliman@1450.com
888.848.1450 ext. 210
Is your EHR doing all of the dictating? Take back control, and the ability to dictate your notes, with the most accurate speech recognition software yet, Dragon Medical Practice Edition. Visit SpeechRecognition.com to schedule a free demo today!
Streamline Health Solutions, Inc.

Booth 1821
Contact: Michael Schiller, Senior Vice President, Sales, Marketing & Account Management
solutions@streamlinehealth.net
303.316.0696
Streamline Health offers specialized solutions that will:
- Get you closer to Meaningful Use with EHR-integrated enterprise content management solutions
- Provide actionable insight into your organization’s true financial performance with Business Intelligence solutions
- Help facilitate the transition to ICD-10 with our suite of integrated computer assisted coding (CAC) and CDI solutions
Stop by booth 1821 at HIMSS to view a live demonstration of AccessAnyWare™, OpportunityAnyWare™ and/or Collabra™ and learn how Streamline Health Solutions, Inc., can help your healthcare organization successfully face today’s challenges.
SuccessEHS

Booth 4411
Contact: Dante Rankart, Vice President of Sales
marketing@successehs.com
888.879.7302
SuccessEHS is a nationally acclaimed vendor providing Electronic Health Record (EHR) and Practice Management solutions with Integrated Medical Billing Services. SuccessEHS also provides Electronic Dental Record (EDR) and Dental Imaging solutions. Founded in 1995, SuccessEHS established itself as a leader in the emerging practice management applications market by delivering an innovative blend of clinical, operational and financial software paired with a suite of specialized integrated success services. SuccessEHS, entirely in-house developed and supported, has achieved multiple certifications from CCHIT.
Visit us at booth #4411 to learn how SuccessEHS can help practices improve care, increase revenue, successfully manage the ICD-10 transition and earn incentives through Meaningful Use and the Physician Quality Reporting System. While you’re there, spin our wheel to win fun prizes, including cash! We look forward to seeing you in the Big Easy!
Sunquest Information Systems, Inc.

Booth 911 and MU Booth 149, Kiosk 85
Contact: Tracey Eddy, Marketing Event Planner
tracey.eddy@sunquestinfo.com
520.570.2333
Sunquest delivers market-leading diagnostic information technology and outreach solutions, designed and implemented to fulfill the business objectives of today’s healthcare leaders. Sunquest Laboratory is the leader in the market, enabling labs to operate with optimized performance and deliver quality diagnoses, while meeting regulatory and interoperability standards. Our solutions demonstrate a commitment to patient safety, workflow excellence, predictive and personalized medicine, and physician and patient affinity, serving users worldwide. Through outreach, we extend the lab to the community and provide the tools that turn information into intelligence.
At Booth 911:
Monday March 4th @ 2:00 pm
Guest Speaker Representative Gayle B. Harrell, President and CEO of Health IT Strategies, LLC ONC HIT Committee Member, Florida House of Representatives
Subject: Meaningful Use
Tuesday March 5th @ 10:30 AM and 3:00 pm
Guest Speaker Patty Sollman, Blood Bank Supervisor/LIS System Manager, Deaconess Health System
Title: In the age of the Integrated EHR, why SUNQUEST is the RIGHT choice as your Laboratory/Pathology System…..a user perspective
To request a meeting with a member of the Sunquest team at HIMSS please complete a request form: http://info.sunquestinfo.com/HIMSS2013_HIMSS2013v1.html.
Our give away this year will be a miniature plush toy – Sunquest Lab.
Surgical Information Systems (SIS)

Booth 6429, Intelligent Hospital Kiosk 8711-33
Contact: Emmy Weber, VP of Marketing
info@sisfirst.com
678.507.1727
Surgical Information Systems (SIS) provides software solutions that are uniquely designed to add value at every point of the perioperative process. SIS’ singular focus in the OR helps hospitals drive both greater efficiency and better patient outcomes while integrating with your information systems environment. Visit SIS at Booth #6429 to learn how the fast, mobile, connected SIS Solution can help you achieve a "Slam Dunk" in your OR. Rapidly achieve remarkable outcomes with a proven implementation approach by the perioperative experts. Speed user adoption with mobile documentation and analytics that simplify OR management. Seamlessly connect to the enterprise, enabling providers to share information, prevent duplicate documentation, and analyze performance.
SIS is proud to be the only perioperative information management system vendor to participate in the HIMSS Intelligent Hospital Showcase. We will demonstrate our comprehensive perioperative software solution, showcasing interoperability between medical devices, hardware, and software.
TeleTracking Technologies, Inc.

Booth 6619
Contact: Amie Podolak, Director, Marketing
amie-podolak@teletracking.com
412.391.6395
TeleTracking, Booth #6619, will preview its Real-Time Capacity Management™ (RTCM) platform, which removes wasted time in hospitals much more efficiently by combining advanced patient flow, business intelligence, and real-time location technologies. The platform integrates the just-released Capacity Management Suite™ system version 3.0 and TeleTracking’s Real-Time Locating System, with the goal of progressively removing delays to the management and execution of critical business processes. Also, enter for a chance to win a Tag Heuer watch (valued at $2,500)!
TeraRecon

Booth 341
Stop by TeraRecon’s booth to learn all about the new iNtuition Enterprise Medical Viewer (iEMV), iNtuition SHARE and iNtuition Cloud. While there, enter a drawing to win a new iPad Mini!
iEMV provides a simple, intuitive, browser-based client which requires no download, no installation, and no plugin. A completely zero-footprint viewer, which supports a wide range of browsers dating back to IE7.
iNtuition SHARE makes possible CD-free transport and distribution of images between medical facilities and peers, or patients. When a healthcare facility deploys an iNtuition SHARE server, it is able to offer free access to network upload of images to institutions that need to send images into the facility, while removing the need to burn CDs for outgoing images.
iNtuition CLOUD is a self-contained solution which allows the full capability of iNtuition to be deployed via a web browser, either as an externally-hosted managed service, or as an in-house Private Cloud.
The McHenry Group

To schedule a meeting:
Contact: Lisa Gatto, Director of Client Development
lisag@mvp4u.biz
815.923.2500
Celebrating nearly 22 years in business, The McHenry Group (TMG) has become the most successful and most experienced International Executive Search Firm solely dedicated to serving the healthcare software vendor market. How successful? Since 1991, TMG has successfully placed over 2,000 candidates within the healthcare technology vendor industry.How experienced? Our Team of ten (10) search consultants has an average tenure with our firm that exceeds 11 years!
One of our Clients put it best: “Even though I was expecting great things from The McHenry Group, I was surprised by the extra effort TMG expended to understand our company, its corporate goals and our goals for our open position.I will definitely seek your help whenever our needs mesh with your services.”
TMG’s recruiting efforts focus on healthcare software vendors in the Provider and Payor (Payer) spaces. We identify superb talent for the C-level, VP Sales, regional sales, territory sales, channel marketing, client account executives, client services and implementation, sales support, consulting, marketing, product management, product development, clinical informatics, physician executives, clinical liaisons, nursing (RN) informatics and more! TMG is equipped to quickly tap into the hidden candidate market and recruit Top Talent that are not active on the market. Additionally, we can delve into our extensive proprietary database of candidates, coded by specific title, areas of expertise, etc.
TrustHCS

To schedule a meeting:
Contact: Jeff Johnston, Executive Director, Business Development, President
jeff.johnston@trusthcs.com
760.277.1190
TrustHCS provides consulting and services to address Clinical Documentation Improvement (CDI) programs, ICD-10 preparation, revenue cycle improvement, coding services, auditing and cancer registry. Visit www.trusthcs.com for more information!
T-System, Inc

Booth 2219, MU Experience booth 149/kiosk 42
Contact: Corinne Tso, Vice President, Marketing
ctso@tsystem.com
469.791.5540
This year at HIMSS, T-System will highlight solutions proven to help hospitals across the country achieve Meaningful Use and reduce avoidable readmissions through better patient transition management. In the T-System main exhibit booth #2219, leadership from Baptist Health of Kentucky and Cox Medical Center Branson in Missouri will discuss their experiences. In the HIMSS13 Meaningful Use Experience, a new special demonstration area for certified EHRs, T-System will demonstrate how an emergency department information system can help hospitals attest to Meaningful Use specifically highlighting the workflow for capturing patient history and documentation.
T-System, Inc. advances the practice of emergency medicine with solutions proven to solve clinical, financial, operational and regulatory challenges for hospitals and urgent care clinics. More than 40 percent of the nation’s emergency departments rely on T-System for gold-standard documentation, revenue cycle management, and performance-enhancing solutions.
Valence Health

Booth 772
Contact: Kevin Weinstein, Chief Marketing Officer
kweinstein@valencehealth.com
312.771.7883
If you’re an executive overseeing a Medicare ACO, interested in population health, or pursuing value-based reimbursement opportunities, Valence Health would like to help. Valence Health is among the nation’s leading companies in helping healthcare providers better manage their patient populations and accept financial responsibility for the quality of the care they provide. With unique data collection and analysis tools, Valence Health has emerged as a leader in population management, serving dozens of clients from small physician groups to the Cleveland Clinic.
At the same time, in-depth actuarial analysis combined with operational excellence allows Valence to not only advise but also provide ongoing services to provider organizations operating under various value-based reimbursement models. From risk-based contracting to accountable care organizations (ACOs) to administering provider-sponsored health plans, Valence has been helping providers appropriately accept and manage financial responsibility while improving clinical quality since 1996.
With headquarters in Chicago, and three other office locations, Valence Health’s 300 employees help support the health of more than 13 million patients nationwide.
Velocity Data Centers

To schedule a meeting:
Contact: Steve Jacobs, President
steve.jacobs@velocitydatacenters.com
734.323.3075
We enable healthcare IT organizations to achieve their strategic goals through our innovative solution to deliver cloud computing infrastructure. This innovative approach delivers incredible benefits at reduced cost. Allowing healthcare organizations to grow revenue, reduce operating costs and leverage current and future technology trends.
VersaSuite

Booth 3121
Contact: Tushar Jain, Regional Sales Manager
tj@versasuite.com
718.316.2254
VersaSuite is an innovative HIS and EHR solution designed to adapt to your hospital’s and clinic’s needs, no matter how complex. We offer a single database solution designed with identical and intuitive user interfaces for inpatient, outpatient and emergency department environments.
Versus Technology

Booth 3463
Contact: Stephanie Bertschy, Director of Marketing
info@versustech.com
231.946.5868
If you’re looking for awesome IT, we’ve got it at booth #3463. Our Real-time Locating System (RTLS) powers multiple time- and money-saving applications, from Asset Tracking to Patient Flow—and even, Hand Hygiene. We’re unveiling the first of its kind, RTLS-integrated dispenser, part of an overall hand hygiene safety program that will help your facility improve compliance by creating a culture of safety and accountability.
Added bonus — we’ll be conducting in-booth RTLS sessions, where you can learn directly from Versus clients, patient flow experts, and our own executives. Delve into implementation, integration and technology-related questions about patient flow, analytics, asset tracking, hand hygiene and more. Space is limited, so learn more and sign up now at http://versustech.com/himss13.
Don’t be led down the path of promises, get experience and proven results with Versus Advantages™ — visit with us at Booth #3463.
Virtelligence Consulting

Booth 3320
Contact: Akhtar Chaudhri, CEO
akhtar@virtelligence.com
952.548.6601
Virtelligence is a privately held premier Healthcare IT consulting firm that offers solution advisory and Healthcare IT consulting services to payors and providers organizations nationwide. Vi Through our unique consulting model providing an implementation-oriented partnership with clients, we offer consulting expertise across the full range of Healthcare IT vendor products and we deliver solutions specifically tailored to address the business needs of the healthcare IT industry.
- Project Management & Strategic Guidance
- Meaningful Use and ICD-10 Projects
- System Implementation & Upgrades
- Clinical Workflow & Process Optimization
- Revenue Cycle Improvement
- Business Intelligence & Data Analytics
- Health Information Exchange Adoption
PLEASE STOP BY OUR BOOTH #3320 TO WIN LATEST IPAD.
VitalWare, LLC.

Booth 6654
Contact: Kelly Jorgensen, VP Business Development
kellyjorgensen@vitalware.com
855.464.2310
Visit booth #6654 and enter to win a free iPad including a license to our new application, Doc Sherpa! A complementary ICD-10 financial risk assessment will also be available for those who sign up!
VitalWare leads the market in transforming healthcare intelligence into useful and actionable information so our clients can focus their time and resources on core business. VitalWare will be launching two new products to assist in provider ICD-10 implementation and beyond:
- DocSherpa, an innovative iPad app designed to guide physicians through documentiation requirements utilizing an easy to understand user interface. By helping physicians document missing concepts, DocSherpa alleviates physician productivity constraints today and well beyond the ICD-10 implementation.
- VitalSigns, the claims analytics solution and retrospective coding & auditing tool using TrueShift analytics over predictive modeling to identify actual ICD-10 risk.
Whether you ten-code your claims in VitalSigns, or opt to take advantage of our Quick Start offering to begin building your repository of claims, the TrueShift identified is critical in understanding true financial risk, documentation deficiency risk and payer contracting opportunities.
Vitera Healthcare Solutions

Booth 6113
Contact:
events@viterahealthcare.com
Vitera Healthcare Solutions provides end-to-end clinical and financial technology solutions so physicians and medical professionals can work with patients instead of paperwork. Serving more than 400,000 healthcare professionals including 80,000 physicians, Vitera Healthcare Solutions provides electronic health records and practice management systems, processes 33 million transactions and 1.8 million e-prescriptions monthly, and serves several specialties including primary care, OB/GYN, pediatrics, cardiology and orthopedics in all sized practices and Community Health Centers. Don’t miss seeing Vitera Healthcare up close and personal! Stop by our booth # 6113 to say "hello" and learn more about our industry leading healthcare software solutions.
VMWare

Booth 851
Contact: Tisa Murdock
tmurdock@vmware.com
831.818.6095
VMware, Inc. (NYSE: VMW), the global leader in virtualization and provider of vCloud for Healthcare; the healthcare industry’s first end-to-end cloud computing platform, is proud to sponsor HIStalk.
VMware vCloud for Healthcare is the first comprehensive framework and partner ecosystem supporting the entire health IT environment – from point of care to the most critical patient care systems. Helping to safely accelerate healthcare reform and the transition to truly connected care, this new innovative platform enables organizations to exchange information and deliver secure, agile, and reliable patient care products and services. A private cloud platform with hybrid cloud capability, VMware vCloud for Healthcare meets the growing needs of healthcare both today and tomorrow.
Vocera Communications, Inc.

Booth 6329, Intelligent Hospital Pavillian Booth 8711
Contact: Mauricio Cornejo, Sales Support
MCornejo@vocera.com
877.790.4190
Vocera provides mobile communication solutions focused on addressing critical communication challenges facing hospitals today. We help our customers improve patient safety and satisfaction, and increase hospital efficiency and productivity through our Voice Communication, Secure Messaging, and Care Transition solutions. Exclusively endorsed by the American Hospital Association, the Vocera solutions are installed in more than 800 hospitals and healthcare facilities worldwide.
Join Vocera in our booth for a Beignet Break on Wednesday morning.
Wellcentive, Inc.

To schedule a meeting:
Contact: Rich Walsh, Vice President of Corporate Strategy
rhwalsh@wellcentive.com
678.367.8187
Senior Management will be located at the Hilton Riverside in an Executive Suite conducting presentations and open discussions! We look forward to seeing you there!
Wellcentive delivers population health management solutions that enable quality improvement throughout the continuum of care. Wellcentive’s Advance™ platform transforms disparate data into actionable insights that facilitate coordinated preventive care and chronic disease management, physician alignment, clinical integration, and success with value-based reimbursement and incentive programs. Wellcentive empowers healthcare organizations to improve both clinical and financial outcomes.
Wellsoft Corporation

Booth 3158
Contact: Denise Helfand, VP, Sales & Marketing
dhelfand@wellsoft.com
800.597.9909
Consistently ranked #1 Emergency Department Information System (EDIS) by KLAS, (most recently awarded Best in KLAS 2012) Wellsoft EDIS offers an exceptional combination of experience, extensive workflow analysis and award winning customer support. Wellsoft EDIS is certified for Meaningful Use. Software features include Patient Tracking, Clinical Documentation, CPOE/Results, Charge Capture including Infusion Charge Capture, Risk Management and CCD Document exchange. Wellsoft is EDIS at its BEST!
Visit Wellsoft at Booth #3158 to have a brief demonstration and discuss how Wellsoft EDIS fully integrates with HIS and ancillary systems AND can help with your roadmap to Meaningful Use attestation.
Winthrop Resources

To schedule a meeting:
Contact: Dan Mandy, Director of Business of Development
dmandy@winthropresources.com
952.656.7687
Winthrop specializes in healthcare technology finance.The realities of today’s healthcare market demand a finance solution that can change with you as your strategic direction dictates.Please reach out to Winthrop to learn more on how we can partner with you to deliver a future of efficient care/systems and improved patient outcomes.
Wolters Kluwer Health

Booth 1740
Contact: Alyssa Downing, Marketing Coordinator
Alyssa.Downing@wolterskluwer.com
612.313.1500
A leader in point of care information, Wolters Kluwer Health Clinical Solutions provide best of breed offerings focused on improving the quality of care & driving clinical productivity. Hospitals, ASCs, physicians offices, payers, labs & retail pharmacies turn to us as their trusted partner for the content & tools they rely on every day. From Clinical Documentation, to Clinical Drug Information, to Clinical Informatics & Surveillance, to Clinical Decision Support, our products deliver meaningful solutions clinicians value. Facts & Comparisons, Lexicomp, Medi-Span, ProVation Medical, ProVation Order Sets, Sentri7, Health Language & UpToDate. Visit our booth for a chance to win one of five iPad minis.
ZirMed

Booth 4469
Contact: Kent Rowe, VP of Sales
sales@zirmed.com
877.494.1032
We’re ZirMed and we’re one of the nation’s leading providers of revenue management solutions for healthcare providers. Offering claims management, eligibility verification, electronic remittances, patient statements, payment processing, and business analytics, our solution suite simplifies the complexities of payments for providers and their patients. We resolve many problems with one simple solution – and one great relationship.





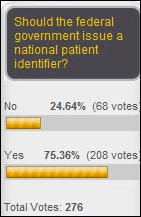


















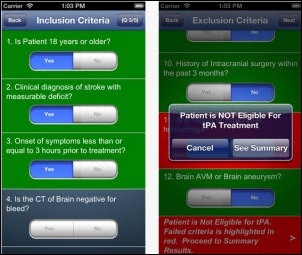
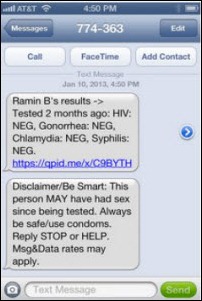
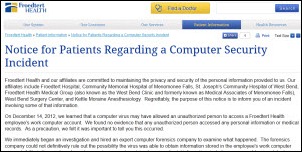







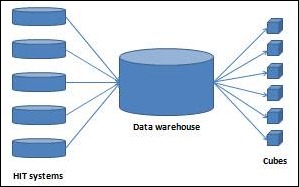
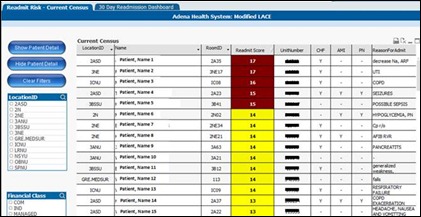












































































































Move your quotes to where they should be and it's no longer politics-in-the-blog, but instead a fact that's true at…