This is the first CIO interview I’ve done with the intention of protecting the subject’s identity. This reader-suggested format allows an unusual level of candor. If you are a health system CIO and want to get your viewpoint in front of the industry risk free, let me know.
What are the good and bad parts about being a health system CIO?
The very best part of it is how lucky we are that we’ve selected a trade in information technology. I got into it out of college. it wasn’t at the dawn of IT, but it certainly was when it broke out and became ubiquitous within just about every industry and every business. It was the advent of the personal computer, the advent of file servers, and it just exploded at the right time. There’s no end in sight, so you pick the career trade where it’s constantly evolving. There’s all kinds of growth. If anyone as an IT professional is bored, that’s on them, because there’s so much that you can pick to expand your own horizons from a technical standpoint.
The second part of that is the fact that it’s at a crossroads between IT. You pick IT and how dynamic and ever-changing that is, and then then you pick healthcare as the industry vertical, and holy smokes. Look at all the change that’s happened and all the change that will continue to happen. IT’s in the middle of it.
It’s anywhere from the more somewhat mundane. Take ICD-10. Organizations can’t convert and be compliant with ICD10 without the IT component. Meaningfully Use, that’s mostly around IT enabling it. And the list goes on. It’s going to keep on going, especially now with payment reform and all the pressures that we all have to be able to deliver quality care for less money. IT’s going to be right in the thick of that, at the very least from measuring it to make sure that you’re hitting the mark and making improvements all the way up into making process improvements that IT will enable.
Do you think CIOs are fairly compensated?
You know, I think we are, because you can’t run the business without us, and there’s all kinds of pressure on keeping up and getting ahead, and especially when you have things like, “We’re going to replace about 70 percent of our systems and we want to do that in 24 months.” That’s a lot of heavy lifting, and even once you get that accomplished, you have a new need for support that you have to figure out. You’re doing this all the while that the business is still operating. Hospitals are still running, the clinics are still running. It is a balancing act that not everyone is cut out for.
If you look at other industries, healthcare leaders aren’t exactly paid the same as what they are in manufacturing and financial services. I cringe when I hear people say that CIOs or other healthcare leaders are overpaid. You don’t hear that about the other C-suite in other industries, general health. I don’t think we’re overpaid at all because it’s a very stressful job.
Even under best circumstances, it’s stressful, albeit the stress sometimes is self-imposed because we’re all very conscientious professionals and we know what we do is important to the organization. We know that mistakes can eventually harm people. It’s fairly rare, thank God, but it still can happen. Then you throw in the constant change. Then if you work in an organization that is, let’s say, less than ideal, then everyone is a critic. Everyone is a critic of IT. Everyone thinks they can do it better. And it’s a fairly risky position from a political standpoint.
So no, I don’t think we’re overpaid at all. Not at all.
What’s the most common reason that you’ve heard that CIOs get fired?
It’s typically around missed expectations. I’ve heard that a lot, especially in the last five years. Some CIOs are really big on marketing their programs and marketing themselves within their organization, sometimes even outside their organization. In doing so, they’re setting the expectations of what IT can do rather high. Sometimes it’s almost like a self-fulfilling prophecy where they’ve gone and worked hard at getting the word out about IT and perhaps they’ve made some promises that they’ve not been able to keep. There are expectations that are missed. That happens more often than what we hear about.
But then the other part that is, even if you’re not actively doing that and are trying to deliver at what’s reasonable and what you can commit to, there are still times where people get taken out because it’s perceived that they’ve not done enough. It’s a pretty slippery slope and it begins with the CEO of the organization. I’ve seen CEOs that are passive about IT. Sometimes the other members of the C-suite will not be passive about it, meaning that the CEO will be somewhat engaged, but they’re not going to be on you all the time. They spread their attention out fairly evenly across all the different divisions, so IT’s not singled out necessarily. And some of your colleagues then will take an interest in it.
CFOs are probably the most guilty of this, just doing their job and they’re trying to manage to the bottom line. It’s more of a financially-driven thing. They feel that there needs to be a check and balance in IT. Other times, I think CFOs believe that they’re smarter than the CIO and IT should be reporting to them because they can really control those costs. They do this sometimes without regard to understanding the value of what IT can deliver. They look at it as just the cost center that is just something else to be controlled. Those are bad situations.
I worked at a place where the organization’s financial standing was in very good shape. The CFO that we had there had retired, and this guy coming into it didn’t have a lot to do. He didn’t have to work very hard for the organization to look good from a financial standpoint. I am fairly confident through his boredom, he decided to stick his nose into other parts of the organization, including IT, and it really wreaked hell, challenging everything that we were doing. Finally we had to ask the CEO to intervene, which he did. That further pissed off the CFO, which I thought, well, too bad, dude, why don’t you stick to your knitting? Everyone’s a critic and sometimes people become active from outside of IT and try to manage and get into your business about it. I’ll never understand it.
It’s always interesting to me that a lot of the people who are IT critics approved the systems, but then resent IT having the maintenance expense in its budget.
Here’s an example of that. A hospital selected Epic while they were recruiting the CIO. They committed and got board approval for $80 million. The CIO gets on the ground, figures out where the restroom is and where the water cooler is, and is like, “Can I take a look at the budget for the Epic project just to make sure everything’s up to snuff?” The CIO asks the program director, "Is it your understanding that this budget in front of us is to cover everything?" They said yes. The CIO says, "We’re in trouble, then." Based on a crosswalk from similar Epic organizations, the hospital was about $32 million short.
The board approved the extra money, it gets implemented, and it’s done on time. Six or seven go-lives, inpatient and outpatient. Then the CFO says, “We’re not spending $18 million a year to support Epic.” The CIO says, “With all the stuff you guys missed going into it, let me guess that no one has had the conversation with you that to support Epic, it takes more. It takes more people, costs more money than whatever you’re coming out of.”
The CFO says he just assumed it would be less because the hospital was consolidating all these systems. That’s one of the dirty secrets of Epic. If you don’t talk to the right people and if you don’t ask the right questions, the support does cost you more money.
The CFO is fit to be tied. He wasn’t happy about going to Epic. He wasn’t happy about $80 million and he sure as heck wasn’t happy about $120 million. Then he’s looking at 18 or 19 million bucks a year on top of the 16 to 17 million a year in non-Epic IT. He’s just fit to be tied.
People are all yippy skippy about getting the new platforms. It’s going to be great and we’re going to spend this money. Then you get through it and the financial reality hits you. Then they’re not so crazy about it because now they’re spending more money in some cases on support, which then doesn’t allow you to do other initiatives. The spotlight remains on IT, and I think very unfairly.
If you’re a decent CIO, the big decisions as far as financial commitment to do major projects and everything that goes with that … if you’re doing a good job, the organization is deciding and committing the resources. You’re not. Good IT programs, for the most part, are working at the will of the organization and working on their priorities. The only thing that IT should be doing that most of your peers of the CIO are not going to care very much about it is the infrastructure stuff. You’re still getting the right approval, you’re still informing, you’re still making sure that, yeah, if we’re going to move from HP servers to Cisco servers and we’re going to spend $8 or $10 million over two or three years, here’s what we’re going to get for this.
It’s a very weird phenomenon. You don’t necessarily see that in any other part of the business.
What companies are doing a good and not so good job in your eyes?
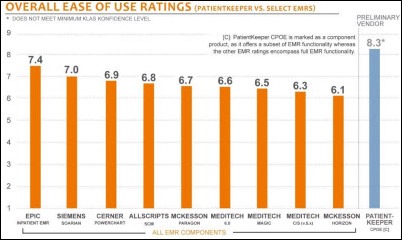
Epic does a good job as long as you know what you’re getting into and you ask the right questions. MedAssets does a good job in what they do. I’ve worked with them a few times and I think they’re a pretty upstanding organization.
We’ve had very good experience with Nordic Consulting. Very good people and they stand behind their folks and we’ve not had a bad person from there. Trying to think of bad experiences. I’ve been pretty lucky, because what I consider a bad experience is usually something that the organizations brought on themselves.
There have been people that have shown up for consulting work that we’ve had to turn around and after a week or two and they’ve not qualified, but that’s not the end of the world. That happens. There’s plenty of firms where I’ve seen that happen. maxIT, it’s happened with once or twice. I don’t hold it against them because sometimes it’s a misunderstanding of what we were looking for. Sometimes the hiring manager hasn’t been able to articulate the skills that they’re needing. It’s usually a mismatch. It’s not usually they’ve sent us a bum or they’ve sent us someone who’s just not competent. They’ve sent a competent person, but they just don’t have the skillsets that we thought we needed. I don’t get too worked up about that.
When you look at what vendors are hyping, what do you think’s the most overhyped stuff that’s out there that could be a landmine?
Certainly anything cloud and some of the risks that come with that.
I think one of the things that Microsoft is doing right now without telling too many stories that Microsoft will get pissed off about, but we had our enterprise agreement renewal come up. It was about $1.8 million net increase for the next three-year agreement and we weren’t buying anything in addition to the previous three-year agreement, so it was a net zero difference on stuff. We had some exposure if we acquired or merged or whatever, but that’s business as usual. We figure that in.
We knew he had this $1.8 million no matter if we didn’t add a single seat to the agreement. They came back and they said, if you go to Office 365, we’ll waive that $1.8 million. We get that in front of the CFO and he’s like, yeah, done, we’re going to do this. I’m like, whoa, whoa, whoa, whoa, wait.
I said, "Do you really understand what that means? All of our email, Exchange Server, Outlook, everything goes to Microsoft facilities. Everything goes to the cloud. We have PHI in our email and there’s nothing we can do about that. That’s always going to be there. We’re completely trusting Microsoft to have our back for any PHI disclosure when it comes to email, right? And if we have a breach and it goes public, you know that $1.8 million is going to look like chump change, right?"
He still did it. He went to the CEO and said, "We can save this money." I’m like, oh good Lord, OK. Microsoft held a gun to our head. Maybe they were gambling a little bit and they felt that our financial position was such that we’d take the bait. They were right. Even after my emphatic pleas in trying to get people to understand what a risk that was that we were assuming, they’re still doing it. I wasn’t happy about that at all, and I think that at least in the case of Microsoft, we’ll see more things like that. From a financial standpoint, it makes it hard to say no, but from a business standpoint, especially innate to healthcare, we have to be good stewards and be aware of what our risks are, especially with patient information. That it puts us potentially in a bad spot.
People overlook how much of the IT budget is made up of ongoing maintenance. It sounds good upfront, you spend your money, and then suddenly you’re locked into these forever contracts that have price escalators built in.
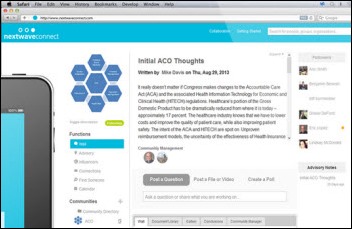
You ran a piece from Frank about big data and the hype around that. I thought it was a pretty good piece. In fact, I copied that and put it in a Word file for future reference.
I think that’s kind of a slippery slope right now, too. Even though there are plenty of organizations in healthcare that have not done a really good with decision support and with business intelligence and they do need to catch up a little bit and it will make them more effective, some organizations are going to go into this headfirst into the deep end. They’re going to be looking at companies and buying product from SAS, which is good stuff, but you have to have smart, very well-trained people in order to get the most out of it. The list goes on.
Some organizations have figured out that you don’t have to invest $5 million or $8 million or $10 million to have good analytics to be able to drive the business. It’s going to continue to heat up and we may see a bit more hype around big data. You’re going to see organizations overspending a bit.
Do you think hospitals even use the data that they already have? The problem often isn’t that they don’t have enough data, but are lacking the will or the capability to do something with it.
I think that’s correct. There’s so much good data available that is just dormant. But again, some of the tools are not the best.
For example, Epic took a big step last year at UGM when they announced this whole Cogito thing. They have the ability where you can do ETL data transfers into the Cogito platform from non-Epic systems. If you’re an enterprise customer, you get the platform for free, you just have to pay to stand the thing up. I know it’s a step in the right direction, but I think that until an organization has a platform where they can have data from any part of their system infrastructure, they’re going to be leaving a little bit on the table.
Of course you can get it done through much simpler tools like Access and, God forbid, Excel worksheets, but you’re always going to be prone to missing something or having a transcription issue when you take data from your key and from one place to another. I don’t believe you have to bet the farm on BI and spend $8 million just to get what you need. I think there’s some risk. I think there’s some hype there that we’re all going to have to deal with.
Would you as a CIO be comfortable in being the data and quality lead for the whole health system?
There are some CIOs that could do that. I’ve met plenty out there that have had more training than I’ve had in statistics and data management. That’s the luck of the draw. We’re all exposed to different things throughout our career and we all have different parts of what we do that are more interesting than others. I can see some CIOs doing that.
For me, I would take it on, but boy, I would make sure that I had a very strong individual or data jocks that really know and understood what the data was telling the organization and understood the relationships and understood what it meant to have high integrity in the data and the source of truth. There’s plenty of people who don’t understand the fundamentals and then you end up making decisions on bad data.
If you had a blank check both organizationally and financially to run IT any way you wanted, what would you do differently?
The first thing that is anything that has to do with IT would be under the IT umbrella. Too many organizations have allowed different parts and different departments too much leeway and have their own IT staffs and they end up sometimes with an uncoordinated mess. If there’s a bit or byte involved, it comes into central IT so it can have a much better coordinated effort.
I’d probably invest a little going back to the whole data thing. I think most organizations from the people standpoint don’t have enough of the right people. No matter what the decision support BI tool is, that’s almost not important if you have really good data people in the organization. I’d invest a bit more there. I think it’s becoming much more important given where we are and where we’re headed as an industry. The organizations that are going to be successful are those that understand their information and their data, act on it appropriately, and use it to make the improvements they need to make be it quality, cost reduction, or process improvement.
I guess the third thing is, I always am very transparent as far as what IT does, but I certainly would continue to say, “Look, Mr. CFO, Mr. Fill-in-the-Blank, just keep your nose out of our business and don’t try to run IT. Leave it to the professionals.”
How do you as a CIO feel about HIMSS and the HIMSS conference?
I have found that I don’t go to the sessions. I spend my time networking with people I know in business, especially vendor partners. That’s the one time of year where you can get caught up. It’s a pretty good setting. People are more open and honest at HIMSS. For whatever reason, it’s just a more relaxing environment than just having one-on-one meetings throughout the year.
I think it’s still relevant to the industry, especially for staff to go. There are good presentations. There’s good information to be had. Of course, there are some that are not so good, but that’s been ever since I’ve been going.
I think the exhibit all is helpful if, of course, if you’re in a buying mode where you can do one-stop-shop and compare products, but also learn about new products, which is pretty helpful. In New Orleans, I spent all my time in the exhibit hall and meeting with colleagues and with people that I know that are in different aspects of the industry. I didn’t go to a single session. I’ll still go, but I don’t go for the full event. I’ll go for three days.
Any final thoughts?
Those of us that work in the business, we’re all just very fortunate to have these dynamic times with our industry and the dynamic times as technology evolves and how we can figure out how to apply it to the work we do. Continuing to work on getting organizations to understand what the potential value is and how we can deliver it and strengthen how IT is being viewed versus just a cost center.



















































Merry Christmas and a Happy New Year to the HIStalk crowd. I wish you the joys of the season!