Top News


IBM and Epic start background work on the $11 billion Department of Defense EHR project for which they are bidding even though the award won’t go out until summer, saying they need a head start to meet the DoD’s aggressive timelines. IBM has installed an Epic model system in one of its government-level security data centers so that it can test an integrated in a DoD-like environment. The companies also announce that they have formed a 17-member advisory group that includes former Kaiser Permanente CIO Bruce Turkstra and military patient advocate Major William Lyles.
Reader Comments
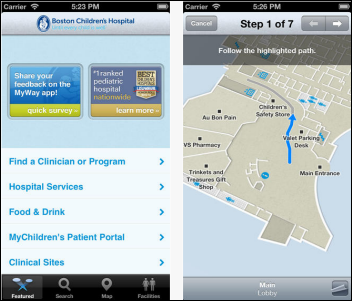
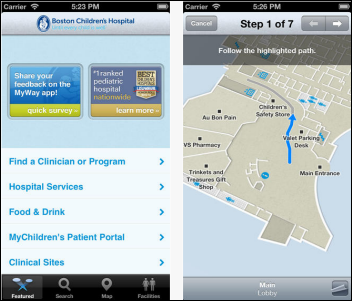
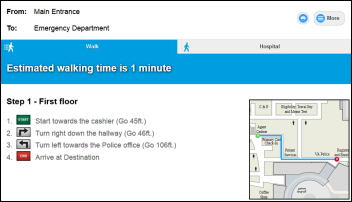
From Dan Nigrin: “Re: wayfinding apps. We’ve had Meridian’s technology in place for years at Boston Children’s.” Dan is the CIO at Boston Children’s, whose MyWay app offers a nice package of services for visitors and patients. I think hospitals that offer way-finding apps assume that everybody uses them, I bet the penetration is tiny. It would be nice as a patient to be able to get turn-by-turn instructions from the parking garage to a particular hospital department or physician office. Hospitals have the most consumer-unfriendly access that I’ve seen in any industry, starting with dreary pay parking garages and inadequate spaces for their huge numbers of employees. Tip: if you’re a vendor trying to get a meeting with a mid-level hospital IT executive whose non-CIO status doesn’t come with a reserved parking spot, offer to pick them up and drop them off curbside at their location – they’ll accept since they otherwise rarely leave campus for lunch because of the trek to get their car followed by endless cruising for an open space upon returning.
From Fracker: “Re: Meditech. Terminated its distribution agreement with Riyadh, Saudi Arabia-based National Technology Group.” Unverified.
From Vegas Baby: “Re: conferences CMIOs attend. Which ones are popular other than AMDIS?” The HIMSS conference probably has more CMIOs attending than any other conference, although obviously they make up a small percentage of attendees overall. AMIA would have a higher percentage but lower number, I’m guessing. Anyone have insight?
From Malice Cooper: “Re: HIStalkapalooza. Are you taking requests? I am sure demand is high, but I would love to be part of the event.” I haven’t yet put up the “I want to come” page. I need to finalize who’s sponsoring the event to figure out how many people I can afford to invite. That will tell me when I’ll have to cut off requests, assuming that demand exceeds supply, which has happened every year since the first (tiny) event in 2008. I’ll also have a great HIStalk sponsor networking event the Sunday of HIMSS week and will send details about that shortly for those looking to swap war stories or strike deals.
HIStalk Announcements and Requests
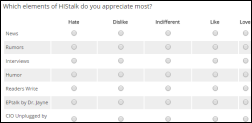
It’s time for my once-yearly HIStalk Reader Survey, which helps me picture who’s reading and to get your advice. I would really appreciate your participation since, as usual, I’ll plan everything I do this year based on the results. I’ll also randomly choose three respondents to win a $50 Amazon gift certificate. Thanks for taking a handful of minutes to help me out.
Early January also means its time for your HISsies nominations. Tell me the worst vendor, the smartest vendor action taken in 2014, the industry figure of the year, and the all-important “Industry figure in whose face you’d most like to throw a pie.” The final ballot will contain the most-nominated entries, so think of this as the primary election that precedes the general one by a couple of weeks.
This week on HIStalk Practice: New Hampshire pediatricians sound off on the state’s non-existent vaccine registry. HealthTap CEO brings telemedicine back down to Earth. HHS looks for vendors to run its National Data Warehouse. Healthcare gets New Jersey physicians down in the dumps. EHRs create threats to confidentiality. 23andMe sees investment revival. Thanks for reading.
This week on HIStalk Connect: The year’s biggest digital health stories are recapped, including: unprecedented VC funding levels for digital health startups; Apple, Samsung, and Google all expanding their presence in the digital health sector; 3D printing finding more uses in healthcare, DNA sequencing breaking through the long-awaited $1,000 price barrier, and IBM doubling-down on its Watson supercomputer despite a slower than expected road to profitability. During this week’s CES conference in Las Vegas, Withings unveils its newest fitness tracker, Alterica introduces a smartphone-connected EpiPen case, and Cambridge Consultants shows of breakthrough technology in sensor-laden sportswear.
Webinars
January 13 (Tuesday) 1:00 ET. “The Bug Stops Here: How Our Hospital Used its EHR and RTLS Systems to Contain a Deadly New Virus.” Sponsored by Versus Technology. Presenter: John Olmstead, RN, MBA, FACHE, director of surgical and emergency services, The Community Hospital, Munster, Indiana. Community Hospital was the first US hospital to treat a patient with MERS (Middle East Respiratory Syndrome). It used clinical data from its EHR and staff contact information from a real-time locating system to provide on-site CDC staff with the information they needed to contain the virus and to study how it spreads. Employees who were identified as being exposed were quickly tested, avoiding a hospital shutdown.
Acquisitions, Funding, Business, and Stock

Par8o, which grandly styles itself as “Healthcare’s Operating System,” raises $10.5 million in Series A funding. The referral management software company, whose name is a play on the word “Pareto,” was co-founded by Sermo co-founders Daniel Palestrant, MD and Adam Sharp, MD. Customers include hospitals that are part of the Harvard and Mount Sinai health systems.

Entrepreneur and author Sramana Mitra profiles for her upcoming book those “Unicorn” companies that generate their initial funding from sales rather than from financing, listing among them eClinicalWorks, which she says has $300 million in annual sales and, “If it were valued, it would easily be a multi-billion dollar company.” ECW’s Girish Kumar is among the most astute, genuine, and interesting people I’ve ever talked to.

HCS announces record sales in 2014 with 19 percent revenue growth and the addition of 30 employees.

McKesson shares hit a 52-week high Thursday, valuing the company at $50 billion. Above is the one-year share price of MCK (blue, up 24 percent) vs. the Dow (up 9 percent).

A venture capital firm increases its stake in Etransmedia with an unspecified investment that will support the company’s merger with physician practice services vendor DoctorsXL.
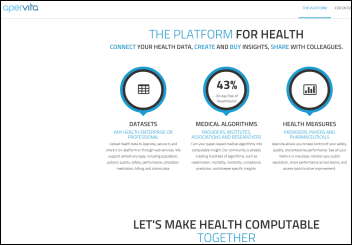
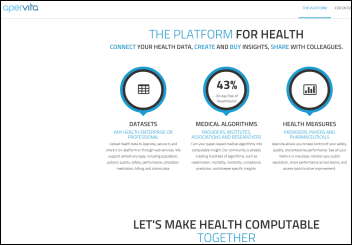
Chicago-based health analytics and algorithm sharing marketplace vendor Apervita, known until last week as Pervasive Health, completes an $18 million Series A funding round. It’s an interesting concept – allowing people to buy and sell health-related databases, algorithms, and measures.
Sales

Rush University Medical Center (IL) chooses Merge Cardiology PACS. MRGE shares have jumped 71 percent in the past 90 days vs. the Nasdaq’s gain of 8 percent.
Health Information Network of Arizona selects Quality Systems subsidiary Mirth to provide patient information exchange.
People

GetWellNetwork hires John George (StayWell) as chief growth officer.

Tom Stampiglia (Origin Healthcare Solutions) joins Surgical Information Systems as president and CEO.
Announcements and Implementations
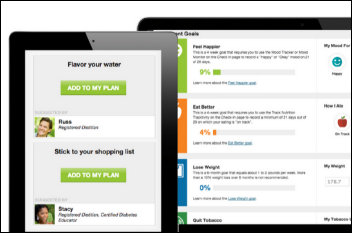
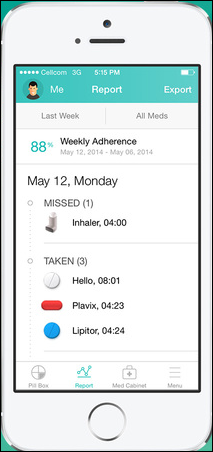
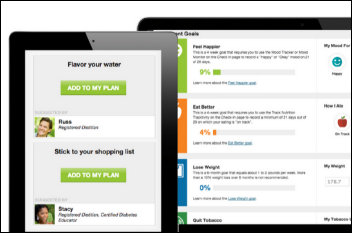
Walgreens adds Your Digital Health Advisor, a virtual coaching program developed by WebMD, to its website and mobile app. The app includes programs for smoking cessation, weight management, nutrition, exercise, and emotional health and also offers real-time 24×7 coaching via Walgreens Pharmacy Chat. It will connect to WebMD’s iPhone app Health Target, which lets users upload their data from connected devices to receive physician-reviewed advice and tips. Users who meet their health goals earn Walgreens Balance Reward points.
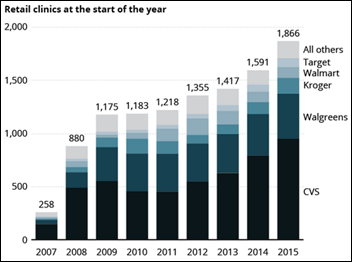
Walgreens also announces that it will use Qualcomm’s medical device connectivity for remote patient monitoring and chronic care management, initially offering integration with Walgreens blood pressure cuffs and glucose meters. A new line of Qualcomm-branded devices will be announced in the next few months. This, too, will reward members with Walgreens Balance Rewards points for their participation. Walgreens is unbelievably ahead of just about everybody in healthcare in terms of technology use, consumer connection, and industry partnerships. Their technology creates revenue instead of just expense. I tried to connect with the company to interview its CIO, but they didn’t respond to my inquiry.
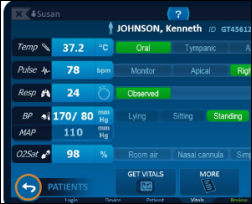
Capsule announces GA of its SmartLinx medical device information system that includes patient surveillance, clinical decision support, alarm interpretation and alerting, and asset tracking.
InterSystems HealthShare is certified as an eHealth Exchange Validated Product.
BD Medical gets FDA clearance for its Intelliport Medication Management System, which provides real-time drug identification, dose checking, and allergy detection at the point of IV bolus injection and then wirelessly documents the drug’s administration in the EHR. The system, which includes an IV access site sensor, wireless base, and table software, will reach the market in spring 2015. It will be marketed for use in perioperative areas to reduce syringe swap, dosing errors, and manual documentation requirements. This looks like a very cool product, even smarter in some ways than IV infusion pumps, and bolus dose errors cause patient problems much faster than an IV.

O’Reilly releases a freely downloadable e-book, “Data Driven: Creating a Data Culture,” that contains interesting business examples including a cool one that studied why people who had tried Twitter stopped using it. It’s a straightforward, hype-free overview of the possibilities of using data to do good work. I ran across it by accident – I like it a lot.
A DrFirst market share analysis of EHRs used in New York finds that 80 percent of the ambulatory EHRs and 85 percent of the hospital EHRs are ready for the state’s I-STOP law that takes effect March 27, 2015. The law requires that all prescriptions be sent electronically from prescribers to pharmacies. New York pharmacies aren’t as well prepared as prescribers, however, with only 58 percent of them ready to accept electronic prescriptions for controlled drugs.

NantHealth announces a new version of its HBox medical device that collects and transmits real-time information from blood pressure cuffs, scales, and other personal devices using technology from BlackBerry.
Skylight Healthcare announces a secure videoconferencing solution that connects hospitalized patients with up to four other people simultaneously via the company’s interactive patient engagement technology.
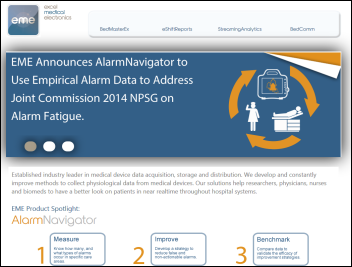
Erlanger Health System (TN) becomes the first US hospital to roll out AlarmNavigator from Excel Medical Electronics, which helps users analyze alarms from GE patient monitoring systems to support customizing settings to reduce alarm fatigue.
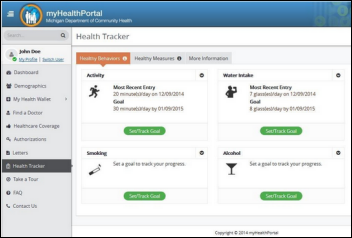
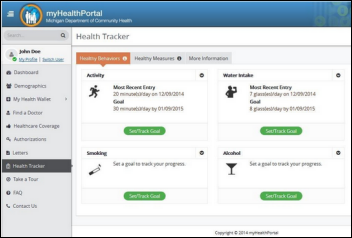
The Michigan Department of Community Health launches a mobile app and portal so that Medicaid patients can access their medical information remotely.
Government and Politics
The FCC proposes updating its 2010 definition that said “broadband” has a minimum speed of 4 Mbps down/1 Mbps up to instead require 25/3 Mbps. The agency says rural and Tribal lands are underserved, with the proposed definition change upping the requirements for broadband providers that requesting federal grant money to add services. Both AT&T and Verizon had already objected to a previously proposed 10/1 Mbps minimum speed requirement, saying 4 Mbps is plenty for consumers.
Innovation and Research
The Economist corrects yet another example of attention-seeking publications that create inaccurate headlines and stories hoping for salacious clicks. It turns out that despite the recent hype, getting cancer isn’t only due to bad luck. The original research paper said that two-thirds of the variation in cancer risk is caused by chance mutations, which is not the same thing as saying that two-thirds of the chance of getting cancer is due to luck (since not every mutation causes cancer in the given tissue). The authors explain that cancer is “a combination of bad luck, bad environment, and bad inherited genes” and people control 40 percent of the risk via their lifestyle decisions about smoking, diet, sunlight exposure, exposure to papilloma virus, obesity, exercise, and alcohol intake.
Technology
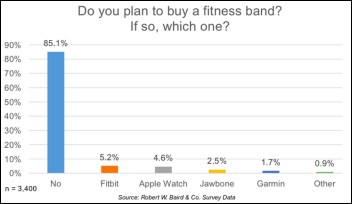
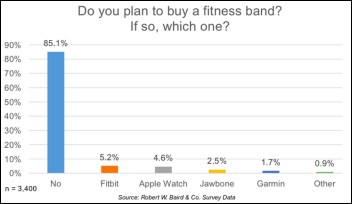
A survey finds that while fitness tracker companies desperately try to outdo each other with added features and higher prices, 85 percent of consumers have no plans to buy one.
Other
Athenahealth says its network and previous years’ data suggest that the flu season has peaked, although CDC’s just-updated report says 29 states have high flu intensity. February is usually the worst flu month.
A new survey finds that nearly two-thirds of Americans couldn’t afford to write a $1,000 check for an unplanned ED visit. More than one-third of them would dip into savings, 26 percent would have to cut back elsewhere, 16 percent would borrow the money from family or friends, and 12 percent would charge the amount to their credit card.
Sponsor Updates
- Allscripts will integrate Perceptive Software’s enterprise content management into its EHRs, giving customers a common infrastructure for storing and sharing patient content.
- Medicity publishes case studies on Trinity Health’s use of Medicity HISP to transmit information and Intermountain Healthcare’s lab results notification and public health reporting via Medicity Exchange. Brian Ahier, Medicity’s director of standards and government affairs, publishes an article with Wisconsin Statewide Health Information Network COO Jean Doeringsfeld titled “FHIR and the Future of Interoperability.”
- Teramedica-sponsored Vendor-Neutral Archive Institute of Technology offers free online courses that include CPHIMS and CPHIMA credit.
- Direct Consulting Associates will sponsor “Becoming a Game Changer in the World of Healthcare Technology” on January 29, 2015 in Scottsdale, AZ. Texas Health Resources SVP/CIO Ed Marx will deliver the keynote address.
- Logicworks publishes a blog on healthcare security, highlighting three reasons why hackers target healthcare clouds.
- Liaison Technologies publishes a new blog on next-gen data integration and management by Chief Marketing Officer Manish Gupta.
- Local papers profile Ingenious Med President and CEO S. Hart Williford’s work with startups; and COO Mike Pickering’s work with the Atlanta All Stars Talent Show Network, a non-profit community outreach program he founded in 2004.
- Impact Advisors offers a snapshot of its latest white paper, on population health management, in a new blog.
- Huntzinger Management Group Client Executive Rob Tashiro will speak during a CHIME webinar on January 28 covering lessons learned from big bang implementations.
- Optum’s latest blog looks at how providers use analytics to better manage their populations and reduce costs.
- Healthfinch sets intentions for the new year in a new blog post.
- Healthcare Data Solutions shares insight into the Walgreens-Qualcomm partnership in a new blog post.
- HCI Group’s SVP of Delivery Operations Robert “Bob” Steele receives his HIMSS senior member certification.
- Hayes Management Consulting posts a new blog on the advantageous countdown to ICD-10.
- DocuSign will host the Tech Founders Forum in San Francisco on January 13.
EPtalk by Dr. Jayne

While I share many of Mr. H’s pet peeves with regards to grammar, my top peeve at the moment is misleading headlines. It was bad enough when it was just Yahoo and MSN, but now the sensationalism is rampant in various physician publications. Medical Economics screams “Meaningful use penalties sear more than half of EPs in 2015.” Personally, “sear” wouldn’t be the verb I would choose for a 1 percent Medicare penalty. Tintoretto’s “The Martyrdom of St. Lawrence” illustrates what it would really look like to be seared.
Massachusetts physicians will need to update their own pet peeve lists with this one. The Massachusetts Board of Registration in Medicine recently adopted a regulation that requires demonstration of Meaningful Use as a condition of licensure. It went into effect last week. Fortunately, they’ve built some flexibility into the final requirement. Beyond successful attestation as an Eligible Provider, other options include:
- Completing continuing medical education that discusses EHRs and the MU programs objectives and quality measures.
- Employment, contracting, or credentialing by a hospital that is participating in MU.
- Participating in the Massachusetts Health Information Highway.
Physicians renewing their licenses prior to March 31 can receive a single-use “get out of jail free” exemption. If you’re due for renewal within 60 days of the end of March, you can take advantage of it as well by applying early, so get those checkbooks ready.

For those of us who wear many different hats (CMIO, practicing physician, anonymous blogger) time management is a constant challenge. If you’re as compulsive as me about it, you’ll want to consider blocking time on your schedule to peruse the proposed rule for Meaningful Use Stage 3. I highly recommend slotting a weekend evening with a roaring fire and a nice bottle of wine, as that worked well for me when Stage 2 was released. Given the state of my average work week, there’s no way it’s going to happen during normal business hours.
If you’re new to the game, the proposed rule currently sits at the Office of Management and Budget. It will be published in the Federal Register once the OMB review is complete. Stage 3 is supposed to focus on using the work done in previous stages to actually drive improvements in patient outcomes. According to statements from HHS, there will also be changes in the reporting period and program structure.
They also hope to clarify the definition of Meaningful Use (given confusion about requirements from multiple stages and multiple revisions) and to make sure the program is sustainable. I don’t have a crystal ball, but I hope there’s a 90-day reporting period involved and that they give vendors at least a year after finalization of the Rule to write code and physicians a year to install and upgrade.
Earlier this year, the Health IT Policy Committee recommended that HHS incorporate fewer objectives and reduce the burden on providers. Various other constituencies have pushed for further narrowing of the requirements. I’d bet we have the NPRM in the Federal Register within the next few weeks, so get your wine selections ready.

HIMSS is releasing more information about the conference and several new offerings including a Cybersecurity Command Center, Disaster Preparedness Knowledge Center, and the HIMSS Health IT Value Suite. Another new offering is HX360 , a joint effort of HIMSS and AVIA to look at non-EHR technology that can benefit health systems and provider organizations. I was initially drawn to it, but seeing that they’re charging an additional fee to attend the “Venture+ Forum pitch competition for early stage companies” dampened my enthusiasm. I don’t think what they’re offering is worth an additional $225 (or $795 as a standalone) of my hospital’s money.
I’m a little more enthusiastic about the “HIMSS Speakeasy” theme for the opening reception, which is usually pretty vanilla. Who’s ready to bob their hair and pack their flapper dresses and dancing shoes? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.























































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…