News 11/4/15
Top News
Pamplona Capital Management will acquire MedAssets for $2.7 billion, announcing plans to divest the company’s group purchasing and performance improvement segments to VHA-UHC and merge its revenue cycle business with another of Pamplona’s recent acquisitions, Precyse. Pamplona says the new, privately company will be a national leader in outsourced revenue cycle, technology, and education, explaining:
Existing and prospective customers of the new, realigned company should expect a business that is dedicated to investing in integrating our technology both internally and with EMR software providers; improving the visualization and utility of our data; scaling our front, middle, and back-end services businesses; and, developing offerings in patient payments and value-based reimbursement. MedAssets and Precyse employees will be part of a growing, focused business that prioritizes long-term value creation
Pamplona will pay a 30 percent premium for shares of MedAssets. MedAssets said this summer that it was exploring strategic alternatives even as an activist investor called for it to replace some of its board members due to questionable acquisitions and undervalued shares. It also lost a key customer and and announced plans to lay off 5 percent of its workforce just a few weeks ago.
Pamplona acquired Precyse in July 2015 for an undisclosed price from Altaris Capital Partners and NewSpring Capital.
HIStalk Announcements and Requests
Want to connect with me on LinkedIn? I’m here, as is Dann’s 3,649-member HIStalk Fan Club.
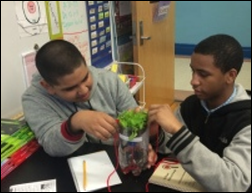
Mr. Graham in Illinois sent photos of his students using the STEM materials we provided, saying, “The students have shown a great interest in science. They enjoy working with these activities and do the research that goes along with them. They have learned more from these kits than I would have ever been able to teach them using our science textbooks. It is very rewarding for me to see how much they enjoy science now and how engaged they are with these activities. We would like to thank you for supporting our grant and putting these awesome materials into our classroom.”
HIT Geek donated $100 for my DonorsChoose project, which with double matching funded $400 worth of classroom projects:
- Eight scientific calculators for Ms. Tyler’s Algebra 2 class in La Mesa, CA.
- Green screen broadcasting equipment for Mr. Ventura’s classes in Omaha, NE to allow students to produce morning news broadcasts and video projects.
- A field trip to the Wildlife Science center for Ms. B’s Grade 6-8 class of emotionally disabled students in Brooklyn Park, MN.
HIT Geek likes reading about my funding choices. For others who would like to donate, here’s how to do it:
- Purchase a gift card in the amount you’d like to donate.
- Send the gift card by the email option to mr_histalk@histalk.com (that’s my DonorsChoose account).
- I’ll be notified of your donation and you can print your own receipt for tax purposes.
- I’ll pool the money, apply the matching funds, and publicly report here (as I always do) which projects I funded, with an emphasis on STEM-related projects.
Webinars
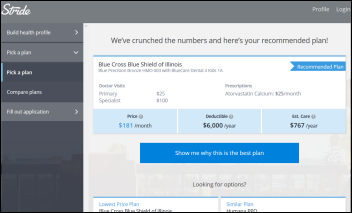
November 11 (Wednesday) 2:00 ET. “Trouble Upstream: The Underinsured and Cash Flow Challenges.” Sponsored by TransUnion. Presenter: Jonathan Wiik, principal consultant, TransUnion Healthcare. The average person spends nearly $15,000 per year on healthcare as deductibles keep rising. Providers must educate their patients on plan costs and benefits while controlling their own collection costs by using estimation tools, propensity-to-pay analytics, and point-of-sale collections. This webinar will highlight industry trends in managing underinsured patients and will describe ways to match patients to appropriate funding.
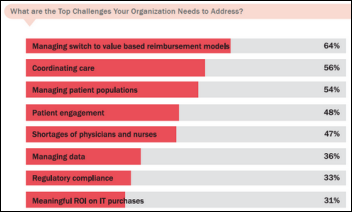
November 12 (Thursday) 1 :00 ET. “Top Predictions for Population Health Management in 2016 and Beyond.” Sponsored by Medecision. Presenters: Tobias C. Samo, MD, FACP, FHIMSS, CMIO, Medecision; Laura Kanov, BS, RRT, MBA, SVP of care delivery organization solutions, Medecision. With all the noise and hype around population health management, the presenters will share their predictions for 2016 and their insight into meeting the mounting pressures of value-based reimbursement and the tools and technology needed to manage care delivery.
Contact Lorre for webinar services. Past webinars are on our HIStalk webinars YouTube channel.
Acquisitions, Funding, Business, and Stock

Cerner reports Q3 results: revenue up 34 percent, adjusted EPS $0.54 vs. $0.42, meeting earnings estimates but falling short on revenue expectations. The company projects Q4 revenue and earnings lower than consensus, sending shares down 9 percent in after-hours trading following the announcement.

EClinicalWorks announces the opening of a London office and the signing of its first UK customer, the 1,700-store Specsavers optical chain. ECW says it booked $100 million in international business in the past year.

Teladoc reports Q3 results: revenue up 83 percent, EPS –$0.37 vs. –$2.68, with its loss meeting expectations and its $20 million in revenue beating slightly. From the earnings call:
- The company touted future potential given its 60 percent telehealth market share in a market that’s only 1 percent penetrated.
- Subscription fees made up 85 percent of the quarter’s revenue, with the remaining $3 million coming from telehealth visits.
- The company will raise its visit fee from $40 to $45 on January 1.
- Teladoc spent $1.6 million in the quarter on its legal fight with the Texas Medical Board and expects to spend up to $750K more in Q4.
- The company emphasizes that customers get what they pay for, with some lower-priced offerings failing to deliver value.
- The company says health systems are using its product to acquire patients, while health plans are using it for population health and care management.
- Teladoc believes CMS will allow fee-for-service telehealth payments via Medicare and Medicaid.
- The company is working with health systems to design a post-discharge program.
Two co-founders and a former executive of travel and expense management system vendor Concur (sold to AP last year for $8.3 billion) join Accolade. The Plymouth Meeting, PA company offer Health Assistants who work with technology and analytics to engage with consumers to reduce utilization and costs. The company claims a 98 percent user satisfaction rate, contacting healthy members an average of five times annually and reaching out to the least-healthy ones 24 times per year.
Referral and access management technology vendor SCI Solutions acquires Clarity Health, which offers authorization and referral management services.
![]()
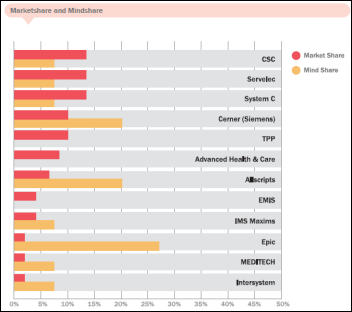
Meditech announces Q3 results: revenue down 3.5 percent, EPS $0.37 vs. $0.50 as product revenue dropped 16 percent year over year due to lower sales. Nine-month net income slid to $51 million vs. $104 million in 2014. Here’s the five-year change:
Product revenue: $60,102,900 (2010) vs. $37,004,099 (2015) – down 38 percent
Service revenue: $58,368,348 (2010) vs.$82,102,999 (2015) – up 41 percent
Total revenue: $118,471,248 (2010) vs. $119,107,098 (2015) – flat
Net income: $31,957,358 (2010) vs. $13,591,077 (2015) – down 57 percent
Earnings per share: $0.89 (2010) vs. $0.37 (2015) – down 58 percent
Shareholder equity: $408,525,252 (2010) vs. $529,738,300 (up 30 percent)
People

Best Doctors names Peter McClennen (Allscripts) as CEO.

HealthMedx founder Charlie Daniels (CS Funding) will return to the company as COO.

Sam Miller, former CIO at Massachusetts General Hospital and University Medical Center (AZ), died last month in Canada. He was 77.
A reader reports that Graham King, former president of Shared Medical Systems and McKessonHBOC’s IT business, passed away this week.
Announcements and Implementations
A two-year Geisinger study finds that patients given online access to their clinical documentation via OpenNotes have a slightly higher rate of adhering to their medication regimens. It’s an unimpressive finding, but perhaps asked the wrong question in the first place since the two observations don’t seem to have much intuitive correlation.
Wheaton Franciscan Healthcare’s southeastern Wisconsin operations will join Ascension Health, which already had 150,000 employees and 131 hospitals. Ascension pays big salaries: the CEO made $8.5 million, the CFO $4 million, the chief medical officer $2.7 million, and quite a few executives at $1.5 million and up.
In England, Addenbrooke’s Hospital is testing an online tool that allows prostate cancer patients to set PSA testing reminders and to track their own PSA levels.
A small study of outpatient diabetic patients finds that use of Glytec’s Glucommander insulin management software reduced the average A1C level from 10.4 percent to 7.4 percent within 30 days.
Middle Park Medical Center (CO) will implement Epic via Centura Health, replacing Healthland.
Government and Politics
The just-announced 2016 work plan for HHS’s Office of the Inspector General includes examining the effectiveness of the FDA’s oversight of medical device security to determine if it adequately protects patients.
The FDA seeks input on how technologies such as apps, telemedicine, and biomedical sensors might be used in performing clinical trials for drugs. FDA wants to know what technologies are being used, how FDA can encourage their use, and what challenges need to be overcome, especially regarding the use of patient-owned devices.
I’m bored with taxpayer trough-lappers biting the hand that feeds them, including the AMA, which announces that the Meaningful Use program is “doomed” unless Congress lowers the bar. It says the market needs new EHRs to support the way doctors practice, not mentioning how many of its members bought whatever a salesperson stuck in front of them in their zeal to pocket a seemingly easy $44,000 taxpayer bribe. AMA blames Meaningful Use for physician data entry time, the requirement to collect pointless information, and for creating interoperability barriers. AMA concludes that physicians embrace new technology, but are stymied by bureaucracy. I hope they are right, actually – it would be just fine with me if Meaningful Use went away.
Medicare will eliminate higher payments for medical practices acquired by hospitals starting in 2017, lowering their payments to be the same as for non-hospital owned practices and saving $9 billion per year. However, the change isn’t retroactive, so it effects only newly acquired practices, meaning hospitals may buy practices even more aggressively to lock in their high Medicare rates. The AHA is predictably lobbying against the change, saying it will reduce access to care. The change may have limited impact anyway depending on how far value-based care has progressed by the time the change kicks in.
Two senators are investigating why 12 of 23 non-profit state co-op insurers funded by $2.3 billion in ACA loans have failed. The senators also express concerns that the surviving co-ops may be using “creative accounting” that may lead to even more failures. A report from a few weeks ago found that all but one co-op is struggling financially, with some of their leaders blaming Republican-led funding cuts. Observers say the co-ops set their premiums too low and had to use their federal loans to pay medical claims.
A national human resources team sent by the VA’s national headquarters to help fix widespread problems (including extended wait times) and massive employee shortages at the Phoenix VA hospital was sent home by the hospital’s acting director, who told them that he “calls the shots.” The team says hospital management was “obstructionist” and “clearly lacked integrity.” The Phoenix VA’s HR department uses paper-based systems with no tracking capability, hampering its hiring efforts. The team observed chronic abseentism that left clueless people in charge and noted that several HR employees refused to learn new IT systems because they would then be held accountable for completing tasks.
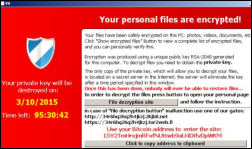
Privacy and Security
An unnamed hacker earns a $1 million prize for creating a Web-based exploit for iOS 9, which is mostly interesting because company that sponsored the challenge sells hacks non-exclusively to the highest-bidding world governments and to the NSA. An ACLU technologist referred the earlier company as a “merchant of death” that sold “the bullets for cyberwar.” The new company, Zerodium, will undoubtedly sell the hack many times for far more than $1 million to governments interested in performing electronic surveillance.
Innovation and Research
The Birmingham business paper covers Alabama Eye Bank’s self-development of a FileMaker iPad app for collecting information from cornea donors. The CIO likes that developers only need to learn one tool to deploy to both mobile and to the Web.
Technology
The Glow fertility app comes under scrutiny after the company presents data that claims women who use it to track their fertility cycles are 40 percent more likely to conceive. Researchers immediately pounced on that assertion since the analysis proved correlation but not causation. The study also didn’t control for important variables such as prior fertility treatments. An expert says the results most likely reflect selection bias rather than an app-inspired change in behavior.
Other
The Boise newspaper digs up old news from 2012 saying that the implementation of Epic at St. Luke’s caused provider productivity problems. It appears that the reporter was just playing in some legal databases and decided to throw some factoids together to create a non-story.

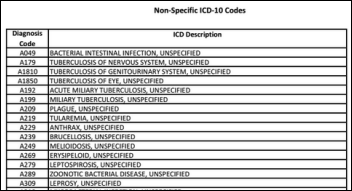
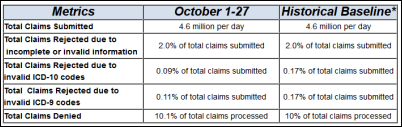
Here’s an infuriatingly stupid and insulting comment from an oncology site that also declared the ICD-10 switch to be “much ado about almost nothing.” I suppose the next time an oncology intervention saves someone from dying of cancer we should just say the tumor “blew over” instead of thanking the oncology team for saving them.
A small survey finds that people prefer receiving their lab results via a patient portal rather than by email, traditional mail, or voice mail.
In England, NHS launches its digital maturity self-assessment that trusts are required to complete. NHS England created its own assessment in which trusts will rate themselves on how well they use their systems. NHS declined to use the HIMSS EMR Adoption Model, saying it measures use only within a given organization and NHS wants to focus on interoperability.

A New York business paper delves into the expensive and not universally loved “rebranding” of North-Shore LIJ Health System to Northwell Health, chosen because it’s a neutral name that won’t limit the system as it expands. The system rejected similarly dull, feel-good names such as Laudica Health, Dedication Health, and Northstar. It will spend $20 million to roll out the new name.
Experts debate whether surgeries should be recorded on video as a “surgical black box” that could be used for learning or to defend malpractice lawsuits. Naysayers don’t like the possibility that recordings could be used to prove malpractice, would increase costs, and would expose the sometimes secretive goings-on of a typical OR.
Weirton Medical Center (WV) protests the $1.5 million an arbitrator awarded to a management company the hospital hired to turn its finances around, saying the company miscalculated payment rates and failed to prepare it to earn $1.8 million in Meaningful Use money.
Weird News Andy leans on the bar and starts his story with, “A deer walks into an ER …” An injured deer walks through the automatic doors of Strong Memorial Hospital’s ED and wanders down the corridor. Unlike other ED patients, the deer was taken out to the parking lot, where animal control officers killed it.
Sponsor Updates
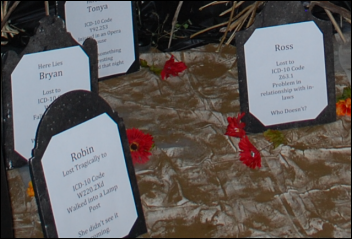
- Medicity celebrated Halloween with an ICD-10 graveyard titled “You Don’t Want to Die on This Hill.”
- Fox Business profiles AirStrip’s integration with Apple Watch and its use at Montefiore Medical Center.
- Wellcentive wins the “Emerging Company of the Year” award presented by the Metro Atlanta Chamber of Commerce.
- Aprima will exhibit at the American College of Rheumatology Annual Meeting November 8-10 in San Francisco.
- Awarepoint will exhibit at the iHT2 Health IT Summit November 3-4 in Beverly Hills, CA.
- Bernoulli will exhibit at the American Association for Respiratory Care Congress November 7-9 in Tampa, FL.
- Besler Consulting wins a 2015 Bright Bulb B2B Marketing Award for best small team in-house campaign.
- CenterX will exhibit at the NCPDP Workgroup Meeting November 4-6 in St. Louis.
- Sunquest will exhibit with GeneInsight at AMP 2015 November 5-7 in Austin, TX.
- Nordic releases a video titled “After ICD-10: Minimizing pain, increasing gain.”
- Direct Consulting Associates sponsors the HIMSS North Ohio Chapter Conference November 5 in Akron.
- Connected for Care introduces its telemedicine solution and integrate it with HealthMedx’s LTPAC EHR.
- Divurgent will exhibit at the Virginia HIMSS Fall Conference November 5-6 in Williamsburg.
- EClinicalWorks and Healthwise will exhibit at the mHealth Summit November 5-6 in National Harbor, MD.
- FormFast helps hospitals move away from paper documentation.
- The Colorado Technology Association nominates Healthgrades EVP/CIO Douglas Walton for Apex CIO of the Year.
Blog Posts
- 10 Objectives for EHR Incentive Programs (AdvancedMD)
- 33 Cyber Security Tips from the Experts (AirWatch)
- Technology to Understand the “Pop” in Population Health (Caradigm)
- Yes You Can – Put Medicare’s Chronic Care Management Billing Code to Work For You and Your Patients (CareSync)
- Lessons Learned – Allscripts PM V14 Upgrade (Culbert Healthcare Solutions)
- Enabling Your Integration – IGUANA (Galen Healthcare Solutions)
- 3 Secrets to Save on Healthcare IT Costs (Hayes Management Consulting)
- Butter knives and healthcare delivery – yes, there’s a connection! (Healthfinch)
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us or send news tips online.































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…