From HIMSS 4/14/15
HIStalkapalooza took up a lot of my time yesterday, so I didn’t even have time to post. This will be a dribs-and-drabs version – I’ll have more time the rest of the week to get organized. Let me know if there’s something I should make sure to see since I’m just flailing around for the most part.
From Anonymous Vendor President: “Re: Dana Moore and DonorsChoose donations. We will anonymously match whatever total you raise up to $5k. Let’s make this thing really work! Many of my family and countless within our company have ties and heartstrings attached to the cause.” Centura SVP/CIO Dana Moore will be in our booth Wednesday, meeting with vendors for 20 minutes each in return for their $500 donation to DonorsChoose. I’ve scheduled six sessions with him so far, meaning with with the very generous anonymous matching funds, we’ll be donating $6,000 for individual classroom projects via DonorsChoose. I have a bunch of teacher thank-you emails to get through from the projects already funded. Next up is the fun of funding new projects. Thanks to everyone involved.
From Kaboodle: “Re: MedStar in Maryland. You failed to mention their GE Centricity EHR crash, where all clinics were down and back to paper. But, but mind you, care was not affected!” Unverified. I haven’t heard anything about it.
HIStalkapalooza
I haven’t had much time to do the post-mortem on HIStalkapalooza since I didn’t get back until well after midnight. House of Blues was perfect and ran things with great skill, the food and bar service was really good, and the band was as outstanding as I remember them from last year. I was backstage the whole time so I didn’t experience the event as an attendee this time around, which I sort of regret, but I could feel the energy and excitement. Some notes:
- Lorre Wisham worked on the event for many months going back to last spring. She arranged everything you saw or did as an attendee, wrangling an enormous list of to-do items (contracts, menus, sponsors, band details, banners and signs, etc.) The many hundreds of hours were in addition to her doing her “real” HIStalk work.
- I would have gone seriously broke without the financial help of the event sponsors since we had to sign band and venue contracts almost a year ago, putting me at complete financial risk if sponsors hadn’t participated. Thanks to Elsevier, Santa Rosa Holdings, Divurgent, Sagacious Consultants, Aventura, CommVault, Falcon Consulting Group, Greenway Health, PatientSafe Solutions, Sunquest, Thrasys, and Validic for making it happen. Those who had opera boxes seemed to be enjoying themselves as Lorre checked in with them several times through the evening.
- Sagacious did a superb job checking people in (and apparently, according to their report, keeping quite a few people out who showed up but weren’t supposed to be there). HOB says we had close to 1,000 people in the house (of 1,500 invited), meaning their folks got everybody in professionally and cheerfully. Elsevier ran the red carpet and I heard people enjoyed that.
- The House of Blues staff was super professional and treated us like the big-name acts they host there.
- Rocking doctor Ross Martin kicked it off in style despite a technical snafu that prevented us from enjoying the big finish of his freshly updated Interoperetta. I’ll try to get something on audio or video from Ross so we can hear the full version.
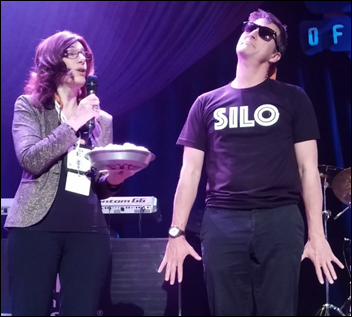
- Barry Wightman and Jennifer Lyle were great hosts on stage. It’s harder than it looks to engage a huge room full of partygoers and managing the people and equipment on stage.
- Special thanks to Judy Faulkner and Jonathan Bush for presenting each other awards on stage in a funny but classy manner.
- I can’t really say anything about Party on the Moon because if you were there, you already know how electrifying they were, and if you weren’t, words alone can’t describe it. Lorre had vendors coming up to her wanting to know how to book them for their own events. The 13 band members came all the way from Atlanta on their tour bus to spend the evening with us. You know a band is killing it when, as one attendee pointed out, you have nerdy IT guys so anxious to participate that they dance with each other. There were some great moments out there in the audience. According to one attendee, “Easily the best party I have ever been to, as good or better than any fraternity party.”
- We have photos and video coming from several sources that I haven’t had time to review yet. Stay tuned and we can all relive the evening all over again.
Neil Versel took some good pictures of the Judy and JB show, even though he annoyed me by dismissively referring to HIStalk as the “National Enquirer of health IT.”

A nice HOB exterior shot by Rudy Flores. The stencil over the light that shines the logo — I now know having ordered three of them for this event — is called a “gobo,” just in case you want to increase your vocabulary.
Somewhat Interesting News Announcements
- IBM creates Watson Health with the announced acquisition of Explorys (analytics and population health management) and Phytel (population health management). The company also announced health partnerships with Apple, J&J, and Medtronic.
- Surescripts creates a National Record Locator Service along with EClinicalWorks, Greenway, and Epic that will allow providers to locate and exchange patient health records using the Carequality trust framework.
- InterSystems announces a vendor-neutral, interoperable patient portal.
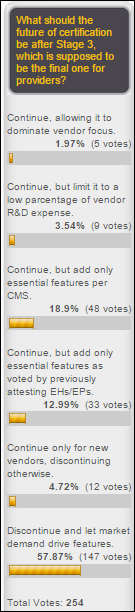
- HIMSS turns the work of its interoperability workgroup into a certification program for EHRs, HIEs, and HISPs, run by ICSA under the name “ConCert by HIMSS.” I don’t think of HIMSS as the group that should be certifying products, but apparently their opinion differs from mine.
- KPMG acquires Beacon Partners, as was predicted in an HIStalk rumor report a couple of weeks ago.
- Peer60 publishes a free report titled “Will mhealth Drive Patient Engagement?” that questions whether EHRs provide adequate mobile support to meet consumer expectations.
Today in our booth (# 5371)
All day (I think): Regina Holliday will be painting
11:00 Funny lawyer Steve Blumenthal will be handing out swag and dry humor.
2:00 NVoq will hand out Garrett Popcorn (it’s the great Chicago kind that costs a fortune in the airport).
3:00 Your HIStalkapalooza host Barry Wightman will be autographing copies of his book “Pepperland” (which I enjoyed a lot).
4:30 The Walking Gallery will meet.
I forgot that we intended to auction off Regina’s HIStalking original painting from which we made the scholarship winner tee shirts. Make Lorre an offer if you are interested. Maybe she can post the highest current bid on an index card underneath it or something.
My Fitbit shows that I walked 12 miles Monday. It felt like I wasted a lot of time just walking around, but that’s par for the course on the first day of the conference.
The folks at XG Health Solutions (a new HIStalk sponsor that I haven’t announced yet) invited me to a breakfast briefing covering their new apps. It’s a Geisinger spinoff that will sell software based on work done there to present clinicians with a better view of EHR data and collect additional information to make it easier to quickly understand patient problems and concerns and to document additional specialty-specific findings (rheumatology is the first one). Partnerships were announced with Epic, Cerner, and Athenahealth, whose EHRs will exchange information with the XG apps using SMART on FHIR. They have four apps going to beta testing by summer and plan to roll out six over the next 18 months.
From the hallway conversations I heard and my own opinions, here are the positives: Geisinger has developed a lot of expertise and content that’s less ivory tower than most big academic medical centers, they put some thought into involving the patient in the use of their apps, and the SaaS-based subscription means new best practices can be put into place quickly. Negatives: the company has significant venture capital ownership (they aren’t Geisinger, in other words), you might suspect that Geisinger applied soft pressure to the newly named EHR vendor partners to get on board with uncertain future commitments, and so far they’re a company that hasn’t done much to dent the market other than to do Geisinger stuff and make announcements. Success in commercializing hospital software is elusive, and while Version 1.0 is easy, it’s Version 2.0 that gets ugly with upgrades, design decisions, and testing. The first non-Geisinger betas will be important.









Some notes from my circuits around the exhibit hall (actually both of them – it’s a split hall that ensures confusion and uneven booth traffic). My badge is intentionally unimpressive to vendors, so I get the same treatment as everybody else.
- Trying to find a given booth even when you know its number is maddening given the gerrymandered aisles. The printed floor layout is laughable – you would need a high-powered microscope to read any part of it except the anchor booth companies (which may be the intention, come to think of it).
- Booth reps were screwing around with their phones literally from the moment the exhibits opened. It was depressingly easy to find booths where every single person was staring in rapt attention at their phones while prospects passed by without even being acknowledged. Vendors are really stupid in not coaching and policing their people.
- Even the fake patient in the hospital bed was surreptitiously killing time with her phone while waiting for her next scene. Check her out in the photo above – I wasn’t quite sure what was going on under those sheets until I came around to the head of the bed.
- I have three mandatory HIMSS kickoff rituals – I have to stroke the sultry curves of the latest Enovate cart; I have to have amazing scones from MedData (the orange chocolate chip were great, but I swung by later for one that had ham, cheese, and what looked like chives); and I have to see the magic guy in Hyland’s booth (above), who is simply amazing not only magically, but in snarky humor and getting people to come closer. I don’t usually like that kind of stuff, but he has been my favorite part of HIMSS for a bunch of years.
- Amazon Web Services had a little booth, which was interesting.
- A guy from Network Detective for Healthcare pitched their product that analyzes the network looking for HIPAA-related problems. It seemed pretty cool, especially the report showing the results in plain English with cross-references to HIPAA sections.
- Scotland-based Nugensis had guys in kilts and bottles of Scotch on the shelf.
- I tried to use the HIMSS app, but it locked up, spammed me with some guy’s endless and boring motivational quotes, and then started pushing ads as notifications. Big waste of time. The conference is basically just one giant advertising platform already.
- The NextGen booth was very cool with clear walls and a waterfall.
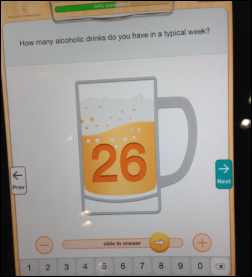
- Elsevier demoed their Tonic iPad app that collects information from patients. One of the cool aspects is that it can steer patients to automatically log on to the patient portal without their even realizing that it’s a separate app, which is nice for Meaningful Use. I didn’t see many products Monday, but this one was my favorite. That’s my bad iPhone picture of it above with the beer mug.
- The nice folks at zCover gave me a new iPhone case to replace the one they gave me a couple of HIMSS conferences ago. Stop by and they’ll even put it on for you.
- The FHIR puns were plentifully irritating. IT geek humor doesn’t usually work.
- Kforce was giving out pretty decent pizza way back in a low-density corner of the hall.
- Sagacious had their fun HIStalkapalooza posters out.
- InterSystems had a huge audience for one of their presenters. Their presence was significant.
- I stopped by the Microsoft booth and, as happens every single year, the reps were too busy yapping at each other to even look at all those prospects invading their space. As also happens every year, I stood patiently in front of a display (mobile devices and Surface this time) and the nearest Microserf stormed by scowling while nearly pushing me out of his way. Perhaps that’s why, unlike years past, their booth didn’t have much traffic.
- The Georgia display featured the sign I had made for them a few months ago following Atlanta’s HIStalk poll win.
- Bathroom capacity and seating space were ridiculously inadequate. I hiked forever down a long hall following the restroom sign, only to be met with the dreaded “pardon our dust” sign that said to find another restroom without actually saying where one might be. Another one had a grand-looking entrance, but inside was just one stall and one urinal. I’m thinking of one of those parking space type apps where I hire people to sit in the very few actual seats where people can relax or eat, then providing an app for attendees to find and buy their seats. It makes me uneasy to watch guys in crisp white shirts slopping down a wildly overpriced commissary barbeque sandwich while standing in front of a trash can.

Tahoe Forest Hospital (CA) names CIO Jake Dorst as interim CEO. He’ll also continue as CIO.
The outcome of dueling lawsuits between Allscripts and Medfusion may hinge on interpretation of the use of an Oxford comma in their agreement, which is pretty fascinating.

A reader wants to know if anyone else thinks that having costumed female entertainers at the HIMSS opening reception crossed the border into sexism territory. I wasn’t there, but if they didn’t have any men, that might at least make me think about it. I noticed fewer obvious booth babes in the hall this year, so maybe the “skin to win” sales approach is finally and deservedly dying off. It would seem especially inappropriate to have a provocatively clad model pretending to be a company rep in trying to get the attention of a female CEO, CIO, or CMIO.
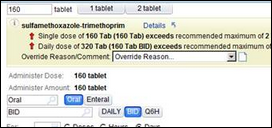
A terribly written and insight-free Forbes article click-baitingly titled “Two Dirty Little Secrets About Electronic Health Records” says EHRs are “a threat to freedom of speech and academic freedom” in claiming that EHR vendors (and Epic specifically) requires customers to sign non-disparagement clauses. The author works up righteous indignation for Bob Wachter, MD, who the author says had to get Epic’s permission to write about a UCSF medication error and to use Epic’s screenshots to illustrate it. The problem is the author just made stuff up rather than asking anyone involved and Bob had to correct him – Epic doesn’t include non-disparagement language in its contracts, although the screenshot part is true and Bob’s not thrilled about that (he emailed me to clarify that the author was wrong on the first point and has since changed the story). The second big secret is that EHRs are designed to help with billing and management. The author magnanimously proclaims that, “I’m not against EHRs,” which would be comforting except nobody’s ever heard of him and his mastery of the subject is clearly minimal.
That’s all for now. I’m headed over to McCormick Place later than I’d like.






















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…