Frank Naeymi-Rad, PhD is chairman and CEO of Intelligent Medical Objects of Northbrook, IL.

Tell me about yourself and the company.
I received my computer science doctorate degree from Illinois Institute of Technology. My dissertation research work was in developing medical dictionaries that support electronic medical records, decision support, and information retrieval used at the point of care.
I got introduced to medical terminology when I was teaching classes to medical students, where I was directing academic, research, and administrative information services at the Chicago Medical School. These classes included use of computers for directed history and physical documentation, informatics workup, and concepts in medical artificial intelligence as senior electives.
During the senior elective setting, I wanted students to build knowledge for different decision support applications. The major task and challenge that we had developing knowledge for the decision support was standard terminology. Each system had its own dictionary. The systems we used were MEDAS, Dxplain, QMR, Knowledge Coupler, and Iliad. The medical students had to build knowledge for pattern recognition as well as rule-based decision support and application.
The knowledge created by students for a given diagnosis was then compared to knowledge within these expert systems for the same topic. The key learning objective was that everyone learned how the computers were used to make decisions and the results could be manipulated to reflect the new discoveries.
During that process, the most important aspect that came out was when we compared students’ patterns to other expert systems. It became clear that what was missing was standard medical terminology. This became the topic of my dissertation. It was really the concept of capturing and preserving the truth, what the source of truth about a given decision was and how the decision was made by the computer.
It was then necessary to reverse engineer the patterns back to the original form to explain why it led to the need to build a dictionary that students used to codify the rule. This allowed us to compare the pattern across multiple domains using the same foundation dictionaries. This led to my dissertation topic, which was a feature dictionary for clinical systems and electronic medical records.
The ultimate test was how the students’ knowledge would perform when interfaced to real patient data. Into the late 1980s and early 1990s, there were no coded electronic records. This led to the development of a history and physical documentation program on the Apple PowerBook for medical students. This program was expanded as a tool for second-year students as part of a supplement for the introduction to the clinical medicine class.
This program allowed students to develop comprehensive documentation for the history and physical exam. While the objective was to a develop a patient electronic record that could be used to test the student decision support pattern, instead it led to the creation of an electronic medical record which was used a the Cook County ER. IMO was created to help commercialize the product that was sold to Glaxo Wellcome, which at that time was called HealthMatic.
Later on, HealthMatic was sold to a company called A4 Sytems, and then A4 Systems sold its assets to Allscripts. The EMR that we developed at the medical school, with the help from many of the same IMO team developers working with me at the medical school, helped commercialize it. The current generation is called Allscripts Professional.
You can understand how the team who is working at IMO right now are key players in the industry. This is the same team from the medical school as well as the same team that developed the early clinical documentation for HealthMatic and medical content work for Glaxo Wellcome.
Describe how IMO’s product and the terminology works with EHRs.
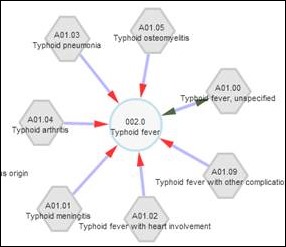
Our flagship product is interface terminology. Our primary objective is to capture and preserve the clinical intent and then map that clinical intent — the truth — to their corresponding regulatory requirement. Interface terminology manages and maps between clinicians’ terms and the required regulatory code terminology like ICD-10 and Meaningful Use codes as well as reference terminology like SNOMED CT.
The way we have succeeded is that we have removed the overhead of making a clinician to be a coder. They can say what they want to say. We manage the code and mapping and help our EHR partners to capture and preserve the truth.
Who is your most significant competitor?
The competitors that I see are people who do not really understand the challenge of terminology and the importance of preserving the clinical intent. Fortunately and unfortunately for us, I think the knowledge base within the marketplace is growing. We need a dynamic model to respond to these changes as soon as possible.
We are very happy that we are able to help our partners meet regulatory standards. Adaption of standards is a very daunting task for many of our vendor partners. There has been a lot of movement in our space because most of the new regulatory standards require several new coding subsets.
We expect large and innovative competitors coming into the terminology space. What they are missing is the understanding of the electronic medical record and how terminology should be used within the electronic medical record. Having the EHR knowledge expertise gives a true edge to IMO’s team as the market moves from fee-for-service to fee-for-performance.
There are many competitors within the terminology space. We have competitors who are managing the coding for reimbursement and now have to also do clinical. We have competitors who sell you tools in order for you to manage the complex mapping for the coding within the clinical setting.
Terminology management is hard and tedious work. We have a unique group of knowledge workers and physicians because they are good at it and love doing it. Adding to that our technology team, with the understanding of the electronic medical record and how terminology is used within the electronic medical record, creates a major barrier for others to match the quality of our service delivery.
What parts of HITECH have caused both vendors and providers to seek you out as a company?
It’s compliance to the Meaningful Use requirement and making sure that they are able to manage the changes associated with Meaningful Use requirements. When you look at our portfolio of clients, they initially used us to enhance clinical searching and finding codes for reimbursement. I believe Meaningful Use is creating a unique challenge for them because it is moving the market from fee-for-service to fee-for-performance and that aspect of care creates a unique attribute and need of understanding the use of terminology within the state of care. Our interface terminology service is to make sure that the truth about clinical data is stored as expressed by the clinical team.
For example, when you’re on the same term within the assessment, it may have a different ICD-9 code versus that same term in the history section. Being able to have a concept-based architecture that manages this complexity allows for correct mapping to ICD-9 as well as to ICD-10 complex billing post-coordination, but also maps to SNOMED CT and other required Meaningful Use terminology subsets.
We take that complexity out. We manage that complexity within our tool set and then we deliver those to our client base, allowing their clinical user community intent to be preserved so we can also code for care.
A recent study found that IMO’s interface terminology can identify population health issues when paired with EHR data. What are the implications of what that study found?
The early studies that I did historically looked at finding the clinical truth. You really want to make sure that what clinicians are saying is preserved in their words and that the data being collected is following guidance dictated by the clinical team. The data collection service needs to provide terms that reflect the clinician intent in its original form.
We as a company have been very fortunate to be trusted by and permitted to serve one important population of our society, and that’s the clinician. We believe clinicians are under massive pressure to do their job through primitive electronic documentation services that do not speak their language.
I worked at the medical school for 12 years and I observed students going through all of the different stages of medical training. I understand and appreciate the difficulties physicians have to go through in their medical training. The knowledge base learned as part of their training is their most important tool to make them master problem solvers. Capturing and preserving their clinical intent is always the best card we have in understanding exactly what is wrong with the patient and even when a physician is making a wrong assumption.
Our interface terminology allows the truth to be preserved and not distorted by coding optimization templates or services. Preserving the physician intent is responsible for the success of this study, identifying 99 percent plus patients correctly in this publication. By empowering the clinical team and using IMO interface terminology, we are going to have a near perfect understanding of our patients at risk.
What’s your perception of the state of readiness for ICD-10 transition and what impact this is going to have on providers?
The impact for our vendor partners is going to be nominal because we knew going from 14,000 ICD-9 codes to 90,000 ICD-10 codes will be a massive transformation for many EHR vendors. But for our clients, it’s different because we started distributing ICD-10 mapping last year and we have been working with them to deliver their point of service solution.
As part of our support for ICD-10 CM, PCS, and MU 2, we are expanding our terminology foundations by 3,000-plus concepts and as many as 30,000 interface terms per month. What that really means is that our clients are able to manage all these lexical variants long before the regulatory deadlines for ICD-10 and MU2.
ICD-10 is just a different mapping for you and you allow customers to create or maintain their own in addition to what you supply, correct?
Correct. We don’t allow them to manage their own mapping outside of our mapping because we really believe in this crowd-based or wiki-based model. It creates transparency that our clients have the correct standard mapping. Our mapping obviously grows and changes faster because of this transparent model and medical knowledge changes. We have developed sophisticated tools and workflow to manage all the mapping ourselves.
Normally when people go to IMO we move them to what we call a migration process to make sure that everybody standardizes their local dictionaries to the same datasets. If there is an error in our mapping or if there is an inconsistency, we can always correct it quickly in the next release. But if we allow local mapping, it really can violate some of the principles that we have. We don’t prevent them from having local variation and mapping. They can have their own lexicons if they want to, but we don’t take responsibility for those maps and will not distribute to other sites.
If they have like a certain phrase that they use locally, they can build it into the equivalent of a dictionary so that even if it’s not commonly used they can still understand?
They could still understand, but they should normally be asking to send it to us. If it matches our editorial policies, we distribute to everybody else. Everybody else would use that as well.
But I think it is important for them to be cognizant of the bigger picture because we really believe that this is the grand opportunity to really make standards like SNOMED and ICD-10 to truly work, because if we map correctly to them, at least these standard coding systems and these regulatory coding systems become more valuable for our future. Obviously they will be changing as well. If people start mapping their own local terms, there’s no way to be able to validate or review that and then challenge it.
That would be unusual, right?
That’s unfortunately not true. There is always going to be new concepts requested. We have term request workflow to incorporate new valid terms in our next release within six weeks and to have everything made available to our community. There are going to be some domains that most likely our clients would need to have their own local terminology, but terminology as it relates to clinicians’ decisions, like the problem list, the past medical history, assessment, and plan, which are foundations for clinical team decision making and requires billing codes that need to be codified correctly.
Has ICD-10 changed your business substantially so that people are seeking you out for a painless solution?
I don’t believe that ICD-10 alone is the issue. The reason our product has been sought out is EHR adoption and usability by clinicians. I really do believe that clinicians are commanders-in-chief when it comes down to fighting diseases and planning treatments. Clinicians are the key stakeholders as we transform from fee-for-service to fee-for-performance. They must be in control.
What our vendors do is use IMO as a source of truth for tracking clinician commands and orders, preserving the patient problem list and differential diagnosis using their dictation into the electronic medical record. ICD-10 is just a byproduct that the EHR vendors needed to comply to. You could say the usability is how the value of IMO is realized when complying with ICD-10, SNOMED CT, and within a few years ICD-11 are byproducts.
What research and development is the company working on?
We have been done with ICD-10 for quite a while. Our biggest research and development is invested in tools to manage our growth that we are facing right now. We are becoming the foundation technology innovation platform for many of our EHR partners. What that really means is that we have worked very, very hard to make sure to marry technology with terminology.
We have a cloud-based solution we call our portal service that allows the physicians to search the way they want to search. We can then rank order the search results in context of the domain that they’re searching for. This new technology allows us to do what we call just-in-time vocabulary releases. We have 60 releases a year total and for diagnostic and procedures 10 releases each. Using the portal eliminates many of the overheads associated with local dictionary normalization.
But these 60 releases a year historically without our technology would be impossible to adopt with import/export technologies. In most cases it takes maybe some times two or three months for people to deploy updates or in many cases people only deploy the regulatory requirements rather than updating on a monthly basis. By having this portal technology available, allowing the marriage of technology and terminology, we are able to make these datasets available at the point of service for our clients almost instantaneously after delivery of our service.
This has really increased our product usage. We have over 350,000 physician users and over 2,500 hospitals using our product. Many of our vendors are moving to our portal as their terminology innovation platform. One comment that we get from our clients is that they know when IMO is not there. That’s by far the biggest compliment that we could get.
What does the physician see differently if they’re using a system that uses IMO versus one that doesn’t?
They can find what they’re looking for and the description that they want to assign to the patient’s problem in the right lexical context and within the top three to five term list results.
Is that time-saving for them?
Absolutely. We are seeing up to three minutes for complex visits and as much as 30 seconds per common visit. The most valuable is a more granular problem list and orders in their clinical speak. We have not measured the IMO factor in follow-up time saving. We hope to work with our partners and perform independent research on the effects of having IMO in time and quality.
Where do you see the company going in the next five years?
Where we are going is to empower our vendor partners to deliver the best EHR solutions in the marketplace. We believe that our technology and removing this complexity associated with its managing terminology makes our partners stronger. They can do more innovations for clinician documentation. That is the most important thing to us.
We believe we want to participate in the success of the care delivery organizations in our country. I believe that as clinicians become empowered in the clinical setting and take over the responsibility of delivery of care using IMO-enabled EHRs, they and care delivery organizations will see a reward based on the quality of care they’re delivering. We would be a key part of this transformation for our vendor partners, their clients, and users.
As we allow our vendor partners to innovate, many of IMO’s portfolio terminology-enabled assets that we have been developing in the last 20 years will become more valuable at the front line and will allow our partners to build a positive distance between their offerings and others not using IMO. We hope to grow with our vendor partners to eventually make the US destination healthcare through new innovations in medical terminology-enabled technology. This is the way it should be.
Do you have any final thoughts?
Thank you for your time and opportunity to present IMO to your audience. We are honored with the finding of the independent study result showing that when using IMO interface terminology, nearly perfect agreement is achieved with greater than 99 percent in a peer-reviewed CDC publication. This article was truly energizing for me and the IMO team working in this space of dictionaries and terminology innovation to capture clinicians’ intent. It seems that finally after all these years we can actually see the fruit of our work, and that is really a good feeling.

































































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en