Part 1 of the interview is here.
Neal Patterson is chairman of the board, CEO, and co-founder of Cerner Corporation of Kansas City, MO.

Are EMRs the center of the universe, or would a better model be more open systems that support an ecosystem of components?
I think there needs to be much more openness. Because of the complexity of healthcare, nobody, no company, is ever going to do 100 percent of the needs. There’s just too much complexity to healthcare to think in terms that you’ll have a 100 percent.
I love seeing innovation done at the edge, whether that’s coming out of clients that have committed enough resources to do development or where we put out pockets of developers to work specifically at the client edge. There’s all kinds of needs for our systems, Cerner’s included, to be more open so that we can have an ecosystem developed around our systems.
I don’t think, though, that core chassis of the 80 to 90 percent of the requirements that are driving the clinical enterprise … I don’t think openness evolves that back to best of breed. I think those are the core capabilities of integration are going to win over in the center of the needs. The edges should be open. There’s too many things to work on to think of it all coming out of one top-down driven organization.
If you were starting a healthcare IT company today out there on the edge, what problem would you choose to solve and how would you go about creating a business from it?
I’ve thought about that recently, not that I’m out to start another one. Somebody was starting an accelerator in Kansas City and the question was, do we as a company want to be part of it? The short answer was, we’re supportive, blah blah blah, but we stepped back one step. In that process, I actually pondered that question.
Historically, there have been a lot of niches. All of us started in a niche somewhere as a company. I’m a big fan of innovation that gets done at the forest floor. The forest floor that I talk about is when you go to HIMSS, you see the big towers at the boat show, but there’s always a whole bunch of the smaller stuff. I love the forest floor because all trees in the forest started as a little sapling somewhere. The advantage of small is you can be highly focused. You’re all in. You’re putting in all your innovation skills.
But the reality is that in the past, a lot of people created business models and niches around all of the peculiarities of healthcare and how inefficient it has been in the past, particularly around the payment system. There’s always niches to go develop around on the delivery side. I think the inefficiencies in healthcare are slowly going away. There’s fewer targets to go start the companies at, although there’s still probably another 15 years .. find the spot in the billing system that you can help increase your revenues. I’d be real smart around NLP, around coding in this subspecialty. I think those ultimately go away.
I think the opportunities are less. I think the home, the integration of the devices… devices, I think, are still reasonably wide open because everything is now so smart. I would try to find some edge condition around the result of that condition where it’s probably outside the enterprise. That’s what I’d invest in.
When you look at that forest floor of those companies that are trying to get a foothold, what do rules do you apply to them to determine whether you think they’ll be successful or not?
Jim Macaleer of Shared Medical Systems happened to be a neighbor of my older brother. Or my brother was a neighbor of Jim, or they knew each other back in Pennsylvania. When we did our very first venture round in 1983, I asked my brother whether he wanted to be involved. Without asking me, he took our business plan over to Macaleer and showed it to him. And Macaleer basically goes, according to my brother, "I’ve seen so many of these and they’ve almost all failed." So I’m afraid that I might be becoming Jim. I hope not. [laughs]
I later got to know Jim a little bit and he was an outstanding man. I mean, he really was. But he had his beliefs. When he got to be a certain size, he looked back and didn’t create a lot of credence. I have a lot of respect for what people are doing. I don’t know that I’m smart enough to give you the formula which one will survive and which one won’t. It’s all hard. There’s a lot of serendipity to success, too. More serendipity typically than brilliance. Right time, right place. The art’s in the timing. It’s not so much in the idea.
Could someone today do what you did at Cerner in taking the company from an idea drawn at a picnic table to a huge, publicly traded company while retaining control after all those years?
The art’s in the timing. The window has to be there. There are these waves. As a small company, you don’t create the wave. You have to be able to see it, sense it, and then … I’ve never surfed, but it seems to fit my vivid description of what you have to do … you have to be there at the right time, at the right place. The wave has to be there, too. The wave’s got more energy than you ever can create. Somewhere you’ve got to create this leverage point of being able to get up and ride.
You can’t take the Cerner wave because everything is unique. It was point in time stuff. You can’t use our pattern. It’s the same skill set, though. You’ve got to see the wave and you’ve got to find those convergence points of where technologies and needs and industries match. Then you’re there. You’ve got the skills. You’ve got enough to make enough payrolls to get far enough down the road.
I love entrepreneurs. I love the entrepreneur spirit. Entrepreneurs love this country. I think those pilgrims that came over were entrepreneurs of sort. They were certainly avoiding something they didn’t like in the old countries, but they were mutants where they could handle risks that most people abhorred. The skill set was common. The patterns, though, are all individually or unique to the time.
It would be a very good time. There’s more change that will happen in healthcare in the next seven years as we finish this decade than has happened in the last 70 years. This thing has to change. Change is what creates opportunity. And my gosh, this intersection of healthcare and IT … just look at the innovation in IT over the last seven years and look at the change in healthcare over the last seven years and then just say, well, if there’s even similar trends of the past equals the future, there’s going to be huge fundamental opportunities over the next seven years.
It’s a great time to be where we are. We’ve made plenty of mistakes, but we fix mistakes. We learn from them. We also get better from it
How do you think private equity firms influence the industry?
It’s probably a little negative. My experience in that era is relatively dated. It just seems to me that there’s a lot of leashes that come with money nowadays. As an entrepreneur, the last thing you really want is a leash.
The hospital system market has boiled down to Cerner and Epic. Did Epic’s growth surprise you, and how do you see that competition shaping up over the next few years?
The first part was a surprise. They might have been a little bit surprising. They were very fortuitous in the way the market developed. Again, the art’s in the timing. Their strengths matched up very well with how decisions got made.
I think we have inherently greater strengths on a much broader basis. We don’t stay static. What you may view as a weakness today will be viewed as a strength tomorrow. That’s how we work. I’m pretty sure I was the first to use the word “duopoly” and there were people who cringed when I said it, but it’s relatively descriptive. Healthcare in IT is huge because it’s worldwide. I personally believe competition is the best thing ever invented. Competition drives, accelerates innovation, it creates value for our clients. If you don’t respond to competition, you’re eliminated. It deals with the survival of the strong.
We are strong and we will get stronger. In every era, we’ve had major competitors. We go back to the lab days. I cannot tell you what exactly happened to Sunquest. I didn’t track it all. I’m just finishing a note, what I call a Neal note, to our associates. I have the HBOC story in there. We usually do our town halls right after our health conference. The associates we could get, we’d get them all together and we had basically a town hall format with a question and answer period. We were using an outdoor stadium and it rained on our town hall so I had to call it off. I told the story that the last time I had to call a town hall off because of weather was back in 1998. I went on to talk about the head-to-head match with HBOC and how tough a competitor they were and how many people declared them the winner. We’re going to do fine.
Epic draws the contrast saying that they don’t do sales and marketing and the product just flies off the shelf on its own. What is your thought about the role of sales and marketing in something like selling healthcare systems?
Frankly, I think there’s a lot of things that have been stated by that company … I think sales and marketing are healthy parts of an economic enterprise. I don’t know if they’re trying to make that bad or evil.
This business ends up being a relationship business, because I don’t know of another relationship or healthcare delivery organization formed that’s more important to them than the relationship we end up with. You’ve got to start that relationship somewhere and people have to learn about you. I don’t know what you call that. I don’t believe any company that has grown a lot doesn’t have that.
How would you describe your management style?
I make sure I have a great team around me. I mean, a really great team. Then my objective is, in the perfect world, that the organization is so well designed that there’s nothing for me to do. Now I’ve never even gotten close to the perfect world. I say that somewhat jokingly in a sense. Goal One is to create a great team that can operate without you.
Then I do two things. I look at chunks of my time, usually about 100-day chunks, and I say, what do I need as the leader to get accomplished in that 100 days? Then I design everything about me to work on what comes at the top at the list for the next 100 days. That’s how I do my calendar stuff. The test is that the rest of the organization is working well.
I’m kind of a free safety. I touch the things that I think that need to move internally, that I go then drill down. Another style I have is that I get very deep. When I want to understand something internally, I’m not going through the chain of command. I’m going down to where the work is and I get pretty deep. I tend to be in the room when we’re defining the three-, five-, and 10-year views of what we’re going to accomplish, too.
Intermountain Healthcare had an agreement with GE Healthcare similar to the one Cerner just signed. That didn’t seem to produce anything much for either organization. How will the company work with Intermountain in developing something that’s both useful to them and that has market value for Cerner?
I think they learned a lot from their GE endeavor. Their intent wasn’t to go develop something unique. Their intent was to basically go to a marketplace and build a relationship around a company that can meet most of their needs today. The foundation of that relationship wasn’t to go build something, it was to deliver something.
The flipside of that is that this is a very innovative, creative organization and entrepreneurial organization. We’re going to go build the first real costing system this industry’s ever had, working with Brent James and his institute, around building an activity-based cost system for healthcare. There are some specific things we’re going to go innovate together with them. Their large body of work over the last couple of decades around process models will certainly be a source of content for us and our other clients.
They changed what they were trying to accomplish with the relationship significantly. They wanted to go to the current marketplace and buy the best solution for them that’s available in the marketplace today. That was how they made that decision. It’s a neat organization.
I assume it’s similar to the agreement or the arrangement that you have with UPMC with also a lot of innovation and entrepreneurship coming out of a non-profit group.
UPMC is a great client and great innovators. They are amazing as well. We have a good relationship with them, but we’re at different points in time between the two. I don’t try to compare the two.
When these agreements are struck, it’s always between large, prominent healthcare systems and vendors. Do you think that that’s the right kind of information or outcome that will be useful to the average 300-bed community hospital, or should somebody be forming a relationships with smaller places that are more prevalent in number if not in stature?
I’m extraordinarily pleased with the level of collaborations we are doing throughout the industry. It’s not all with the megas. The work we’re doing with Advocate, a large system, around population health is real cool. I mean, that’s the largest ACO in this country. They pioneered the whole concept of clinical integration, which is the backbone to how you manage the care side of a population health system. They have 500,000 lives where they’re risk for, defined risk of a population attributed to their health system and down to individual doctors in their health system.
The other side of it is we announced recently an institute at Children’s National Medical Center, which is really this notion of development at the edge. We’re using them around pediatric populations. We have an institute at the University of Missouri, which wouldn’t be considered a mega client, but it’s a three-year-old collaboration where we are focused on the adult population. Then we have an institute up in Canada, I think they recently rebranded their health system but it’s Island Health in Vancouver, that focuses on the elderly. If you think of those three institutes, those aren’t your megas that you referenced.
We love where we clearly create an alignment between us and another organization and there is a specific area of interest and they have an attitude that toward innovation and development inside their health system. We jump on that. We have a whole model around that. I’m just very pleased with the depth of that and how productive that’s all been. Intermountain fits into that broad category of defining strategic relationships.
What’s the long-term plan for Cerner and for you personally?
There is a new layer of information, a new information model and technologies and platform around it, that’s growing up above the EMR that’s fundamentally designed to manage the health in a population and to support enterprises that can get closer to the first dollar. If you compiled that fairly concise set of three or four items we covered, it gives you what I believe we’re going to have.
I think we can synchronize the activities of a complete system around health and care and synchronize it and be able to through different organizations deliver predictable, guaranteed levels of care. I call them SLAs, the same as what we do in our data centers. Here’s the performance that you can expect from that system. Here’s the measurements that are useful.
There’s a new middle that has to be created in healthcare. Healthcare is this inverted thing — it’s all delivered local. You can get on an airplane and fly someplace, you can change the ZIP code, but it’s delivered local. From the ZIP code up, there’s just a huge amount of opportunity in healthcare. It’s the largest sector of the US economy. It’s typically the largest sector of every economy in the world, the exceptions being India and China where the investments haven’t been yet made. The needs are very, very similar worldwide. I think Cerner’s got a huge future.
As regards to me personally, I said at the beginning of the decade that this is the first decade that I start as CEO that I don’t expect to end as CEO. That’s a function of age, not a function of desire or anything else. It’s just kind of a reality. There are things in nature you do not change. It’s also a statement of confidence of how strong a team I think we have at Cerner.
Any concluding thoughts?
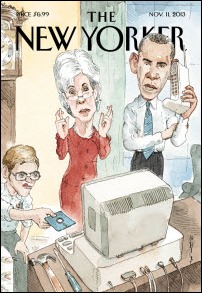
As we finish this decade, I think we’ll look back and say, this was the key decade that many people predicted over the last three decades, that there was going to be fundamental change and transformation in healthcare. I believe it happens inside this decade. My basis for that will be repeats of what I said previously, but I think the ability to finance an ever-growing expenditure of healthcare is decreasing rapidly. I think the need to transform it is here and I think the largest lever that you can have to change healthcare with IT.
This country and many other countries have invested significantly in IT, and we as providers of IT will collaborate with our clients around using that lever to fundamentally change the cost structures and the quality that’s produced. I also believe that there will be a fundamental change in business models, and providers will be much more integrated on vertically on how healthcare is financed, and they’ll be more accountable for the health of populations.
This is a significant industry and I’m extremely excited to be part of it. I feel very privileged.

























































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en