Top News
Apple updates its privacy policy to prohibit companies whose apps connect to its HealthKit platform from selling user data to marketing firms. The change comes just ahead of the expected announcement of new health-related iOS 8 capabilities, including Apple’s Health app. Deborah Peel, MD of Patient Privacy Rights reacted to the announcement by saying, “If Apple is really doing this, if they’re really saying to developers that you can only use the data for the specific purpose that app provides the user and that they can not share the data with anyone else without informed consent, that is the victory of victories. That’s what we’re seeking from all of the 100,000 of the companies that are now selling health data.”
Reader Comments

From Aruba Layoffs: “Re: Aruba Networks. Many talented people let go as healthcare technology spending is way down.” Wireless networking vendor Aruba isn’t healthcare specific. Both its revenue and earnings announced this week beat expectations, revenue is growing at 30 percent annually, and share price matches the Nasdaq at 25 percent growth in the past year. The company is, however, laying off 65 employees and moving 75 jobs to Oregon, India, and Ireland, but it sounds like that’s related to shifting resources to less-expensive locations rather than because of financial problems.

From Stephanie Reel: “Re: Star-Spangled Spectacular. I wonder if your readers would be interested in something that has everything to do with our nation, but nothing to do with our industry?” Baltimore celebrates the 200th anniversary of the National Anthem — written as Francis Scott Key observed the British bombardment of Baltimore’s Fort McHenry — with a week-long celebration September 10-16. It features visiting ships, a Blue Angels air show, a concert (Kristin Chenoweth, Melissa Etheridge, Denyce Graves-Montgomery, Kenny Rogers, Train, and the Baltimore Symphony Orchestra), festival villages, and of course fireworks. Stephanie is CIO for Johns Hopkins University and Hopkins Medicine – both campuses are worth a tour if you visit Baltimore for the celebration. You can bring the kids and take short side trips from the Inner Harbor to DC and Lancaster, PA along with seeing the Orioles play the Yankees that week.
From Jimmy John: “Re: HIPPA. I thought you would enjoy this magazine’s misspelling.” At least they were inconsistent from one line to the next amidst the click-baiting headlines – 50 percent right is better than none. They’re owned by HIMSS (or is that HIMMS?), as is the publication devoting 12 lazy paragraphs to a wandering, not-too-interesting story with the breathy “Generalissimo Francisco Franco is still dead tonight” style headline: “New HIPAA breach details remain vague.” The “new” breach occurred in June and details are “vague” because the reporter just cobbled together the story and quotes from wire reports.
HIStalk Announcements and Requests

School has started, so I sponsored some new DonorsChoose projects involving Teach for America teachers, doubling the impact of HIStalk readers since the Bill & Melinda Gates Foundation matched our contributions to fully fund them all. Teachers of DonorsChoose projects provide photos and updates, so I’ll have more later. What we as readers did:
- Purchased headphones and whiteboards for Grades 3-5 of a highest-poverty school whose teacher is urging her students to take ownership of their education, accept leadership roles, and share knowledge in groups that include peer tutoring.
- Bought 50 library books for a high-minority, high-poverty North Carolina charter school that has 100 percent college acceptance of its seniors.
- Provided a listening center for a highest-poverty school in southern Kentucky, whose energetic English teacher is struggling with ninth graders who haven’t read a book in years, some of whom have learning limitations.
- Bought six bilingual picture dictionaries for a middle school class of a highest-poverty school in New Orleans, whose large population of new students from Central America are working hard to learn English.
Meanwhile, I heard today from the teacher of a high school engineering class for which we bought a 3-D printer. He says he has had to redesign his lesson plans and projects for the better, the number of students in his classes has doubled, and he makes them think about, “How would you model that in the Replicator? What medium should we use?” He taught students the importance of scale and precision by having them create an iPhone case. He says, “I am overwhelmed with requests from the students about what is in the printing queue.”
This week on HIStalk Practice: Dr. Gregg shares a humorous take on voice recognition and “otto collect.” McGree Medical goes live on Epic’s Community Care EHR. HealthSpot prepares to install 100 telemedicine kiosks. Walgreens implements Greenway’s EHR in over 8,200 pharmacies. South Florida Medicine Director of PM Alyson Tiedeman shares her thoughts on managing IT across a large medical group. CarePoint Health System goes with eClinicalWorks for its medical practices. Results are in from the annual HIStalk Practice Reader’s Survey. Thanks for reading.
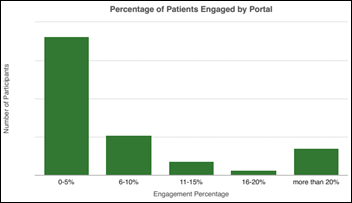
This week on HIStalk Connect: Dr. Travis discusses health IT IPOs and speculates who the next batch of likely contenders might be. Peer60 analyzes the patient portal market and the varying levels of success health systems are having with each vendor’s offering. Skullcandy partners with USC to host a digital health innovation contest focused on encouraging development efforts at the cross section of health IT and music.
Webinars
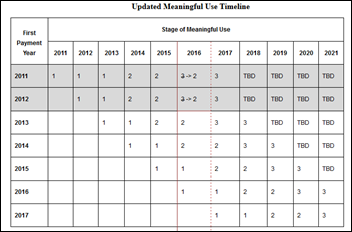
September 4 (Thursday) 2:00 p.m. ET. MU2 Veterans Speak Out: Implementing Direct Secure Messaging for Success. Presented by DataMotion. Moderator: Mr. HIStalk. Panelists: Darby Buroker, executive director of health information exchange, Steward Health Care; Anne Lara, EdD, RN, CIO, Union Hospital of Cecil County, MD; Andy Nieto, health IT strategist, DataMotion; Mat Osmanski, senior application analyst, Steward Health Care; Bill Winn, PhD, Meaningful Use service line executive, Navin, Haffty & Associates. Panelists will discuss the strategy and tactics of meeting the transitions of care requirements for MU2, including assembling the team, implementing Direct Secure Messaging, getting providers on board, and reporting results.
September 11 (Thursday) 1:00 p.m.ET. Electronic Health Record Divorce Rates on the Rise — The Four Factors that Predict Long-term Success. Presented by The Breakaway Group, A Xerox Company. Presenters: Heather Haugen, PhD, CEO and managing director, The Breakaway Group, A Xerox Company; Bill Rieger, CIO, Flagler Hospital, St. Augustine, FL. Many users are considering divorcing their EHR as dissatisfaction increases. Many are spending 90 percent of their time and resources on the wedding (the go-live) instead of the long-term commitment to new workflows, communication, education, and care outcomes (the marriage). Hear more about the findings of research published in “Beyond Implementation: A Prescription for Lasting EMR Adoption” about EHR adoption and success factors. Registrants get a free electronic or paper copy of the book.
Encore did a great webinar Wednesday on “Enterprise Data – Tapping Your Most Critical Asset for Survival” that some registrants couldn’t view because of a GoToWebinar problem in its latest code update. You can watch it above or on YouTube. Jonathan Velez, MD (CMIO – Hartford HealthCare) and Randy Thomas (Encore) did a nice job and filled the 40 minutes with solid information.
Meanwhile, here’s a case study on how to be a crappy software vendor like GoToWebinar, owned by Citrix:
- Don’t QA your new releases. Instead, outsource QA to your customers and then just roll them back to pre-broken versions when they call in problems.
- Don’t notify customers of known problems, especially those that affect critical processes like viewing and recording webinars. Admitting failure will shake their confidence.
- Instruct your support reps to quickly tell callers that their problem is a known issue. Everybody loves to hear it’s not just them.
- Keep support callers on hold when they call the high-priority service number and play annoying messages throughout telling them how great support will be once they get through. This heightens their anticipation.
- Propose illogical solutions, such as restarting a webinar already underway even though that would prevent anyone from seeing it. The support engineer will seem more skilled since no non-engineer would propose a similarly out-of-touch solution.
- Ask customers to trust you in rolling back to old code versions, even when they have no way to verify that the change works (unless they have 100 friends willing to hop on an impromptu webinar to see if they can get in). You trust them to pay their bills, so the should trust you to release pretty good code.
- Just give up, as did the person from Citrix who told me apologetically, “Maybe it’s time for you to find a new webinar provider.” This reverse psychology will make them want you even more.
I apologize if GTW’s bug locked you out of Wednesday’s webinar. The video above is perfect and worth watching.
Acquisitions, Funding, Business, and Stock

Craneware acquires Scottish patient access mobile systems vendor Kestros Limited, which has been selling primarily to NHS Trusts.

September 10 is a critical day for Castlight Health and its tanking share price: the lockup period ends and the pre-IPO shareholders will be able to sell up to 76 million shares, which closed at around $40 on IPO day in March but are now trading at less than $12. That’s a 70 percent haircut, but the company still has a $1 billion market cap on less than $30 million in annual revenue and huge losses. Maybe co-founder Todd Park can swing by on his new West Coast White House gig and apply Healthcare.gov-like CPR.
Sales

Robert Wood Johnson Health System (NJ) expands its relationship with NTT Data in selecting its Optimum RCM suite.

Kaweah Delta Health Care District chooses Access for electronic forms and patient signatures.
Marshfield Clinic (WI) standardizes on Client Outlook’s eUnity university image viewer and collaboration tool for its homegrown CattailsMD EHR.

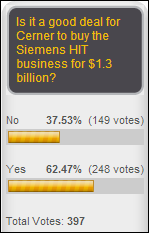
Georgia Regents Health System (Augusta, GA-based GRHealth) signs a $400 million agreement to turn over its IT operation to Cerner, which it says will save it 15 percent of its operating costs annually and make its annual expense predictable. GRHealth operates Georgia Regents Medical Center and Children’s Hospital of Georgia. The system says all 132 employees will receive offer letters from Cerner. Cerner became interested in the arrangement last year when the system signed a $300 million clinical technology partnership agreement with Philips, indicating along with the Siemens acquisition that Cerner sees a future in merging IT systems with clinical monitoring.
Sunquest will expand its relationship with private pathology lab CellNetix to work on anatomic pathology workflow solutions.
People

Boston Software Systems promotes Steve Cohen to COO.

David Watson (Oracle) will be named CEO of the new California Integrated Data Exchange (Cal INDEX).
Announcements and Implementations
Walgreens the rollout of its Greenway Health EHR to all of its 8,200 locations, allowing its pharmacists to counsel patients and provide immunization and testing recommendations.
Aspirus Wausau Hospital (WI) announces an OR digital integration project that will feature a centralized OR hub equipped with touch-screen monitors that can display images from all devices and modalities. It will use Brainlab’s Buzz digital OR.

Sentry Data Systems announces its 340B Technology Backbone to help pharmacies manage their 340B drug purchasing programs.
Government and Politics

Bloomberg reports that Google executive Megan Smith is the top candidate to replace Todd Park as US CTO. Smith’s background is the Google X skunkworks lab, so unlike her predecessors Aneesh Chopra and Park, she has no healthcare experience. She is married to re/code technical reporter Kara Swisher, although they are separated.

Meanwhile, the White House confirms that CTO Todd Park will continue working for the White House after returning home to California, recruiting technical talent for government work in a new role of technical advisor. President Obama said in a statement, “From launching the Presidential Innovation Fellows program, to opening up troves of government data to the public, to helping spearhead the successful turnaround of HealthCare.gov, Todd has been, and will continue to be, a key member of my Administration. I thank Todd for his service as my Chief Technology Officer, and look forward to his continuing to help us deploy the best people and ideas from the tech community in service of the American people.”
Innovation and Research
XPRIZE names the 10 finalists competing for its $10 million Qualcomm Tricorder XPRIZE: Aezon (US), CloudDX (Canada), Danvantri (India), DMI (US), Dynamic Biomarkers Group (China), Final Frontier Medical Devices (US), MESI Simplifying diagnostics (Slovenia), Scanadu (US), ScaNurse (England), and zensor (Ireland.)
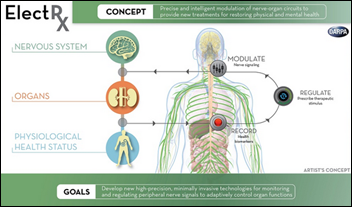
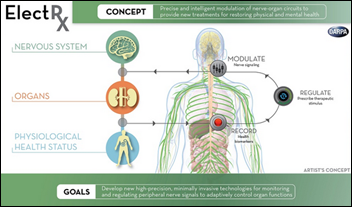
President Obama will champion ElectRx, a $79 million, five-year DARPA-run project to implant computer chips in troops and veterans to promote faster healing. The program’s manager describes it as “a closed-loop system that would work in concept like a tiny, intelligent pacemaker” to assess conditions and send electrical stimulation to induce healing. A related effort will detect mood changes associated with PTSD. I don’t know how they’ll deal with FDA approval.
Speaking at the American Legion National Convention in Charlotte, NC, President Obama said,
So we’re going to keep at this until we end this backlog once and for all. And as we do, we’re going to keep working to liberate you from those mountains of paper. We’ve got to move towards a paperless system — electronic health records that our troops and veterans can keep for life, and that could cut down on some of the bureaucratic red tape so that you’re getting the benefits that you’ve earned a little bit faster.
Technology
Korea-based medical wearables startup Ybrain raises $3.5 million in a Series A round. Its product isn’t the usual fitness tracker: the US-educated team has developed an electrical stimulation device that it says can combat the effects of Alzheimer’s when used at home for 30 minutes per day, five days per week. The company hopes to launch its service in early 2015.

Apple co-founder Steve Wozniak says he expects the company to create a market for wearables starting with upcoming announcements on September 9 that will likely include the iWatch. He says he expects fitness monitors to be involved and maybe an EKG display at some point, but in the mean time, he’s not a fan of the category:
I feel that wearables are a hard sell. They are go-betweens for your smartphone but are an extra piece and need special advantages that the smartphone doesn’t have, in my opinion. If they are just a Bluetooth go-between then it could wind up in the category of Bluetooth headsets: Fun to wear and show off for a day.

Discover magazine highlights three projects that owners of 3-D printers can perform to help people in need. Among them: use downloadable designs to print and assemble a prosthetic hand for someone who needs one, requiring around $50 in parts and 8-14 hours of printer time. The first e-NABLE conference will be held at The Johns Hopkins Hospital (MD) on September 28.
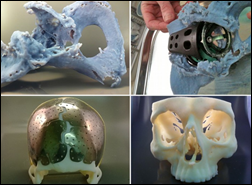
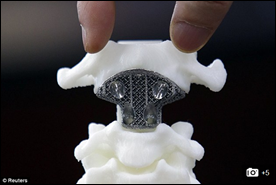
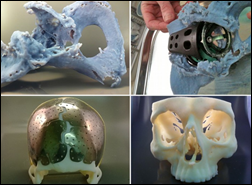
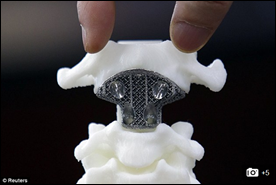
More on 3-D printing: in the UK, 12 NHS trusts are using 3-D printers to test implants before surgery to reduce cost and OR time, including bones for facial reconstruction surgery, hip replacements, and forearms. In China, surgeons implant a 3-D-printed vertebra in the spine of a 12-year-old cancer patient.
Other
Sharp HealthCare (CA) becomes the tenth of the 32 Pioneer ACOs to drop out of the program, saying that local wages rose 8.2 percent in San Diego but the Pioneer model doesn’t adjust payments accordingly.
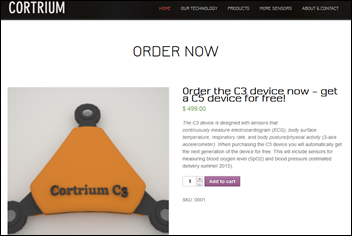
Drug maker Bayer starts a healthcare accelerator for Europe-based companies, offering a 3.5-month program of mentoring, free office space in Berlin, and around $65,000 financial support, taking as much of 10 percent equity in return. The five startups chosen from 70 applicants are Cortrium (a device that measures temperature, activity, respiration rate, and EKG); PharmaAssistant (medication reminders via smartphone); Parica (vital signs analysis); FabUlyzer (measuring fat burned after exercise); and Cardimoni (checks heart rate and rhythm).
AMIA’s annual meeting will be held November 15-19 in Washington, DC. The early bird member registration fee of $795 ended Thursday, August 28, but it’s still discounted to $895 through October 23 (then $995). Keynotes will be Amy Abernethy, MD, PhD of Flatiron Health (I interviewed her last month) and National Coordinator Karen DeSalvo, MD, MPH, MSc. Ross Martin, MD will head up the talent show, which will provide a musically equipped stage and a house band for participants, who need only bring “additional instruments, props, and groupies.”

Cisco CEO John Chambers says the US and other developed countries will go bankrupt if they don’t fix their healthcare systems, adding that technology has a key role (although he seems to pay little attention to the caregivers on the other end of it):
The first thing that will happen is all devices on our bodies, in hospitals and in our homes will be connected. The second technological advance is video, which is the way people will prefer to communicate in the future. Video can connect any health care professional to any patient and to any specialist, all at tremendous speeds. You’ll be able to receive medical expertise 24/7. Health care applications will combine the technologies of cloud and big data, whether in the hospital or in your home. Video allows a different level of collaboration, and it offers security and privacy from your home. This is the Internet of Everything … in a typical hospital, there are nine to 15 different applications that were never designed to share information with each other. And without a common medical record that has the appropriate security and privacy built into it, moving data from one application to another is difficult … The end game should be connecting any patient to the best healthcare professionals in the world at any time, using video-driven, low-cost technology.
Greenway Health CEO Tee Green accepts his Ice Bucket Challenge, offering to make a donation to ALS Association for every employee who sends him a video of themselves doing the same.
Weird News Andy asks if Oompa Loompas were vegetarians because he never found them attractive: a study (of questionable scientific validity) finds that the healthy skin glow of people who eat high-carotenoid vegetables is more attractive than a suntan.
Sponsor Updates
- Kyle Silvestro of SyTrue will participate in a panel discussion titled “How Cloud Based Solutions Allow for Improved Coordination of Care and Patient Satisfaction While Reducing Overall Costs of Billing”at the Radiology Business Management’s fall conference October 19-21 in Seattle.
- GetWellNetwork CEO Michael O’Neil will facilitate a breakout session, “Interactive Patient Engagement and Activation Workshop: What’s in a Number?” and will present “ePatient Entrepreneur Story” at the Stanford Medicine X conference on September 4.
- Craneware announces the appointment of Russ Rudish (Deloitte Touche Tohmatsu) to its board as non-executive director.
- Emdeon launches its co-pay assistance program for retail pharmacies, Emdeon Easy Save.
- AirWatch renovates and expands its former headquarters.
- TeleTracking Technologies will launch multiple solutions at its client conference October 26-29 in Florida.
- Sentry Data Systems shares how a Rand report clarifies the 340B program impact and provides steps to ensure its longevity.
- NextGen announces that its ambulatory EHR V 5.8.1 has earned 2014 ONC HIT Cancer Registry Certification.
EPtalk by Dr. Jayne
Recent research at the University of Michigan finds that patients with low literacy and low comprehension of numerical concepts are less able to understand online lab results. The Internet survey of 1,800 adult patients looked at simulated diabetes results and whether patients understood if labs were within or outside of reference ranges. Less literate patients were also less able to determine when they should call their doctor, based on the data.
Researcher Brian Zikmund-Fisher is quoted as saying, “We can spend all the money we want making sure that patients have access to their test results, but it won’t matter if they don’t know what to do with them.” At the other end of the spectrum, over three-quarters of patients with higher literacy skills could identify levels outside the reference range. He goes on to state the need for more research on the best ways to display lab data.
When we first started releasing lab results directly to patients, our physicians voiced concerns. Physicians wanted to hold the results until they could put a comment with them, as they had done in the paper world. Many of our physicians would mail the patient a copy of the test results with a handwritten “OK” or “great” or “double your Lipitor and see me for fasting labs in six weeks.” Our administration overruled the physicians.
Initially we received more phone calls about labs. Most physicians changed their behavior to start counseling patients about potential lab results at the time they were ordered or drawn to reduce the potential for calls.
That approach is fine when you’re counseling a patient on an existing diagnosis or if the labs in question are “maintenance” labs, although it adds a new dynamic to the visit that we don’t always have time for. Looking at other scenarios, I don’t think it’s the best approach when you’re dealing with a new diagnosis, particularly if it’s an emotionally charged one such as cancer or other potentially fatal conditions. I’d like to at least get to those patients on the phone first before they see the results on the patient portal.
Our results release in real time, so it puts the physicians in the position of “stalking” lab results in the evening and over the weekend, then frantically trying to get in touch with patients before they log on. An uncertain diagnosis is certainly stressful for the patient, but it also weighs heavily on the physician. Adding time pressure isn’t optimal for anyone, especially if the physician needs to consult with other members of the care team prior to talking with the patient.

National Health IT Week is almost upon us again, with the goal of raising “awareness of Health Information Technology’s power to improve the health and health care of patients across the nation.” When IT solutions are used to transform care and improve quality it can be a powerful thing, but when tools are employed without goals, accountability, or governance, it doesn’t make the world a better place. There are key themes for each day of the week:
- Patient Engagement
- Advancing Interoperability Through Meaningful Use
- Advancing Interoperability Across the Care Continuum – Beyond
- Advancing Interoperability Through Standards
- Clinical Quality & Safety
I couldn’t help but notice that quality and safety are last on the list. I’m going to give ONC the benefit of the doubt and assume that they are building the week towards the most important aspect, but if that’s true, then it puts patient engagement towards the bottom.
Why do we seem to revere the means more than the ends? Email me.
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.


































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…