Top News


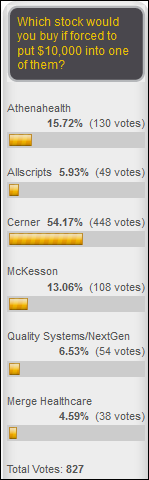
Quality Systems (NextGen) announces the retirement of President and CEO Steven Plochoki. He will be replaced by Carefusion SVP/GM Rusty Frantz. QSII share price dropped 14.5 percent in Plochoki’s seven-year tenure vs. the Nasdaq’s 111 percent gain.
Reader Comments
From LearnHealthTech: “Re: Florida Governor Rick Scott. Thanks for the new article on the stunningly corrupt and hypocritical governor. After defrauding taxpayers as a hospital CEO, he wants to go after non-profit hospitals for turning a profit.” Both for-profit and non-profit hospitals have plenty to be ashamed about, but Columbia/HCA’s felony fraud guilty pleas and $2 billion in settlement costs top the list. I suppose I shouldn’t be so critical because: (a) our healthcare system rewards aggressive business tactics, as evidenced by the stock market success of for-profit hospital operators and big healthcare-focused companies like McKesson and any number of insurers; (b) CMS’s “pay and chase” payment methods encourage health systems and companies to interpret its rules favorably in asking forgiveness rather than permission, no different than companies dealing with the IRS; and (c) Scott is right about the non-profit hospitals that still manage to have hundreds of millions of dollars in “excess revenue” that never seems to result in their overpaid CEOs offering to return the money, which usually means they just spend it on outcomes-indifferent activities such as buying up physician practices or erecting fancier buildings.
From Marshall: “Re: Connecticut hospital CEO salaries. Boosted handsomely.” Ten non-profit hospital executives made between $1 million to $3.52 million, with one CEO’s compensation increased 133 percent from $1 million to $2.3 million in just one year, while a second CEO saw his pay bumped by 85 percent to $3.1 million in the same year. The health systems didn’t provide a response to the newspaper’s inquiries, but it’s always the same anyway: (a) we have to pay that to keep him and we’re lucky he hasn’t left for greener pastures; (b) it’s not our fault that the market commands such high salaries and it’s a really hard job; or (c) we’re not really paying that much – it just looks that way because of one-time benefits such as payout of accrued retirement or severance benefits.
HIStalk Announcements and Requests
Thanks to the following sponsors, new and renewing, that recently supported HIStalk, HIStalk Practice, and HIStalk Connect. Click a logo for more information.












This week on HIStalk Connect: Dallas-based telehealth provider Teladoc enjoys its first victory in its antitrust lawsuit against the Texas Medical Board. The National Cancer Institute announces the start of a multi-arm cancer research project that will attempt to match cancer drugs with cancer-related genetic mutations. Google’s artificial intelligence research team is working on an app that will calculate the total calories in a plate of food by analyzing a picture of it. Rockwood City, CA-based digital health startup BaseHealth launches a genome API that will enable developers to integrate personalized care plans and risk reports into wellness applications.
This week on HIStalk Practice: Persivia CEO Mansoor Khan gives Jenn the scoop on starting up a new population health management company. Northwestern Counseling & Support Services connects to the Vermont HIE. Dr. Gregg describes the “bastardization” of HIT. CVS Health partners with HHS. Hughston Clinic rolls out TrainerRx software. TMA PracticeEdge COO Dave Spalding lays out the vision for ACOs in Texas. CMS opens up data for further research and development, and gives physicians an easy way to rat out information blockers. Solutions Recovery Center goes with ZenCharts. Gastro Health launches virtual support community.
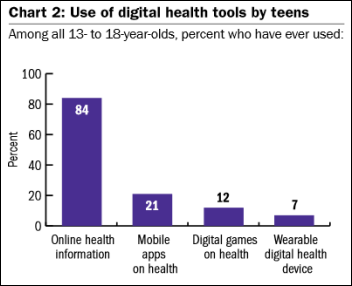
I was thinking about the plethora (and increasing number) of proprietary body sensors tied to specific apps or services. That sensor-app connection is mandatory at the moment, particularly with FDA-approved systems, but at some point the sensor overlap and need for economy of scale would seem to make it desirable for a single universal sensor that all health and fitness apps can talk to. It seems inefficient for every app vendor to develop and maintain yet another heart rate or calories-burned gadget, especially when consumers need or want information that requires more than one of them.
Webinars
June 9 (Tuesday) 11:30 ET. “Successful HIEs DO Exist: Best Practices for Care Coordination.” Sponsored by Medicity. Presenters: Dan Paoletti, CEO, Ohio Health Information Partnership; Brian Ahier, director of standards and government affairs, Medicity. Not all HIEs are dead – some, like Ohio’s CliniSync HIE, are evolving and forging a new path to successful care coordination. Brian Ahier will explain how HIEs can help providers move to value-based care models, emphasizing Meaningful Use Stage 3 and FHIR. Dan Paoletti will provide best practices in describing CliniSync’s journey to success in serving 6,000 primary care physicians, 141 hospitals, and and 290 long-term and post-acute care facilities. Attendees will learn how to use a phased approach, establish client champions, help providers meet MU Stage 2, create a provider email directory, deliver care coordination tools, and drive continued ROI.
Acquisitions, Funding, Business, and Stock

Genstar, owner of behavioral EHR vendor Netsmart, has reportedly retained an investment bank to either take the company public or sell it, with a potential price of $750 million. Also on the block, according to insiders, are health IT firms Precyse Solutions, Mediware, Edifecs, Caradigm, and Altegra Health.
Telemedicine provider Carena receives $13.3 million in funding from Cambia Health Solutions and McKesson Ventures to continue development of its virtual clinic solutions, which it says can be brought live 90 days after signing as a branded virtual clinic.
GE is rumored to be shopping its GE Capital Healthcare Financial Services unit for up to $11 billion as it dismantles GE Capital.
Shares of value-based care consulting firm Evolent Health begin trading on the New York Stock Exchange Friday at $17, which values the company — formed in 2011 by UPMC Health Plan and The Advisory Board Company — at $800 million.
Sales
East Jefferson General Hospital (LA) signs up for MedCPU’s clinical decision support system. I interviewed EJGH CMIO Beau Raymond, MD a couple of weeks ago.

Penn State Hershey Medical Center chooses PeraHealth’s clinical surveillance system.
People

Patient engagement solutions vendor TeleHealth Services names Gary Kolbeck (GK Consulting Services) as VP of business development.

Ted Reynolds (CTG Health Solutions) joins Impact Advisors as VP.
Announcements and Implementations

Provide Medical Park (WA) goes live on the Advantages RTLS patient flow system from Versus Technology, which allows patients to skip the waiting room and proceed directly to an available exam room.
CitiusTech launches CQ-IQ, a cloud-hosted quality analytics platform for CQM reporting that includes 250 pre-built quality measures across several care settings. I interviewed CEO Rizwan Koita in January.
Former Facebook CFO David Ebersman launches Lyra Health, which offers behavioral health screening tools and care coordination. His co-founder and chief medical officer is Dena Bravata, MD, who left Castlight Health in December 2014 after five years as chief medical officer and head of products.

Two public relations firms, one of which focuses on sensitive federal government issues, form ATDigitalHealth, which will promote interoperability and telehealth services to lawmakers.
Government and Politics
The opening of the Topeka, KS VA hospital’s ED – closed for almost a year and a half due to staffing shortages — is delayed for at least six more weeks as the VA’s central office requires it to upgrade its EDIS.
Privacy and Security
A report by cyberdefense vendor TrapX finds that most healthcare organizations are vulnerable to Medjack (medical device hijack), where hackers locate unpatched, Internet-connected medical devices and use them as a back door to penetrate the health system’s network. The attacks, which are made easier by FDA restrictions on keeping devices it has approved updated, are hard to detect since security teams can’t view a device console and can’t just disconnect them for maintenance.
Plans by the Federal Employees Health Benefits Program to launch a claims database of federal employees for third-party cost analysis are criticized by privacy advocates, unions, and consumer groups who question the potential privacy exposure.
Technology
A Harvard-developed blood test that costs as little as $25 can detect nearly every virus to which a person has been exposed, potentially allowing epidemiologists to track diseases and to determine optimal vaccination ages.
Other
East Texas Medical Center sues Blue Cross, Aetna, and Cigna for excluding the hospital from their PPO networks in what it says is a violation of Texas insurance code.
I’m not surprised by Will Weider’s tweet. What we think patients want, as often is the case, isn’t what they really want. It’s smug paternalism to presume either way without actually asking them or letting their actions speak for themselves.
Clint Eastwood will direct a movie version of US Air pilot Sully Sullenberger’s biography, most likely dramatizing the “Miracle on the Hudson” story of his saving his own life (and in doing so, the lives of his passengers) rather than his later, less-dramatic safety efforts.
A Washington Post article says hospitals struggle to meet unrealistic consumer expectations as they try to manage their social media reputations, with patients rating doctors and nurses on bedside manner and convenience while providers are focused instead on delivering clinical outcomes. It mentions HealthLoop’s tailored follow-up messages and responses that help doctors know when to intervene after an encounter, citing an unnamed hospital whose satisfaction scores jumped 11 percent after implementing HealthLoop.
BIDMC CIO John Halamka, MD says the Meaningful Use program should be shut down and replaced with outcomes-based CMS incentives, with ONC refocusing its work to create a national provider messaging directory, encourage the use of a voluntary national patient identifier, work to streamline state-specific privacy laws, coordinate federal health IT priorities, and support private sector initiatives. He says interoperability demands have changed in a value-based care world and that the private sector is best equipped to meet market needs, urging that the industry “help providers do their job and improve satisfaction to the point that Congress no longer wants to legislate the solution to the problem.”
Several high-profile health IT bloggers who are patients of One Medical Group call out the supposedly tech-savvy concierge medicine company on Twitter for not providing online bill payments and for being unable to give patients digital copies of their records.
British Medical Journal reorganizes its software development teams as it moves from publisher to a vendor of point-of-care clinical guidance.
An anesthesiologist says it’s not just OR personnel who are distracted by screwing around with their phones instead of doing their jobs. He provides a first-hand example of a teen struck by a car and awaiting surgery who was taking selfies from his hospital bed while one parent was texting and the other was posting to Facebook, all of them scolding the anesthesiologist for interrupting them as he tried to take a pre-op history. He urges health professionals to educate the public about addiction to texting and social media.
Sponsor Updates
- Patientco CFO Kurt Lovell is recognized by the Atlanta Business Chronicle as a CFO of the Year finalist.
- Anthelio’s Engage mobile patient engagement app earns ONC’s 2014 Edition Modular Certification.
- Impact Advisors is named to Crain’s Chicago “Fast 50 List” as the #21 fastest-growing Chicago company.
- Healthloop is featured in an Economist article titled “Small data from patients at home will mean big cost savings.”
- Nordic profiles practice director and cheese carver Joey Vosters, who says he’ll carve the company’s logo for the next work party if Nordic will get him a 45-pound block of cheese.
- Patientkeeper offers “About Nurses, Patience, and EHRs.”
- Iatric Systems announces successful integration of Welch Allyn and Nihon Kohden medical devices with the EHR of Halifax Regional Medical Center (NC) using its Accelero Connect solution.
- MedData will exhibit at the Coastal Emergency Medicine Conference June 5-6 in Kiawah Island, SC.
- Navicure offers “Setting Goals to Improve Patient Collections and Total RCM.”
- Nordic hosts a meetup for Houston-area consultants and candidates on June 5.
- Oneview Healthcare Head of Solutions Niall O’Neill talks to NewJobRadio.
- Orion Health offers “Why you should be an engaged patient.”
- Passport Health will hold a Northeast User Group Meeting June 11-12.
- PatientSafe Solutions offers “Patient Centered Care: Is It Really That New?”
- PDS publishes “Technology and the Group Purchasing Organization Business Model.”
- Phynd Technologies offers “My Time at the More Disruption Please Hill Day.”
- New York eHealth Collaborative will exhibit at NYHIMA’s 2015 Annual Conference June 7-10 in Syracuse, NY.
- PMD posts “Purpose Build: EHR Mobile Apps vs. PMD Charge Capture.”
- Qpid Health offers “’Human-Digestible’ Documentation Tops AMIA EHR 2020 Task Force Recommendations.”
- Extension Healthcare offers “Bridging the Gap Between Clinical Users and Health Tech Managers.”
- Galen Healthcare Solutions recaps its experience at the 2015 MUSE conference.
- Beth Israel Deaconess Medical Center CIO John Halamka, MD contributes to the debut of Hayes Management Consulting’s new Healthcare Leaders series.
- HDS posts “The High Price of Health IT Security Breaches: $6B.”
- The Atlanta Journal-Constitution profiles entrepreneur Greg Foster’s battle with brain cancer while starting Brightwhistle, which was recently acquired by Influence Health.
- InstaMed publishes a new white paper entitled, “New Expectations: The Payment Experience Members Want from US Health Plans.”
- Intellect Resources offers “Healthcare IT Jobs: Carpe Diem.”
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.

Comments Off on News 6/5/15
































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…