News 1/24/14
Top News
At ONC’s annual meeting on Thursday, HHS Secretary Kathleen Sebelius UK Secretary for Health Jeremy Hunt sign a collaboration agreement between the US and UK that calls for sharing quality indicators, exchanging data and interoperability ideas, maximizing healthcare IT usage, and encouraging health IT innovation.
Reader Comments
From Freedom Rock: “Re: Martin Health System, Stuart, FL. A friend who is there says their $80 million Epic system is down throughout three hospitals and many other facilities and physician offices. They’re calling in off-duty nurses and clerks to go back to paper.” I asked CIO Ed Collins, feeling guilty as I did so knowing as an IT person how annoying it is to field questions about downtime when you could be fixing it instead, but he was gracious to provide a response Thursday afternoon:
“Martin Health System had a hardware failure that has resulted in our network being down. The failure occurred the evening of Jan. 22 and we are continuing to work on rectifying the situation. Epic is among the systems being impacted by this hardware failure, however, it was not the genesis of the problem. We are continuing operations as scheduled, while strictly monitoring any potential patient safety concerns or issues that would require appropriate care determinations to be made. Our patient care teams are following downtime procedures and protocols to ensure patient safety and proper documentation is provided.”
From Macke: “Re: Dave Henriksen. The former SVP/GM at McKesson who left to become president of healthcare information solutions at Carestream Health in July 2013 has left Carestream.” Verified. A Carestream spokesperson says Henriksen has left the company for an unspecified opportunity.
HIStalk Announcements and Requests
![]() Some of this week’s highlights from HIStalk Practice include: EMRs helped improve the identification and follow-up of infants born infected with hepatitis C. Connecticut IPA Medical Professional Services selects athenahealth’s Population Health Management platform. Provider engagement and administrative issues present the biggest challenges to practices adopting and implementing EHRs. The biggest complaint patients have about their physician: waiting in their office. CMS seeks EP participation in the 2013 PQRS-Medicare EHR Incentive Pilot. Twelve HIT vendors discuss emerging technologies expected to have the biggest impact on physician practices over the next 12-18 months in the second of a three-part series. Dr. Gregg ponders if HIT has jumped the shark. Thanks for reading.
Some of this week’s highlights from HIStalk Practice include: EMRs helped improve the identification and follow-up of infants born infected with hepatitis C. Connecticut IPA Medical Professional Services selects athenahealth’s Population Health Management platform. Provider engagement and administrative issues present the biggest challenges to practices adopting and implementing EHRs. The biggest complaint patients have about their physician: waiting in their office. CMS seeks EP participation in the 2013 PQRS-Medicare EHR Incentive Pilot. Twelve HIT vendors discuss emerging technologies expected to have the biggest impact on physician practices over the next 12-18 months in the second of a three-part series. Dr. Gregg ponders if HIT has jumped the shark. Thanks for reading.
I like it when companies issues press releases announcing their HIStalk sponsorship, so thanks to Coastal Healthcare Consulting for doing just that.
On the Jobs Board: Principle Clinical Healthcare Consultant, Marketing Manager, Sales Engineer – Boston or Raleigh.
Upcoming Webinars
February 5 (Wednesday) 1:00 p.m. ET. Healthcare Transformation: What’s Good About US Healthcare? Sponsored by Health Catalyst. Presenter: John Haughom, MD, senior advisor, Health Catalyst. Dr. Haughom will provide a deeper look at the forces that have defined and shaped the current state of U.S. healthcare. Paradoxically, some of these same forces are also driving the inevitable need for change.
February 12 (Wednesday) 1:00 p.m. ET. Healthcare CO-OPs and Their Potential to Reduce Costs. Sponsored by Health Catalyst. Presenters: David Napoli, director of performance improvement and strategic analytics, Colorado HealthOP and Richard Schultz, VP of clinical care integration, Kentucky Health Cooperative. Consumer Operated and Oriented Plans (CO-OPs) were established by the Affordable Care Act as nonprofit health insurance companies designed to compete in the individual and small group markets. Their intended impact was to provide more insurance options for consumers to pay for healthcare.
Acquisitions, Funding, Business, and Stock
VMware will buy mobile technology management vendor AirWatch for $1.54 billion. VMware gains secure mobile device credibility to its story for enterprises, including hospitals, that are shifting from fat client desktops to virtualized and mobile devices.
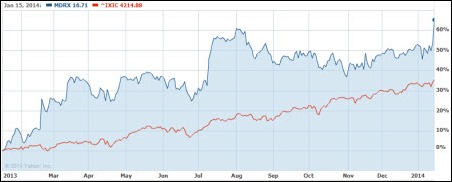
Quality Systems reports Q3 results: revenues down five percent; adjusted EPS of $0.11 vs. $0.29, missing estimates on both due to previously announced problems with its hospital software division. Shares rose 8.4 percent Thursday after the announcement before the market opened.
Microsoft announces Q2 results: revenue up 14 percent, EPS $0.78 vs. $0.76, beating estimates of both.
Proteus Digital Health, a developer of patient-care and self-health management technologies, closes $31.6 million in debt financing expansion. The company had previously raised around $160 million in funding. Proteus sells miniature medication tracking sensors (smart pills) that are activated by gastric contents, sending the information to skin patches that then forward the information via mobile device to a central service and allowing clinicians and family members to track oral medication intake.
Telehealth services and software provider MDLive raises $23.6 million. It offers around-the-clock consumer access to doctors. An individual plan costs $15 per month and includes one-day physician response to emails; phone or video visits cost $20. The company’s previously announced partnerships include Cigna and Sentara Healthcare (VA). One of its financial backers is former Apple CEO John Sculley, best known for firing Steve Jobs from Apple.
Sales
Parkview Health (IN/OH) will implement business analytics and denials management solutions from Streamline Health.
The District of Columbia Primary Care Association joins The Guideline Advantage quality improvement program, which uses population health management tools from Forward Health Group.
OSF Healthcare (IL) chooses Strata Decision Technology’s StrataJazz for budget and management reporting.
People
EDCO Health Information Solutions promotes Lynne Jones to president.
The Pennsylvania eHealth Partnership Authority HIE names the state’s HIT coordinator Alexandra Goss executive director.
HIMSS names Emanuel Furst (Improvement Technologies) the recipient of the 2013 ACCE-HIMSS Excellence in Clinical Engineering and Information Technology Synergies Award.
Announcements and Implementations
Philips Healthcare launches a Healthcare Informatics Solutions and Services business group to be led by Jeroen Tas, who previously served as CIO for Philips. It will offer hospitals clinical programs, analytics, and cloud-based platforms. The company also reorganized its North America Healthcare sales organization.
Mississippi Gov. Phil Bryant announces the launch of the Mississippi Diabetes Telehealth Initiative to improve disease management and health outcomes for diabetic patients. The program, which is a joint effort between the University of Mississippi Medical Center, GE Health, North Sunflower Medical Center, and C Spire, will use telehealth technology to connect UMC providers with diabetic patients in the Mississippi Delta.
Santa Clara Valley Medical Center (CA) goes live with RTLS asset management from Intelligent InSites.
Government and Politics
In his annual budget address, New York Gov. Andre Cuomo proposes a $95 million plan to digitize patient records using $65 million in state funds and $30 million from the federal government’s Medicaid program.
New National Coordinator Karen DeSalvo kicked off ONC’s annual meeting Thursday morning, mostly providing some background about herself and talking yet again about Hurricane Katrina like it was yesterday instead of eight years ago. HIMSS marketed the heck out of that disaster as a call to arm for electronic medical records (as sold by the vendors who provide most of its income, and when that didn’t help sales much, along came HITECH) and now KD has ridden it into the National Coordinator chair as her primary credential even though I haven’t seen any proven Louisiana outcomes that resulted. Her EHR experience isn’t clear, but she has a great public health background. I liked that she characterizes HITECH money as the involuntary taxpayer gift that it was, referring to it as “major investments by the American people.” She seems nice enough and her speech was friendly if not particularly powerful, although her uptalking made her sound less authoritative and is sure to drive mellifluous members of Congress who are used to polished oratory crazy. Nitpicking aside, I like her so far.
In England, Secretary of State for Health Jeremy Hunt urges hospitals to treat patients like people and for clinicians to work together as teams, suggesting that British doctors to behave like US hospitalists in taking responsibility for the patient’s entire stay from plan to handoff, including putting their names up on the wall of the patient’s room as being responsible. He also urges adoption of information-sharing technology, studying whether medical specialties are too specialized, and reducing patient transfers. I don’t know much about him or his politics, but I like him.
Technology
A Microsoft research project uses Kinect to help stroke victims recover.
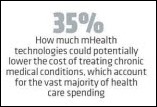
An irrationally exuberant and painfully breezy INC Magazine article declares mHealth to be “the trillion dollar cure” and “the miracle cure for the rising cost of health care in America” in which “smart startups are already cashing in” and that mHealth is “up for grabs, providing an extraordinary opportunity for medically minded entrepreneurs.” It quotes HIStalk Connect’s Travis Good (“a physician and influential blogger on health care technology”) and Palomar Health Chief Innovation Officer Orlando Portale, both of whom contributed just about the only thoughtful content amidst the hype. Like mHealth itself, the article is all over the place with a hodgepodge of apps ranging from weight loss to vital signs monitoring. It isn’t convincing in the slightest that most of them are either effective or destined for financial success, much less the cure for healthcare’s quality and cost problems, but business magazines like to make everything sound like a sure thing.
Speaking of mHealth, you know it has jumped the shark when former basketball player Shaquille O’Neal gets involved. Shaq says he’s working with Qualcomm on wireless and health technologies (I hope that won’t interfere with the making of Kazaam 2 or the next “Shaq Fu” album). Cynicism aside, Shaq actually has meaningful comments, not surprising since he’s a smart guy (he earned an Ed.D doctoral degree in 2012):
I have been using a FitBit, a connected activity monitor, to manage my fitness levels and am finding motivation in the real-time data I can collect on my movement—or lack thereof! Not only can mobile health technologies be engaging, social and easy-to incorporate into your everyday lifestyle, but using them for health monitoring will actually save between $1.96 billion and $5.83 billion in health-care costs worldwide by 2014. The latest technologies can’t solve all of our problems, though. Throughout my career I have found that when individuals come together for a common goal, whether it’s to win an NBA championship or reduce the number of people with chronic disease globally, greater results are achieved. We are on the verge of a new wave of breakthroughs in medical and wireless technologies, legislation and more, but unless we all come together to collaborate across public and private sectors and across educational systems and research institutions we will not see significant change and improvement.That’s why I am joining forces with the World Economic Forum, who are encouraging a global shift towards healthy living and supporting healthy, active lifestyles at individual, community and societal levels.
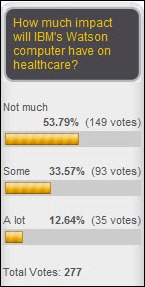
A Wall Street Journal report says IBM’s Curam eligibility software is responsible for problems with health insurance exchanges in Maryland and Minnesota.
Other
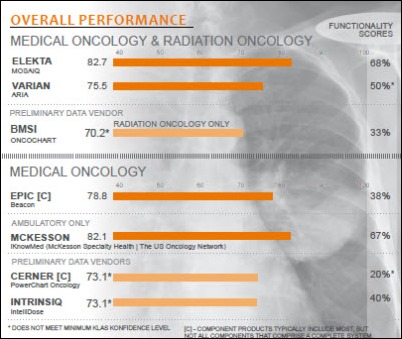
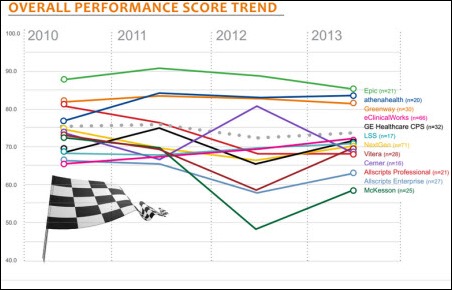
Cerner and Epic are making inroads in the medical oncology market, but product immaturity is leaving providers with a lack of functionality, according to a KLAS report. Radiation oncology is still a best-of-breed market with Elekta and Varian as the main competitors.
A HIMSS heads up: I didn’t realize that the Peabody Hotel in Orlando, across from the street from the convention center and the favored gathering place for well-heeled HIMSS attendees (meaning I’ve never stayed there, although we did hold the first HIStalkapalooza there in 2008), was sold in October for $717 million. It’s now the Hyatt Regency Orlando and is being marketed to mouse ears-wearing tourists. The famous ducks are gone, and given the prohibitive expense of shipping them back to the only surviving Peabody in Memphis, they may well have ended up as a l’orange.
A study finds that the use of EHRs improves the follow-up in identifying and treating babies born to mothers with hepatitis C. Identification of at-risk patients increased from 53 percent to 71 percent, while appropriate follow-up jumped from 8 percent to 50 percent.
Healthcare Growth Partners releases its 2013 Year-End Review report, which is as insightful, rich in detail, and downright eloquent about healthcare in general as it is healthcare IT investments. I would say it’s a must-read for anyone interested in the business side of healthcare delivery. An excerpt:
HGP remains very bullish on the health IT sector. Creating an environment of connected networks and transparency is core to addressing the structural flaws of the U.S. healthcare system, and IT is critical to enable the reform initiatives underway and any reform initiatives that may follow. The need is high, the runway is long, and the consequences are significant – as long as we get out of the way of ourselves, health IT stands to completely redefine not only the delivery of healthcare but also the management and sustainability of health.
![]() The dearth of HIT fashion-related news is finally over, thanks to B-Shoe, a start-up company that is testing a walking shoe that helps prevent falls. Designed for seniors or the physically challenged, the shoe incorporates pressure sensors and an algorithm that detects imbalance, plus a motion device that rolls the shoe slightly until the wearer regains his balance. Perhaps there will be a stiletto version by the time I’m in need.
The dearth of HIT fashion-related news is finally over, thanks to B-Shoe, a start-up company that is testing a walking shoe that helps prevent falls. Designed for seniors or the physically challenged, the shoe incorporates pressure sensors and an algorithm that detects imbalance, plus a motion device that rolls the shoe slightly until the wearer regains his balance. Perhaps there will be a stiletto version by the time I’m in need.
Weird News Andy makes a Roman numeral pun in calling this story “The 4th Doctor.” A company called IV Doctor makes house calls in New York to deliver a $200 hangover-curing IV solution, even providing a sales video. Those who attended the HIMSS conference in Las Vegas will recall my mentioning a similar service in that city.
WNA also turned up this story. A Nashville opera singer says a nurse-midwife’s episiotomy incision ended her mezzo-soprano career when it caused her to experience incontinence and excessive flatulence. She’s suing the federal government for $2.5 million since the treatment was provided by the Army, in which her husband was serving at the time.
Sponsor Updates
- Solstices Medical will use Infor Cloverleaf to integrate its DOCK-to-DOC platform with clinical, financial, and supply chain systems, including Infor Lawson Enterprise Financial Management and Chain Management for Healthcare.
- Vonlay adds 4,000 square feet in office space to its existing Madison, WI headquarters.
- CCHIT awards Iatric Systems Meaningful Use Manager ONC HIT 2014 certification for all 29 clinical quality measures.
- Kareo integrates its PM application with the Nexus EHR.
- Connance CEO and Co-Founder Steve Levin and Gwinnet Hospital System (GA) VP Cathy Dougherty author an HFM Magazine article, “A New Imperative for Patient Relationship Management.”
EPtalk by Dr. Jayne
A recent post on the Harvard Business Review blog discusses research indicating that smartphone use after 9 p.m. can make workers less productive the following day. Their work concludes that phone use causes sleep disturbances that impact work performance. Their two studies will be published later this year and I’m looking forward to seeing the details.
In the first study, they used a survey approach where each participant’s survey response data was analyzed individually over a two-week period. It had a relatively low number of participants (fewer than 100) but showed that increased phone use impacted sleep, creating work issues the next day. The second study had twice the number of participants with more diverse occupations. In addition to daily surveys, they measured use of phones, laptops, tablets, and televisions. The data indicated that smartphones had a greater impact than other devices.
As a physician, I enjoy being able to remotely access my patients’ charts, handle refill requests, process lab results, and take phone messages without being tethered to the office or to a PC. For me, however, using my phone to handle these tasks is a choice. Since my physician income is based on an “eat what you kill” model, I understand the value of my time and can make an informed decision to work outside the office or not.
Our ambulatory EHR has a great mobile product. Logging in and accessing a patient chart takes just a couple of seconds. This has made cross-covering after-hours call for colleagues much easier. I provide better care because I know more about the patients. I don’t have study data, but it would seem to be safer (not to mention more convenient) for the patient if I can address the issue based on the information in the chart rather than sending patients to urgent care. It also makes documenting those phone calls a snap.
Putting on my CMIO hat, however, I worry about the prevalence of working outside the office. Despite various office policies and customs encouraging staff to stay off email after hours, we’re having increasing challenges with staffers who continue to work long after the work day is over. Many of our employees are able to use flex time to accommodate family issues and expect to see some after-hours access in that circumstance. We’ve had some significant weather events with multiple school cancellations this winter, so quite a few parents have been working at home.
Barring flex time arrangements, however, I don’t expect to see people online at 8 or 9 at night unless it’s a scheduled maintenance event, and in that case, it would be happening after 11 p.m. Why is this behavior growing, then? Our health system has been through a couple of rounds of downsizing in the last couple of years and I wonder what impact that has had on people working after hours. Are employees trying to work longer and harder to distinguish themselves from their teammates in the event of another reduction in force? Are they young motivated analysts trying to get ahead? Are they just workaholics? I’d be interested to hear if readers in the trenches are seeing the same trends and what they’re doing to address them.
I beat Weird News Andy to the punch on this one. A Wisconsin medical examiner agrees to a plea deal after being accused of stealing body parts. According to the Wausau Daily Herald, she is accused of taking a piece of cadaver spine and human tissue “to train her dog.” Next time I’d suggest a Milk Bone or possibly a package of Snausages.
Earlier this week in Curbside Consult, I mentioned that I’m going to need roller skates to maneuver through everything we need to accomplish in 2014. Thanks to @SmyrnaGirl who found me the perfect pair. I bet Inga will be jealous.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.













































































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en