Mari Poledna, RN is a telehealth ICU nurse with Banner Health of Phoenix, AZ.
Tell me about yourself and what you do.
I’m a telehealth ICU nurse. I work for Banner. I have been in this position for seven years. I have 18 years of ICU experience. I monitor ICU patients throughout the Banner healthcare system, following the model and the protocols that we’ve developed throughout the years for providing bedside monitoring and services for our sickest patient populations.
What’s it like to be working on the tele-ICU side of the house after being a bedside nurse?
In my heart of hearts, I am, I think, a bedside nurse. I still do some bedside nursing to keep my skills as clinically accurate and up to date as I can. I find that the challenges for me are to keep myself focused on how I can best support the bedside nurse and the patients in their hospital stay. I’m always trying to think like the bedside nurse.
Nurses glean a lot from their familiarity with the patient and how they are behaving. Can you do that as a telehealth nurse?
I have found that at this point in my career, with having the experience I’ve had — 18 years of seeing patients with all acuity levels — that with a video camera, honestly, I can video camera, look at a patient, and within a minute in many instances, I can tell that patient’s in trouble and that patient’s not going to last very long in terms of how they’re doing and what their physiological status is.
I feel in that sense that I can definitely get a good sense of how patients are doing. I don’t have to focus on the minutiae and the tasks of getting the things done. My viewpoint is different than what they see at the bedside, but it’s sometimes a really, really important vantage point. If you’re looking at something really up close versus stepping a few feet away, you’re still looking at the object, but you may see things that you didn’t see before.
A bedside nurse has to worry about the minutiae. They have to worry about the tasks, managing their time, other patients that they’re responsible for. Sometimes you’re just so busy and the patients are so much more ill now than they were when I started in ICU 18 years ago. Half the patients I see now in ICU would probably be dead, in all honesty. They’re very, very sick. So yes, I can look at a patient and a lot of times be able to see there’s going to be a big problem here.
The bedside nursing model seems to fluctuate every few years, with nurses first doing only clinical tasks at the top of their license, but then being made responsible for everything down to emptying patient room trash cans and sweeping floors. Now that you’re isolated from those non-clinical tasks and can concentrate purely on the intellectual activity of being a nurse, does it seem that the model is wrong?
I still do some bedside. I am emptying my trash and I’m doing certain things that other non-licensed people could do. Once again, it’s a budgetary focus, and a lot of times, the things that get cut are the things that they figure, hey, nursing can do that. We’ll just have nursing do that.
The trickle-down effect is that they’re not having the time to sit and look through trends, values, and labs. I can do that. If I see a patient and I’m worried about them, I can spend as much time as I want, 15 or 20 minutes, and look through the chart, look through results, and pull up strips. I have time to come up with a picture and a situation.
When I’m at the bedside, a lot of times I’m in this frantic mode of doing. I’m doing, I’m doing, I’m doing. Sometimes I have to stop myself and go, wait a minute, let’s think for a minute. What’s going on with this patient? What do I need to focus on right now?
I think I have a distinct advantage in that I’m still doing both versus some of the folks that I’ve worked with who are only doing the telemedicine side of it. I can see how you become more out of touch with that bedside experience. You become a little more out of touch of what they’re trying to do and what their challenges are. I like being in touch. I want to be able to be that person who can say, I know what it’s like at the bedside — I still do it.
Tell me what your day looks like.
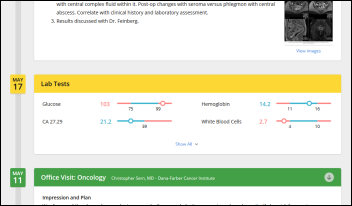
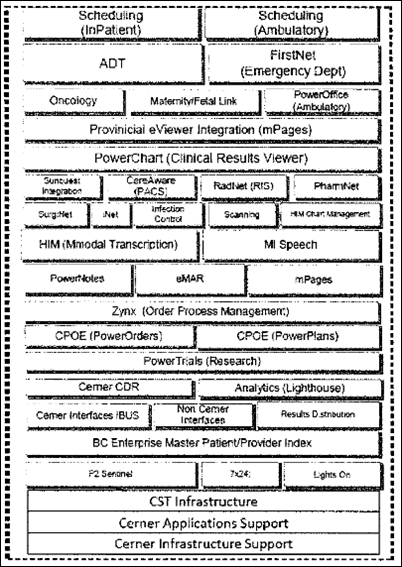
My day will start with getting an assignment of approximately 45 patients in five to seven facilities throughout the United States. I’ll come in and I’ll pull up all my technology, which is Philips monitors at the bedside. I pull up the electronic medical record that the nurses have at the bedside. Then I pull up three different applications that help me monitor the patients. One is just alarms and vital signs. If anyone’s vitals — heart rate, blood pressure, oxygenation — goes out of range, I get a notification for that. I have one screen that’s just a video camera that I can quickly access if I want to look into a patient’s room.
Then I have our version of an EMR. It’s not part of the patient’s medical record, but we use it to admit our patients and create a profile. Our electronic medical record has vital signs, trending, and basic labs. It’s a quick snapshot. If I tell a physician, "Please look at this patient," they can pull up a screen and have a quick snapshot of everything they might need to look at for that patient.
I start out by doing rounds, much like the physicians go in and do rounds. I look at the chart. I look at recent vitals, the labs for the day, I will video camera in a room and look at the room, look at the IV pumps, look at the oxygenation, look at the patient’s general condition. How do they look? Have they been stable? What are their hemodynamic drips? What are their oxygen requirements? Are they safe? Do they look comfortable? That takes maybe five minutes per patient. If I see issues, if I see holes, if I have questions, I’ll go and delve a little bit deeper into that patient’s chart. Then I move onto the next patient.
I’m doing my rounds, and as I’m doing that, new patients will be coming in the system. I have to quickly assess, how sick is this patient coming into this bed? Do I want to send the message to my doctor and say, "I’m getting a really sick patient into this facility — please take a look at this patient." Or is it a relatively stable ICU patient that I can put them in the system and just keep an eye on them? You’re looking at alarms. If I see what we call the red alarms, which are the most acute values, I might have to click into the Philips monitor and say, that oxygen says it’s 80 percent. Is that really true, or could that be the patient pulling the monitor off their finger? There’s a lot of false alarms. I’m sure you know what alarm fatigue is. That’s a big problem in these monitor units.
When I see critical situations, I have to look at that and go, do I need to look at this right now or is this a false alarm? Your whole day is rounding. It’s answering alarms and looking at patients. Sometimes the bedside will call us and ask for a second med verification, or we can actually verify blood. Our video cameras are so specific that I can zoom in and read a patient’s armband. I can zoom in and tell you where an endotracheal tube has been taped at the lip. If you have a nurse with a flashlight in the room, we can check pupils. We can look at anything in that room, even to the minutiae.
If you find something wrong or need to communicate with other ICU nurses or intensivists, what do you do?
A lot of times, if something really serious is happening at that point, if there’s someone physically in the room, a nurse, I’ll be talking to them. If not, I’ll usually ask one of my colleagues, hey, call over to this facility, tell them to go into Room 12.
Let’s say it’s a patient who’s hanging out of bed. They’re going to fall out of bed. We get a lot of that. Confused patient, they’ve just pulled out one of their lines, they’re bleeding all over the place. If it’s a nursing thing, I have someone else call the actual unit and I usually stay with the patient virtually — I talk to them. Believe it or not, they’re actually very receptive if we direct them, “Don’t put your other leg over the bed.” We tell them what to do or what not to do. “Put your oxygen back on” if they can physically do it. A lot of times they’ll actually do what we ask them to do.
If it’s something very serious where they need a physician, we have instant messaging to our physicians. I’m in Phoenix, they’re in Los Angeles, they could be in Tel Aviv, Israel. Sometimes, they’re in the same core that we’re in here in Phoenix. Sometimes I’ll just walk over and say, “Dr. Shah, can you go into this room right now?” Or we’re all up on instant message, so I can instant message them, and within seconds they will be able to turn their video camera on and go in the room and assist with whatever situation is going on.
In the Banner configuration, are you an extra layer of eyes and ears or have they taken nurses away from the bedside and moved the coverage to the tele-nurses?
No, they haven’t. They have not taken anything away from the bedside. One of Banner’s main initiatives is to become a leader in this industry of innovation and telemedicine. They’re using a lot of their resources.
We’re finding that our results are great. We’re saving money and length of stay in ICU patients. We’re bettering our morbidities and mortalities by this service. No, the nurses don’t have to do anything extra. They don’t take on extra patients or extra responsibilities. We used to refer to ourselves as a second layer of care, or second pair of eyes.
Do the bedside nurses see you as a Banner colleague who happens not to be sitting there or do they have some resentment that you’re overseeing them from afar?
Initially there was a lot more resentment, I think because the education that we provided probably wasn’t as much as it should’ve been when we would first go into a facility. What we learned was if we’re going to be providing a service, it’s really important for us to go there, spend several days, meet the staff. Really educate them, explain to them that we’re not watching what they’re doing.
We’re not looking for mistakes. We’re not micromanaging what they’re trying to do. We’re just here. If I see something that maybe for whatever reason I’m not sure if they’re aware of, or I have a concern, I approach it like, "This is something I noticed. Do you need some help? Can I get an order for you? Do you want my doctor to come in and assist you in this situation?”
Here’s a brief example. Doing my rounds one morning, I noticed an oxygen level was at 70 percent for a patient. Normal is 93 to 100. I went into the room to take a look. The respiratory therapist and nurse were in there and the patient had a tracheostomy. They were using a bag. They were bagging the patient and trying to get the oxygen levels up. They were all working very hard, but I could see that the patient was not responding. I could see the patient had had several of these episodes in the past. I said, "Just coming in to check on you guys. Can I send you my doctor? Do you need some help?" One of the nurses said, "We were thinking about calling you." I said, "No problem. Let me have my doctor come in."
When our physician went in the room, he could immediately see the patient and what was going on and see that the patient was not being able to be ventilated. He gave several medications. He paralyzed the patient, gave sedation. He spent a good amount of time to get the patient in a condition where he could be ventilated because the patient was having some heart problems with his oxygenation.
They were doing what they knew to do. They were doing the right thing, but the patient needed more. What the patient needed was an expert physician who understood how to treat this patient. We were able to prevent that patient from coding because they were going to head in the direction of a cardiac arrest. That was a great idea of how I was able to go in and say, "Can I help you?" and they said, "Sure. What can it hurt?”
They’ll think about us, but they’re in the moment, they’re treating the patient. “Oh, I better call the primary care doctor and get some orders,” but in that situation, there really wasn’t time to wait for someone to respond to a page or come in. At my workplace, we call that a save. Our physician did some extensive interventions. We were able to save that patient from deteriorating.
Do you document in the electronic health record?
We do. If we have interaction, there is a special form that’s been developed into our electronic health record. We used to be called iCare and it’s called an iCare intervention form. If I have a discussion with a nurse or I see something, then I’ll put a quick note stating what I observed and that I spoke to the nurse. It will direct me to, did I escalate it to a provider or am I just going to continue to monitor the patient?
We do put our stamp in the medical record when we do some interventions or we have conversations. We need to be able to validate how we’re contributing to the patient care. That’s an important part of our job that they’re having us focus more on. It’s like, if you’re doing things, if you’re assisting with things, make sure that you make a note. We do that.
How do you see more generalized types of video visits fitting in with in-person clinician visits?
It mirrors where we are technologically in our society. Ten years ago, I don’t think any of us thought we would be able to be on the Internet on our phones. That seemed like a strange concept. We are using a lot of our two-way video now. We project our image into a patient room so that they can see us. It’s like anything — when people are exposed to it and they get used to it, it can and I think will become more of the norm.
The only thing our ICU physicians can’t do from a remote location is, of course, lay their hands on the patient. What we’re finding is that certain procedures that used to be physician-only, now we are training advanced respiratory care practitioners to put in central lines and do certain things. There are only very few things that we would need a physician to physically do.
The technology has allowed us to have a conversation. You can physically see the physician. The video, the audio quality is great. We’re going to more and more probably see that as being the norm. Banner is expanding their telehealth programs to tele-psych, tele-wound care, behavioral health, tele-OB. You’ll probably see what Banner is doing with the telemedicine program on the horizon.
Comments Off on HIStalk Interviews Mari Poledna, Telehealth ICU Nurse, Banner Health


































































The $50 billion Rural Health payout is welcome. In context, it's less than the total cost of the F22 raptor…