Top News
Healthcare Informatics owner Vendome Group acquires The Institute for Health Technology Transformation (IHT2), which offers executive health IT conferences, webinars, and research reports.
Reader Comments

From Quilmes Boy: “Re: Medseek. Underwent another round of layoffs this morning. My role was one of them.” Medseek CEO Peter Kuhn provided this response to our inquiries: “Over the past 12 months, Medseek has developed a significant offshore development operation, adding almost 150 personnel in India to accelerate product development and enable us to respond quickly to changing market dynamics and evolving customer requirements. In addition, weeks ago we funded the acquisition of Madison, WI-based Symphony Care, a leading population health and care management solution provider. Today, the company initiated a planned restructure to take full advantage of these recent investments. Medseek has retained all key personnel to deliver on customer commitments and deliver on near and long-term strategic goals.”
HIStalk Announcements and Requests
 Some recent goodies from HIStalk Practice include: McKesson may close its Seattle office. Physician EMR adoption in the US is up but still lags behind many countries. Texting while doctoring could negatively impact patient care and safety. CMS finalizes the 2014 Medicare Physician Fee Schedule, which includes a 24 percent pay cut if the SGR formula is not amended. Patent data from EHRs provide reliable measures of the process of care and the patient-centeredness of a primary care practice. A gastroenterologist finds pleasure in his move to a low-tech office. Lab ordering rates among primary care physicians decline with providers have a real-time display of cost information within their EMRs. Dr. Gregg takes a trip back to the future. Thanks for reading.
Some recent goodies from HIStalk Practice include: McKesson may close its Seattle office. Physician EMR adoption in the US is up but still lags behind many countries. Texting while doctoring could negatively impact patient care and safety. CMS finalizes the 2014 Medicare Physician Fee Schedule, which includes a 24 percent pay cut if the SGR formula is not amended. Patent data from EHRs provide reliable measures of the process of care and the patient-centeredness of a primary care practice. A gastroenterologist finds pleasure in his move to a low-tech office. Lab ordering rates among primary care physicians decline with providers have a real-time display of cost information within their EMRs. Dr. Gregg takes a trip back to the future. Thanks for reading.
On the Jobs Page: Program Manager – Healthcare Resellers.
Upcoming Webinars
December 17


”How to Drive ROI in Your Healthcare Improvement Projects,” presented by Bobbi Brown and Leslie Hough Falk, RN, MBA, PMP of Health Catalyst. Sponsored by Health Catalyst. Tuesday, December 17 at 1:00 Eastern. At a time when average hospital’s margins are stagnating, executives should be asking tough questions about the ROI of "indispensable" technologies. Will new technologies prove their worth or drive them further into the red? How do you measure and track ROI?
December 10



“Paperless Practices: Harnessing EHR Value by Improving Workflows with Electronic Data,” presented by Jay Ward of Kryptiq, Mike Kelly of DocuSign, and Sam Clark of Asheville Head, Neck, & Ear Surgeons, P.A. Sponsored by DocuSign. Thursday, December 10 at 1:00 Eastern. During this Webinar, panelists will discuss how industry and market trends have aligned to rationalize the adoption of e-signature in healthcare. They will also review primary, practical considerations such as legality, security, and mobility. Finally, panelists will highlight case studies and relevant examples of organizations that have successfully jumped onto the “path to paperless”.
December 11


“Audit Readiness: Three Simple Steps to Protect Patient Privacy,” presented by Mark Combs of WVU Healthcare System and Rob Rhodes of Iatric Systems. Sponsored by Iatric Systems. Wednesday, December 11 at 2:00 Eastern. Join us for this insightful Webinar to learn what you can do to keep your healthcare organization safe from unauthorized access to patient data.
December 12

“Looking Behind the Curtain: Value Based Care’s Impact on the Revenue Cycle ,” presented by Karen Marhefka, MHA, RHIA of Encore Health Resources. Sponsored by Encore Health Resources. Thursday, December 12 at 1:00 Eastern. This webinar provides a basic understanding of value-based health care, or accountable care, explain why value-based reimbursement may not impact the core revenue cycle components immediately, discuss the key focal points for change needed to maintain profitability in a value-based reimbursement model, review why organizations will be pressured to consolidate revenue cycle systems, list the type of tools that are being introduced or are changing with the move to value-based reimbursement and name the major changes that will be required from organizations to move to value-based care and reimbursement.
December 17

”The Power of Doctor Happiness: Why The Ideal Patient Experience Needs to Start with the Ideal Provider Experience,” presented by Lyle Berkowitz, MD, FACP, FHIMS (DrLyle). Sponsored by HIStalk. Thursday, December 17 at 2:00 Eastern. Hear from a "Doctor Happiness Guru" who describes how to think innovatively about using healthcare IT in ways which can automate and delegate care, resulting in time savings to doctors as well as improved quality and efficiency for patients.
Acquisitions, Funding, Business, and Stock

ClearDATA Networks closes a $14 million Series B funding round.
Accelera Innovations will pay $4.5 million in cash for Behavioral Health Care Associates, a billing and PM provider.
The College of American Pathologists (CAP) confirmed with Inga that it will shut down its CAP Consulting business over the next few months, concluding that, “The Board decided to exit the CAP Consulting business, our division located in our Lake Cook Road office that provides terminology and clinical information consulting services. CAP Consulting has made steady progress against its business objectives over the past several years; the services it provides are incredibly important and valuable. But with current fiscal constraints, the CAP is not able to continue to invest at the level needed to sustain and grow the business.” Employees were told on November 21. CAP hopes to place those affected in open positions, but also recognizes that the vendors it works with may have an interest in hiring them. CAP will continue to support existing products such as Electronic Cancer Checklists and Electronic Forms and Reporting Module.

Carl Icahn raises his stake in Nuance to nearly 19 percent of the company’s shares. NUAN shares rose around 6 percent in the past week.
Sales
St. Luke’s Hospital (TX) will add Craneware’s Pharmacy ChargeLink.
San Diego Orthopaedic Associates Medical Group (CA) selects SRS EHR.

Marin General Hospital (CA) engages MedAssets to support the optimization of clinical support resources through cost and operational management improvements.
Baptist Health South Florida will implement the Medseek Empower enterprise patient portal and integrate it with its existing Siemens and NextGen EMRs.

Banner Health selects Wolters Kluwer Health’s Health Language solutions to navigate the ICD-10 conversion process.
University Physicians of Brooklyn-Anesthesia (NY) will implement OpenTempo’s staff scheduling and case management solutions.
People

Experian names Jennifer Schulz (Visa) group president of its vertical markets group, which includes the company’s healthcare business. Its healthcare-related acquisitions include SearchAmerica (December 2008), Medical Present Value (June 2011), and Passport Health Communications (November 2013).

The National Association of Professional Women names Trudy Easton, RN, senior clinical consultant with McKesson, as its Professional Woman of the Year.
MedSynergies hires Doug Hansen (Accelion Health) as CFO.
Announcements and Implementations
Homecare and medical staffing company Interim HealthCare implements Procura Home Care Software across 47 locations.
Pediatric genetic testing laboratory Claritas Genomics will implement Cerner’s Millennium Helix solution, join Cerner’s Reference Lab Network, and collaborate with Cerner to develop a laboratory solution for molecular diagnostics. Cerner Capital has also invested in Claritas, closing the company’s Series A round.
Impact Advisors completes a feasibility analysis for Sutter Health (CA) that consider the possibility of Sutter sharing its EHR platform with a community hospital.
Healthix and the Brooklyn HIE (NY) complete their merger and will combine their separate technology platforms over the next year. The organization will retain the Healthix name.
PerfectServe introduces Clinical Event Push, which automatically informs physicians of important clinical events as they occur.
Coastal Healthcare Consulting announces Fusion, a solution to help healthcare organizations achieve peak performance from their EMR investment.

Mediware releases the MediLinks WTS workload solution for respiratory therapist staffing.
Government and Politics
ONC’s HIT Policy Committee votes to urge HHS to abandon a proposed requirement for providers to give patients reports showing who looked at their EHR data. Though patient advocacy groups support the requirement, opponents claim the option would be technically impractical and administratively burdensome.
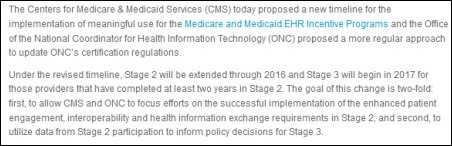
CMS reports that 85 percent of eligible hospitals have received a MU incentive payments through the end of October and 60 percent of Medicare EPs are meaningful users. Agency representatives also note that 89 percent of EHs have attested to Stage 1 MU using a primary vendor that had any 2014 edition product, while 70 percent of EPs used a primary vendor that had any 2014 edition product.

Rep. Scott Peters (D-CA) introduces the Health Savings Through Technology Act, which would create a commission to investigate how digital health technologies could help reduce healthcare costs and how they could be integrated into federal healthcare programs.
Innovation and Research
Researchers find that physicians who receive email notifications of lab results for tests pending at the time of patient discharge are significantly more likely to be aware of abnormal test results. Authors of the AHRQ-supported study suggest that widespread use of such automated systems could improve patient safety.
When it comes to HIE adoption, physicians are more influenced by other physicians with whom they interact and have common patients than by geographical proximity or other factors, according to a study published in the Journal of the American Medical Informatics Association,
Technology
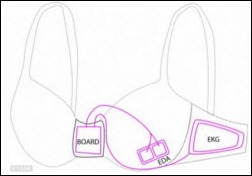
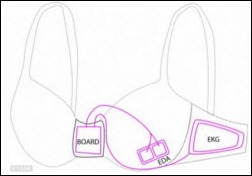
 Microsoft researchers develop a smart bra prototype embedded with sensors that flash smartphone warnings when the wearer’s mood suggests they might be about to eat too much. Enterprising hackers would be well advised to seek fast food chains willing to underwrite lingerie infiltration activities to redirect consumers’ dietary choices.
Microsoft researchers develop a smart bra prototype embedded with sensors that flash smartphone warnings when the wearer’s mood suggests they might be about to eat too much. Enterprising hackers would be well advised to seek fast food chains willing to underwrite lingerie infiltration activities to redirect consumers’ dietary choices.
A study of 19 healthcare systems using the Philips eICU ICU telemedicine system finds that mortality and length of stay were reduced, adding that patients were 26 percent more likely to survive their ICU stay and were discharged from the hospital 15 percent faster. The study also identified the most important criteria in delivering patient care and cost benefits from an tele-ICU program:

I spoke to principal author Craig M. Lilly, MD, professor of medicine, anesthesiology, and surgery at the University of Massachusetts Medical School and director of the eICU program at UMass Memorial Medical Center (MA), who told us, “All of the things we found made sense." The most important factors affecting patient outcome and cost were:
- Having a remote or local intensivist review the patient and care plan within an hour of ICU admission
- Reviewing the results of the program regularly
- Responding faster to patient alerts and alarms
- Following ICU best practices
- Conducting interdisciplinary rounds
- Running an effective ICU committee
Lilly clarified that the organizations studied were hospitals which had not outsourced their intensivists to a for-profit company.
I asked about previous vendor-supported studies that claimed benefits from tele-ICU programs that independent studies rarely validate. He emphasized that no commercial ties existed in this study. "Any meta-analysis that’s done going forward will definitely show improvement whether you include or whether you exclude the studies that were done by the commercial manufacturers."
Several health systems have shut down their tele-ICU programs due to cost and questionable benefit, most recently MaineHealth, and I asked Lilly about that. He said, "The MaineHealth outcome is really interesting. They had withdrawn it from about 35 community hospital intensive care beds and those folks actually signed up with another vendor. Even though MaineHealth wasn’t going to support it or subsidize it — and they were providing a pretty darned good subsidy, I can tell you, to have it in these community hospitals, which I think is when it became financially unviable and that was one of the reasons they wanted to cut it down — these other community hospitals absolutely saw the value in it for their patients and also for their financial outcomes.They signed up with another vendor and paid a lot more money to do so."
In summarizing his study, Lilly told me, "It didn’t matter whether you had in-house intensivists or didn’t and a lot of these places did. They still got better when they added this layer on. Even though they had somebody in house, that person couldn’t be everywhere they needed to be when they needed to be there. Because while they were dealing with the emergency in Bed 1, the patient in the the ICU three floors above them in Bed 7 was really getting sick and they didn’t know about it. This technology allowed hospitals with good intensivists and great bedside nursing to get the right expertise when they needed it, where it needed to be there because they were able to get on the alerts and alarms in less than three minutes and they couldn’t before."
Other
Allscripts India opens a new and expanded office in Vadodara to house 275 existing employees and to accommodate up to 400. Allscripts has 2,000 employees in India, up from 850 in 2010.
A psychiatrist warns peers about blanket authorizations that patients sign to get their insurance companies to pay for their care, with an example of a subsidiary of Quest Diagnostics requesting the complete paper file on one of his patients. He found that the company mines prescription data and sells it to life insurance companies to consider when deciding whether to issue policies. Psychiatric News, which ran the story, said, “Steven Daviss, MD, chair of the APA Committee on Electronic Health Records, told Psychiatric News that health information exchanges (HIEs), which connect different sources of patient health care data for the use of practitioners caring for patients, can also be an unexpected source of sensitive information. In Maryland, for example, the HIE contains information on hospital treatments, laboratory and radiology data, diagnoses, and medications. ‘This is valuable information that improves the continuity of care, but states have different policies regarding access to these data beyond treatment purposes,’ he said. ‘Most states have mechanisms that allow one to opt out of the HIE and to see who has accessed your information.’”

Boston Children’s Hospital (MA) reports a substantial drop in medical errors with the introduction of more standardized communication during patient handoffs, including a structured handoff tool within the EMR that self-populates standard patient information.
Vendors, beware: lawsuit-happy MMRGlobal is awarded its tenth healthcare IT patent entitled “Method and System for Providing Online Records,” which covers prescription and appointment reminders as well as e-prescribing.
A New York Times opinion piece by Pulitzer-winning writer Tina Rosenberg says hospital quality data is inconsistently reported and hard to understand. She says, “But at times it seems as if hospitals aren’t trying very hard. They like to report process measures on which they score well. But with 440,000 deaths from hospital error per year, their record is poor on key safety outcomes. This somewhat dampens their enthusiasm for public reporting. And what hospitals want matters a lot.”
A study finds that hospitals have a median of two employees assigned to manage population health, with mid-level managers being the most likely to be involved. It concludes that hospital population health approaches are inconsistent and poorly integrated.
In Europe, big drug companies are enlisting patient groups to lobby against legislation that would require them to publish all results of clinical trials, not just favorable ones, so that independent researchers could validate their conclusions. The two drug company trade associations want patient advocates to protest the release of such data by expressing concerns that it would be misinterpreted by non-experts. According to a trade group SVP, “EMA’s proposed policies on clinical trial information raise numerous concerns for patients. We believe it is important to engage with all stakeholders in the clinical trial ecosystem, including the patients who volunteer to participate in clinical trials, about the issue. If enacted, the proposals could risk patient privacy, lead to fewer clinical trials, and result in fewer new medicines to meet patient needs and improve health.”
Adoption of core medication MU elements reduces adverse drug event rates with cost savings that recoup 22 percent of IT costs, according to a study published in the American Journal of Managed Care.

An op-ed piece in New England Journal of Medicine reviews the OpenNotes initiative that calls for patients to have access to the notes made about them by their clinicians, citing previous studies showing that most patients read the notes and reported improved understanding, medication adherence, and feeling of control, with the vast majority of both patients and clinicians urging that the program continue. However, the article finds that while electronic medical records created the opportunity, they also complicate it:
Early adopters are learning that implementation means more than simply mailing notes or visit summaries or having patients log on to a portal. For starters, the knowledge that patients (and often their families) will have access to records affects the intent and sometimes the content of clinical documentation. Writing accurately about a suspicion of cancer, for instance, can be difficult for clinicians who don’t want to worry patients unnecessarily, and addressing character disorders or cognitive dysfunction in ways that are useful to patients, consulting providers, and others who use the records requires carefully considered words. These challenges are compounded by today’s electronic records, in which the story weaving together social, familial, cultural, and medical contributors to the patient’s health and illness often disappears, obscured by templates. A boon to billers, quality assessors, and researchers, such records can become formulaic and susceptible to data-entry errors. Moreover, they’re often filled with copied-and-pasted information that buries the essential narrative under voluminous repetitive text.
You may think you possess an unnatural ability to speak Siamese Thai when watching this video from Bumrungrad International Hospital in Thailand that describes its planned January go-live with inpatient nursing documentation using Medicomp’s Quippe.

Weird News Andy racked his brain to come up with “From Doobies to Boobies” as his working title for this article, which describes the potential for marijuana smoking to cause gynecomastia in men (i.e., moobs). WNA also likes the story of Ben Taub Hospital’s ED director (above), who is charged with breaking into the home of another female physician and using red lipstick to write “whore” and “homewrecker” on her bathroom mirror, presumably for reasons not involving emergent care.
Sponsor Updates
- Clinical insights platform vendor QPID is named a finalist for a publisher’s innovation award, as chosen by a panel of hospital CIOs and other executives.
- Greythorn conducts a market survey for HIT professionals to analyze compensation, benefits, job satisfaction, hiring trends, and industry participation. Greythorn will donate $1 to the Boys and Girls Clubs of Bellevue and Chicago for every submission.
- MedcomSoft partners with Liaison Healthcare to connect its Record EHR platform to more than 120 labs and imaging centers integrated within the Liaison EMR-Link Lab Hub.
- Aprima Medical integrates DMEhub into its EHR, allowing physicians to write orders for durable medical equipment directly from their Aprima EHR.
- First Databank begins publishing the National Average Drug Acquisition Cost pricing file from CMS.
- Aspen Advisors spotlights Baystate Health’s (MA) EHR optimization efforts following Aspen’s review and analysis of the organization’s EHR options.
- API Healthcare highlights the top 10 interview questions to ask nurses.
- The Indiana HIE details its work with Predixion Software to develop predictive analytics healthcare solutions at this week’s National Readmission Summit.
- Truven Health Analytics extends its contract to use Post-n-Track’s cloud-based web services platform for the exchange of eligibility data.
- AT&T launches EverThere, a wearable device that connects to a 24/7 call center if it detects that the wearer has fallen.
- Impact Advisors principal Laura Kreofsky discusses the sharing of patient data between hospitals.
- Quantros launches Quantros Member Center, a customer portal that provides immediate access to support cases, training videos, release notes, and user groups.
EPtalk by Dr. Jayne
From The Grey Goose: “Re: RSNA. Booth traffic felt like it was up. The temps were much warmer than last year (except they dip to the 20s later this week) so that probably helped improve the moods. All the big anchor exhibitors continue to improve their booths – more flash, more high tech, better organized space – so people wouldn’t get log-jammed in the middle. Lots of focus on moving data to HIPAA-compliant clouds and being able to access it securely on any device, anywhere. Folks not looking at that seem to be in the minority now which is a big shift from a year or two ago. People want to be more efficient to drive down costs in the land of Obamacare.” Thanks for sharing your experience. It’s great to have roving reporters fill us in on the meetings we’re not able to fit onto our busy dance cards.

From Converse All-Star: “Re: your Thanksgiving column. Mentioning readers sending photos of shoes brought to mind a pair of shoes that my lovely wife possesses. As you might expect, she saves them for special occasions and they also occupy a place of honor in our closet at home.” I’ll let our readers guess what state they represent. The coordinating scarf definitely puts these over the top! Is this the beginning of a 50-state themed challenge? Or better yet, perhaps we could convince The Walking Gallery’s Regina Holliday to branch out into shoes?
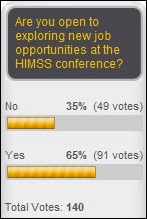
Dr. Jayne’s HIMSS Registration Update
More fun and games on the HIMSS website this week. After the HIMSS14 registration site couldn’t figure out how to charge my membership, I decided to go to the HIMSS main website to try to update my membership first so I wouldn’t have to do that step on the conference page. No luck – this critical error message was all I received. The site also refuses to recognize my MD and I can’t figure out how to update that part of my demographics (although it does refer to me as “Dr.” so it’s even more confusing).
I tried it again a couple of days later. I didn’t get the critical error, but when I tried to renew my membership, it adjusted the expiration date by a month since I’m renewing before mine expires, making it effectively only good for 11 months. At that point I was just glad my housing reservation was successful. I gave up for the night.
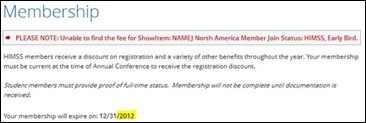
I decided to go back to the conference website and try it again that way. I am still receiving an alert that it can’t find the pricing for a membership renewal, but at least it has my expiration date in the wrong year. For those of you who are not familiar with the concept of positive pessimism, that’s an example: following up a negative statement with another negative statement to take the edge off the current problem. You’ll learn more about it if you are actually able to register for HIMSS and stay until Thursday to hear Erik Weihenmayer speak. He’s one of the best motivational speakers I’ve heard.

I tried to do it again without the membership renewal (thinking I’d try to do it on the main HIMSS site in January) and got this great new alert. Unfortunately it doesn’t tell me what to do with “please note” rather than “error” or “warning.” Perhaps we could use this as a testing scenario for next year’s Clinical Informatics board exam. Is anyone else having these issues? Or is it as I suspect and half the attendees are either vendors or media so they have a different registration process entirely and no one has complained yet?
I finally broke down and called because I didn’t want to miss the Early Bird discount. I was directed into a phone queue that didn’t have an option that applied to my scenario. Unfortunately the best advice the live agent could give was, “log out and log in again” and we all know how much end users love to hear that. I explained that I had been trying to register using multiple browsers on multiple different devices over many days, so I didn’t think logging out would help.
I asked if they could manually register me. She had to ask a supervisor. Ultimately the blame was placed on the data file that HIMSS sent with the incorrect expiration date, although they said they had no access to the file to try to verify the correct dates. After roughly half an hour of back and forth, they were able to shadow me in their system and bypass the problematic steps, so I suppose now I’m good to go. Inga and I are well into planning our social schedules, so please keep those event invitations coming.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.




























































































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en