Top News
KLAS rather histrionically reports (placing itself prominently in the story) that vendor CEOs and provider CIOS will “lock arms to make a difference” in supposedly agreeing to unstated objective measures of interoperability as John Halamka reported on his blog October 6. They will then “work closely with Washington to help alleviate the interoperability measurement burden faced by the government.” The obvious problem is that technical standards reflect capability, not reality, and the ultimate test of interoperability is best assessed by patients trying to get all of their providers working from the same basic information. It matters little that a provider’s EHR scores high on interoperability if it isn’t willing or able to share information.
Reader Comments

From Stewart Scrooged: “Re: Ministry Health Care. CEO announces that 500 employees will be RIF’d in what he calls ‘future-sizing.’ Last day for the chosen ones will be 11/28/15. Merry Christmas!” Unverified. Any organization that lays off employees in November or December is desperate, incompetent, or cold. The best thing about layoffs is that while companies jettison their least-valued employees, their best ones get the message and start looking elsewhere, closing the karmic loop.
From Lab Matters: “Re: Jeb Bush’s health plan overhaul. This is not a repeal and replace proposal. This tinkers on the edges of the ACA. And, not to be cynical, but wouldn’t the reduction in the barriers to entry really benefit his cousin Jonathan? He’s another phony crony wanting more giveaways to the private sector at the expense of the public good. Is the ACA perfect? Not by any means. But fix it. Stop with the ‘repeal’ madness that will go nowhere. Playing to his base by saying that is what he is doing and then NOT actually doing it is disingenuous at best. Sorry, Jonathan. Maybe you are the smart Bush people keep referring to since clearly isn’t Jeb.” Jeb Bush’s health plan says Obamacare has made a messed up health system even worse as the federal government took over one-sixth of the country’s economy, concluding that it “embodies the liberal idea that Washington needs to and can solve every problem,” hurting middle-income families in the process as premiums increase and healthcare choices decrease. Bush’s health IT proposals involve eliminating the Meaningful Use program and associated penalties and publicly releasing all raw, de-identified Medicare and Medicaid claims data. I agree with a lot of what he suggests, although I think his emphasis on innovation as a solution is probably misplaced, repealing the ACA is unlikely, and the idea that all of America (including Fortune 100 companies, medical associations, pharma, and their cadre of lobbyists) will obediently line up and scrap a system that made them rich is naive. His main focus seems to be letting the states run healthcare, which isn’t how it was done in those many countries whose citizens enjoy better and cheaper care than we do.
From Pilsner: “Re: Peer60 EHR report. It does not meet the basics to be called credible. Could you please ask for and publish the N value and demographic information?” The report did not cover EHRs in general – it specifically looked at ambulatory “organizations” that are either hospital-owned or independent. It was what Peer60 calls a “First Reaction” report that collects and publishes information quickly rather than exhaustively, which in this case involved 184 respondents, according to the company. It should be noted that Pilsner has a vested interest in Meditech and therefore in questioning the Meditech-unfriendly survey results.


From Follicular Folly: “Re: Cardinal Health. I was bidding for a health IT services contract and was required to take a hair follicle drug test through DC-based Metro Labs. The location was in a tiny hall, the office was beat up, and supplies were thrown all over the shelves as the entire staff conversed in Ethiopian. They said the hair had to be three inches long, and without warning, the manager chopped off two handfuls worth! I reported this to Cardinal Health, who asked what they could do, and I gave them some requests. They removed me from consideration because they couldn’t accommodate those requests. Now I have a chunk of hair missing and can’t get work .” The Yelp reviews for Metro Labs are mostly scathing.

From Mineopie: “Re: Catholic Health Initiatives. Recently entered into a managed services agreement with both Cerner (inpatient EHR) and Allscripts (outpatient EHR), just announced same for Deloitte AMS to manage Epic markets.” CHI announced the Cerner contract in July 2015 and an Allscripts hosting agreement in November 2014. They’ve been working for years with Deloitte, which announced earlier this year that it would turn its CHI Epic work into a service called Evergreen.
From Bilge Water: “Re: tweets. Your social media posts on Facebook and Twitter get good attention from companies. Nice!” Correction – they sometimes get the attention of twenty-something marketing assistants who are assigned the task of making companies look hipper than they really are by tweeting and Facebook posting on their carefully controlling behalf. It’s not as though any big company’s CEO has actually seen what goes out under the company’s Twitter and Facebook accounts, much less that he or she is writing it personally or retweeting it. It’s easy to forget in a Twitter-induced fog of pedantic kindred spirits that that most of the world, including a high proportion of business executives, has zero interest in what’s on Twitter because it’s just people talking to themselves hoping desperately that someone else is listening.
From Yukon Gold: “Re: Medicare Part A hold for outpatient claims due to Local Coverage Determinations needing to be updated in their system. They are targeting an October 23 turnaround, but this is exactly what hospitals worried about — the federal government NOT being ready for ICD-10. This is a big deal for anyone without large cash reserves that has a payer mix that isn’t mostly commercial.” Unverified.
HIStalk Announcements and Requests
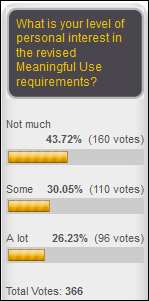
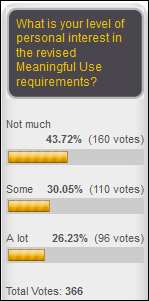
Just over half of poll respondents are interested in Meaningful Use news, while the almost-half that includes me has grown weary of the topic. New poll to your right or here: have you ever been sexually harassed at work? I’ll trust your own definition.
Thanks to Jenn for covering the last couple of posts for me. You will agree with me that she did her job well if you didn’t notice anything different.
I’ve been following the Theranos drama, happy that I had long ago already covered all of the now-hot questions about the company in previous HIStalk posts — that only one of its tests is FDA approved, that its microfluidic methods haven’t been independently validated against traditional ones and make up a minority of its tests, and that the still-small company seems secretive and has a weird but high-powered board. Here’s the thing, though – the microfluidic and nanotainer stuff makes the company sexy to Silicon Valley types and hypes its potential valuation as a technology play, but its real innovation is rock-bottom lab test pricing. Patients will get lab work done no matter how their blood is drawn even though they might prefer the Theranos-exclusive finger stick. Investors might like the company less than before, but patients should be happy that Theranos is trying to break the oligopoly of big lab companies and hospital labs whose technology allows them to process most tests for nearly no incremental cost while charging high prices. Theranos is lucky it isn’t publicly traded yet since the stock would otherwise be tanking on the barrage of criticism.

Ms. L says her Indiana kindergartners love using the two Kindle Fires we bought via the DonorsChoose project, enjoying small-group Kindle Station time every day for practicing letters, numbers, and shapes. I have a few weeks left to use the matching funds generously provided by an anonymous vendor executive for donations of $100 or more. Companies or individuals can follow these steps:
- Purchase a gift card in the amount you’d like to donate.
- Send the gift card by the email option to mr_histalk@histalk.com (that’s my DonorsChoose account).
- I’ll be notified of your donation and you can print your own receipt for tax purposes.
- I’ll pool the money, apply the matching funds, and publicly report here (as I always do) which projects I funded, with an emphasis on STEM-related projects as the matching funds donor prefers.
Here’s another DonorsChoose photo I received from Ms. Klotz, whose Illinois kindergarten class received math learning centers from us. She says the students love hands-on math work in practicing measurement, geometry, number operations.
Webinars
None in the next few days. Contact Lorre for webinar services. Past webinars are on our HIStalk webinars YouTube channel.
Acquisitions, Funding, Business, and Stock

Former HBOC Chairman Charlie McCall has been paying an army of lawyers for years in trying to have his 2009 criminal conviction for securities fraud and his 10-year prison sentence overturned. He failed again this week as the US Supreme Court rejects his argument that his legal counsel was ineffective.
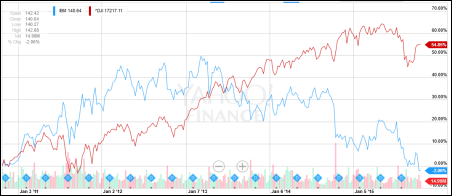
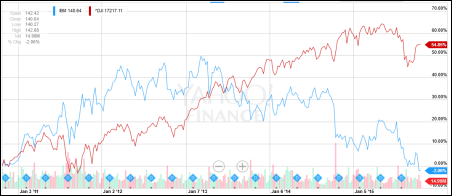
IBM announces Q3 results: revenue down 1 percent, adjusted EPS $3.34 vs. $3.68, with its sexy product lines like Watson, cloud computing, and mobile computing failing to stop the bleeding. Revenue fell for the 14th straight quarter, missing analyst expectations and sending shares down sharply on Monday. Above is the five-year share price of IBM (blue, down 2 percent) vs. the Dow (red, up 55 percent).
MMRGlobal, a self-proclaimed personal health records vendor whose business focus instead is filing patent infringement lawsuits, will conduct a one-for-five reverse stock split in hoping to strike deals with health IT firms (presumably to buy vague, dormant patents to keep their suit-filing lawyers busy). Maybe they should have gone 1,000-to-one since the OTC market shares are trading at $0.0038, valuing the company at $3 million (the price is so low that the major markets just report it as zero). Both share price and revenue are down 70 percent in the past year and cash flow is negative. Bob Lorsch owns 46 million shares, which sounds like a lot until the calculator shows their value as $175,000.
The Right Place, which connects hospitals with nursing homes for patient placement, raises $2 million.

India-based Attune, which offers a hospital information system and medical device integration, raises $10 million in Series B funding from Qualcomm Ventures and Norwest Venture Partners.

Welltok acquires children’s health gamification platform Zamzee from HopeLab, a non-profit started by eBay founder Pierre Omidyar.
Payments and EDI vendor InMediata raises $4 million
Healthcare API vendor Redox raises $3.5 million.
Sales

West Georgia Health (GA) chooses Agilum Healthcare Intelligence.

Cooper University Health Care (NJ) selects eHealth Technologies for record aggregation and analytics.
Baptist Health Care (FL) chooses Allscripts products Sunrise, Sunrise Revenue Cycle Management, EPSi, FollowMyHealth, and dbMotion, beating out Cerner and Epic. Baptist was running McKesson Horizon for inpatient and NextGen for outpatient.
Hartford HealthCare (CT) will implement Glytec’s eGlycemic Management System in its five hospitals.
People

Cynthia Kilroy (Optum) joins Huron Consulting Group as managing director.
Announcements and Implementations
In England, a doctor on trial for killing a six-year-old boy by ordering a Code Blue team to stop trying to save him after confusing him with another patient who had a DNR order admits that she also missed abnormal blood test results that were read to her over the telephone during hospital computer system downtime.
New Zealand announces plans to implement a single national EHR over the next 3-5 years.
Johns Hopkins University School of Medicine and Microsoft will work together on technology that will collect ICU monitor data to highlight big-picture trends for a given patient. They will revise Project Emerge, a Hopkins ICU redesign project that integrates ICU monitoring data via a tablet app.
Aspen Valley Hospital (CO) will implement Epic with the help of University of Colorado Health. The announcement says the implementation will give UCHealth “expanded opportunities for clinical collaboration with the goal of keeping care close to home,” which sounds a lot like using Epic to lock in referrals.
Beaumont Hospital – Farmington Hills (MI) — the former Botsford Hospital — goes live with Epic. They previously ran McKesson Paragon.
Summit Healthcare announces that four hospitals have implemented its Scripting Toolkit – Wellspan Health, Halifax Health, Nathan Littauer Hospital, and Phoebe Putney Health System. Also announced were upcoming upgrades to the product.
Qpid Health announces GA of Qpid Groupers for Epic, a subscription service of clinical content uploaded via an Epic-provided import tool.
Privacy and Security
Apple removes several hundred apps from its App Store that were found to be using technology developed by a China-based advertising company that collects user information to push targeted ads.
Other
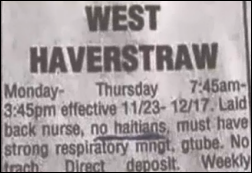
A New York healthcare staffing agency apologizes for running a nurse employment ad in the local Pennysaver that specified, “no Haitians.”
ZDoggMD has turned out some impressive music videos, but now he’s pimped himself out as an Athenahealth spokesperson and is making commercials rather than art. His new one incorrectly blames EHR vendors rather than regulators and bill-payers for the computer work he and his peers are required to perform as a condition of being well compensated, which is like complaining that TurboTax is terrible because it involves paying taxes. He also fails to mention that the employer of those providers (or they themselves) purchased those EHRs voluntarily. Given the functionality requirements of the typical hospital or practice, an innovatively designed new product would look quite a bit like the old ones, excessive clicks and all. We’re the only profession in which the highest-paid workers are expected to peck on computers all day – you would dump your attorney or accountant in a heartbeat if they wasted their expensive time typing while you’re talking. You may also correctly assume that the top-ranking executives of health systems and health IT vendors rarely sit at a keyboard despite their evangelism of the idea for everybody but themselves.
A KLAS interoperability study of minimally described methodology finds that Athenahealth’s EHR is easiest to connect to, followed by Cerner and Epic. That conclusion is pretty much negated by the admission by both vendors and providers that the technology isn’t the problem with lack of interoperability – it’s lack of agreement on standards and the willingness to actually share information.
More drug pricing nonsense and unintended consequences: Congress requires FDA to issue “priority review vouchers” as a reward to companies that develop a drug for underfunded diseases.The vouchers guarantee that FDA will review their next drug in six months instead of its usual 10 months. Drug companies are selling their FDA-issued vouchers on the secondary market, with AbbVie recently buying one from another drug company for $350 million just to cut the FDA’s bureaucratic review time by four months. You can bet that whatever drug they’re developing will be expensive if getting it on the market a few weeks earlier is worth that kind of money.
A study finds the obvious – large health systems are buying up physician practices and then jacking up their prices in using their consumer brand recognition clout to force insurance companies to pay more. What’s unknown is whether those notoriously inefficient health systems will fare better than they did in the 1990s, when they bought a lot of practices only to be shocked by the resulting drop-off in physician productivity.
Weird News Andy says, “I’m not dead yet … well …” in describing a man in India who wakes up as his autopsy begins, only to die later in the ICU.
Sponsor Updates
- Direct Consulting Associates and HDS will exhibit at the Midwest 2015 Fall Technology Conference October 25-27 in Detroit.
- Divurgent and Cerner Health Conference attendees raise $2,000 for Children’s Mercy Hospital (MO).
- Caradigm posts an infographic on clinically integrated networks.
- EClinicalWorks recaps its user conference in a series of posts.
- Clinical Computer Systems posts an integration video for its Obix perinatal database system.
- Extension Healthcare will exhibit at the 2015 CALNOC Conference October 26-27 in Long Beach, CA.
- Healthwise will exhibit at the HealthTrio 2015 Users Group Conference October 26-28 in Tucson, AZ.
- Aprima will exhibit at the AAP Experience National Conference & Exhibition October 24-27 in Washington, DC.
- Aventura and Crossings Healthcare Solutions will exhibit at the 8th Annual Regional DV-NJ Chapters HIMSS Conference October 28-30 in Atlantic City, NJ.
- Bernoulli releases a new case study featuring Hospital for Special Care, “Achieving Clinical Clarity from Ventilator Overload.”
- Forward Health Group will sponsor the American Heart Association’s Heart Innovation Forum in Chicago on October 29.
- CapsuleTech will exhibit at Anesthesiology 2015 October 24-28 in San Diego.
- Impact Advisors publishes a white paper titled “Summary and Analysis of the MU Final Rule: Modifications in 2015-18 and Stage 3 Requirements.”
- Caradigm and CoverMyMeds will exhibit at the Midwest 2015 Fall Technology Conference October 25-27 in Detroit.
- CareTech Solutions launches a new video series, “Women in IT.”
- CenterX CEO Joe Reinardy will speak at the 2015 Real-Time Benefit Verification & ePrior Authorization Forum October 22-23 in San Francisco.
- CitiusTech will exhibit at IBM Insight 2015 October 25-29 in Las Vegas.
- Craneware and its client Parkview Health (OH) will present “Enterprise Pharmacy and Supply Chain Revenue Integrity’ at HFMA’s MAP Event on October 26 in Fort Lauderdale, FL.
Blog Posts
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us or send news tips online.



















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…