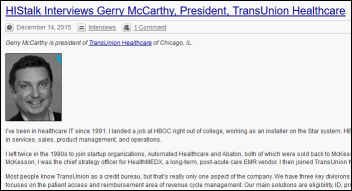
Gerry McCarthy is president of TransUnion Healthcare of Chicago, IL.

I’ve been in healthcare IT since 1991. I landed a job at HBOC right out of college, working as an installer on the Star system. HBO was eventually acquired by McKesson, where I spent the majority of my career with roles in services, sales, product management, and operations.
I left twice in the 1990s to join startup organizations, Automated Healthcare and Abaton, both of which were sold back to McKesson. McKesson has been very good to me and my family over the years. After I left McKesson, I was the chief strategy officer for HealthMEDX, a long-term, post-acute care EMR vendor. I then joined TransUnion two years ago as the president of healthcare.
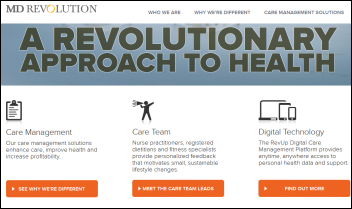
Most people know TransUnion as a credit bureau, but that’s really only one aspect of the company. We have three key divisions representing consumer, financial services, and healthcare. In healthcare, TransUnion focuses on the patient access and reimbursement area of revenue cycle management. Our main solutions are eligibility, ID, propensity to pay, charity care determination, payment plan recommendation, and insurance coverage discovery.
What kind of financial pressure are consumers feeling as the health insurance model changes?
From the Affordable Care Act, there’s been a lot of unintended consequences associated with underinsured. Now that more people have access — which is a great thing — we’re starting to see that people are struggling with being able to pay their bills and understanding what they need to pay and when. From a consumerism perspective, people struggle with how they make clinical and financial decisions based on the care that needs to be provided.
Medical bankruptcy makes up a significant percentage of personal bankruptcies. How do you see that changing over the next few years?
We see it increasing, back to that under-insured component. People think about the indigent and lower income. If you look at even the Baby Boomer generation, there was this perception that Medicare is free. All of these plans, whether it’s Medicare or these high-deductible insurance plans, are causing a significant churn within the marketplace.
Because we are TransUnion, we understand the credit bureaus. For example, the average household income is roughly $60,000. Some of these high-deductible plans are reaching $5,000 for a family. If something happens in January or February, people are immediately under water from a payment perspective against their current income.
This has been a struggle for people. We’re going to continue to see a rise in medical bankruptcy.
Not only are networks getting narrower, but some insurers have quietly eliminated out-of-network coverage completely. What will the impact be?
We see more and more movement towards consumerism in healthcare in general. It has a significant impact on our business and is an opportunity. If you look at what patients are demanding, they’re demanding not only the access to care, but they want to know what it’s going to cost before services are rendered.
Whether it’s value-based care, where there’s potentially a flat rate on a risk-based model, more and more organizations are saying, "There has to be some level of estimation and transparency up front so the patients are educated." That’s a key component of what we do.
If you look at the transparency component, what we’re seeing more and more is it’s not just the hospitals providing this information. You’re starting to see payers provide the information with both clinical and financial data to their membership so they can make the best clinical decision with the best financial outcome based on their individual plan. That’s really the goal — to get that transparency in front of the patient so they can make those decisions.
You can ask someone at the point of service what you owe and they can’t tell you – they don’t know how the encounter will be coded and everybody pays a different price based on the insurance contract. How can that transparency logjam be broken?
You’ve hit the nail on the head. You have to be able to model the actual plan information and the contract that will impact that individual. It costs more money and it’s more time-consuming to implement and do those types of solutions and services, but that’s the first piece.
The second piece is that as the patient enters the system, things change. It’s not always straightforward that this is the DRG from start to finish and this is how we’re going to code that claim. There has to be financial counseling throughout. You have to make sure that you are being transparent with that patient. As they are going through the system and the solution, financial counseling is becoming a key component of what’s happening in the care delivery model during the care as well.
Both sides want something new to happen at the point of care. The patient wants to know what they owe and the provider wants to be paid before the patient leaves. Can those interests be reconciled?
I don’t think it’s ever going to be 100 percent accurate just because of the nature of how healthcare is delivered, but based on certain procedures or certain disease states, we can get much closer. When you think about heart and ortho and standard visits are happening within the physician practice, there’s no reason why we can’t get to that level up front, where everybody can understand and ensure that you have the right patient, we’ve checked for fraud, ID, we understand the credit history of that patient, the clinical history of that patient, and we can put forth a payment plan recommendation so everybody understands that entire process all the way through.
It’s not just an eligibility check any more. It’s the ability to take all of those things into account and then also look for 501(r) charity determination. These are things that our customers in the marketplaces are talking about right now.
It’s less likely that the patient will pay once they’ve left the provider’s premises. What are providers doing to increase point-of-service collections as patient responsibility increases while also knowing that people don’t make paying medical bills a priority?
That’s key right there, to make sure that up front you’re actually providing some level of cost estimation so they clearly understand exactly what is going to happen, the care that’s going to be provided, and the potential cost associated with it.
Studies show that the patient is seven times more likely to pay the total bill on time if you receive at least $1 at the point of patient access. That whole entire step of financial counseling up front with that transparency and estimation is what drives the patient behavior.
So if a patient pays anything at all up front, they feel engaged enough to be more likely to pay the remainder?
That’s correct.
You also make a very good point that patients look at healthcare bills differently than they do everything else in their lives. Being TransUnion with our financial background and history as a company, it’s interesting to see how people pay mortgage versus cell phone versus any other prioritized account. The number one reason of whether or not people will pay their healthcare bill is if they’ve paid a bill in the past.
In the ranking of what a consumer actually will pay for, surprisingly, the cell phone ranks higher than the mortgage.
Will consumer satisfaction with providers decrease as their insurance pays less for services, leaving the patient to personally pay the provider more?
Yes. We’re starting to see for the first time within our customer base and within the market that patients are starting to shop. That does influence. They will leave a provider and go to a new provider if they’re not offering tools. For example, the ability to pay online.
The point that you’re hitting on is very valid. Patients who are dissatisfied because they’re receiving a bill that they didn’t expect to get are more likely to search out a new provider in the future for medical care.
A broader concern for me is those patients who are looking at that bill and then putting off care. It’s not even the fact that they go search for another provider. They feel that they can’t afford it, which leads us to a longer-term problem that it will be more expensive to treat that patient down the road, especially if they have some level of chronic illness.
Are some of your revenue cycle customers finding the process changing so much that they will consider selling out or, in the case of small practices, closing?
What we’re seeing right now is a trend that’s growing substantially at a 20 percent CAGR is the outsourcing of revenue cycle management services, both in physician practices as well as in the hospital setting. Many organizations are stepping back and saying, is this really core to our mission and who we are, which is truly providing the best care for the community and the health of that community? Many organizations are looking to vendors like TransUnion and others, partners of ours like Conifer and MedeAnalytics, that are growing their customer base by outsourcing their core competency of revenue cycle management.
Thinking back to the case of Accretive Health, do outsourced revenue cycle vendors have to be careful to avoid embarrassing their provider customers by using overly aggressive collections practices even as collecting the money owed becomes harder?
It is a fine line for hospitals to turn around and walk when it comes to collections. That’s why it really begins on the front end of patient access.
There’s two things that hospitals can be doing. Number one, working with your collections team at the patient access level up front and using transparency to make sure that the patient understands fully what the costs are and beginning that financial charity and propensity to pay education immediately. That’s the first step.
The second step is, before it even goes to some level of collections, we’re seeing more and more organizations … if you look at uncompensated care, one of the key components of uncompensated care is that almost 5 percent of accounts that go to bad debt have some level of insurance that neither the hospital nor the patient is aware of. Our eScan solution goes and finds all of that data and information and allows hospitals to bill that back. I was just at a hospital last week where a CFO thanked us for finding $4 million in billable claims that they were going to write off to a collection agency to go find. Our goal is to make sure that that happens before it ever becomes a collection issue where you have to involve the patient.
Will a lot of hospitals run afoul of the 501(r) charity regulations that will become a condition of their non-profit status?
We just did a seminar that you helped us put on last week. We had over 250 organizations represented on that webinar. We’ve been surprised at how much hospitals have embraced and wanted to be educated on 501(r).
We do believe that they’re extremely nervous about their tax-exempt status and making sure that they’re following up on everything to follow that law to keep that tax exempt. There’s been a couple of cases recently where hospitals had to write large checks back to counties or states or even the federal government. 501(r) is here to stay and we believe hospitals are paying attention to it.
The company offers data breach-related services. What trends are you seeing?
You can’t have a conversation with anyone in healthcare today without talking about data breach services. First and foremost, we get the first phone call when it’s almost too late, when people are calling and saying that we need to provide credit protection services that TransUnion offers to the affected population. It’s more important, obviously, to have those controls up front to manage that data and lock that down.
You’re seeing a significant spend that’s happening within healthcare being shifted away from EMR and even revenue cycle opportunities as people are investing in their data centers and their policies and controls to make sure that you do not lose access to that data.
Is is sustainable to use HIPAA to fine breached providers even when they followed reasonable standards and the type of breach they experienced could have happened to anyone?
HIPAA is actually a very solid approach, we believe, to make sure that you can maintain patients’ data rights and integrity of that information that we’re supposed to be great stewards of. When you look at, though, some of the impact of HIPAA, this information of going to — whether it’s quality indicators from a clinical perspective or getting after the right financial information — some of these are onerous and put us in a position where we know we could solve some of the problems within healthcare, but some of the regulatory components are actually holding us back from being able to do it because we can’t share and utilize the data in the way we want.
I think finding the right balance between how we manage and maintain that data for information for good versus some of the bad things that are happening out there from the hacker perspective needs to be taken into account.
How do you see the short-term future playing out?
Consumerism is going to continue to grow and influence how care is delivered and paid for. Consumers really must go through the exchanges. They’re struggling with the decision on which plan to choose with little insight as to what the plan will cost them in reality. This is similar to how hospitals are making decisions on risk-based contracting models. They’re shifting that all the way down to the patients. Payers and providers are pushing that cost out.
Patients struggle with the high-deductible plans. The reality that Medicare and ACA aren’t free is setting in. More and more we’re going to start seeing the consumerism play, where patients will want to be educated on outcomes both clinical and financial. When you look at these new “payviders,’’ when you look at health systems that are offering insurance plans, and you look at the large commercial payers, everyone’s trying to get back directly to the patient.
I think there’s going to be a huge shift towards consumerism, where we start providing more and more data and information to them from a clinical and financial perspective so they can make the decisions. Because they are the persons who are ultimately going to be responsible for their healthcare spend.
Do you have any final thoughts?
I’m very thankful for the opportunity to be with TransUnion Healthcare with its great employees and focus. We have very quietly become a leader in the RCM space. We look forward to seeing how this continues to unfold and how we can support it.














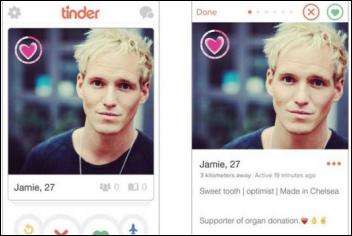





































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…