The JPMorgan Healthcare Conference and the State of Healthcare Innovation
By Marty Felsenthal

I had a lot of fun last year at this time writing about the JPMorgan Healthcare Conference. With thanks to Mr. HIStalk, I thought I’d take an opportunity to provide an update on the conference (it’s happening next week in San Francisco) and also on the state of innovation in healthcare services and healthcare software, as the two subjects are very related.
This will be my 19th consecutive year at the conference, a streak that a handful of the very coolest people might find more impressive than the Golden State Warriors’ winning streak at the beginning of the NBA season. I have been investing in venture-backed healthcare software and services companies for all of those 19 years. I’m recently and temporarily retired, but I’ve been fortunate to have generated strong returns during my career, to have worked with some great entrepreneurs, and to have worked with wonderful partners.
That said, and as I mentioned last year, until the HITECH and the Affordable Care Acts were passed, I was as relevant as Rand Paul in a Republican debate or a movie theatre showing “Star Wars” I, II, and III. Until 2010, there was certainly innovation in the provision and administration of healthcare, but it was just more limited and — relative to its potential importance to our country — not enough people cared. That all changed with the passage of those two pieces of legislation.
Once it became obvious that legislative and judicial efforts to change or repeal the Affordable Care Act would not be successful, almost overnight I underwent a combined transformation like Shia LaBeouf (Megan Fox) in “Transformers I,” Anthony Michael Hall (Kelly LeBrock) in “Weird Science,” and Will Ferrell (his first wife Leslie Bibb) in “Talladega Nights.” Life is pretty good these days for people like Steph Curry and me.
With Reform here to stay, the JPMorgan Healthcare conference became the Comic-Con of the healthcare services and software world. The conference this year will be every bit as crowded and frenetic as in recent years past. However, there are, in my opinion, two very big differences from last year.
When we’re out with friends, my loving wife of 17 years often refers to me as her "old" husband and then goes on to describe what her "new" husband is going to be like. I still haven’t figured out if she intends to leave me, kill me, or just wait for nature to take its course, but she has made it very clear he won’t snore, he won’t nap on weekends, and he’ll be better at taking advice.
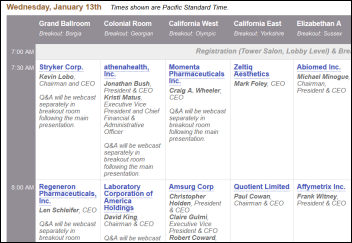
The first big difference at the conference this year is the number of "old" companies that aren’t presenting — or at least won’t be presenting in 2017 if their mergers are completed. During 2015, we have seen a tremendous amount of consolidation activity in healthcare companies attempting to reduce SG&A as a percentage of revenue through the benefits of scale; attempting to gain negotiating leverage with payers or providers (as the case may be) through horizontal consolidation; attempting to gain the benefits of vertical integration by owning more of the value chain; and attempting to diversify away from their core business into areas of the healthcare value chain that potentially have more opportunity and/or may be less regulated.
OmniCare, Rite-Aid, IPC The Hospitalist Company, United Surgical Partners, Vanguard Health, Cigna, Humana, HealthNet, Catamaran, Merge, and Gentiva are just a partial list of public companies that have announced acquisitions this past year and won’t be presenting this year (or next, depending on their merger timing). There are countless other private companies that have been acquired by United, Optum, CVS, Blue consortiums, AmSurg, Emdeon, The Advisory Board, IBM, and others.
I don’t know this for certain, but as a lifelong fan (for the past 3-4 years) and someone who one day aspires to own 0.0000001 percent of the Warriors, I’d wager my next NBA championship ring that there was more merger activity by dollar volume in healthcare services and healthcare software this year than we’ve ever experienced. This trend will absolutely continue in 2016.
The second big difference at the conference this year is the number of newly public and potentially very disruptive health care software and services companies presenting at the conference this year, all of which speak to the changing healthcare landscape.
- Evolent Health (NYSE: EVH) is presenting. The company provides technology and services to help health systems manage full or partial risk, obviously a huge opportunity in the transition to value-based care.
- Press Ganey (NYSE: PGND) is newly public and deploys its technology and services to help providers measure and manage patient satisfaction, which is increasingly being tied to reimbursement and will only get more and more important as insurance networks get more narrow.
- Inovalon (NASDAQ: INOV) is presenting and is a very interesting company that helps health plans and provider organizations collect the necessary data to get paid appropriately, and more importantly, analyze that data to measure quality and identify opportunities to improve quality.
- Teladoc (NYSE: TDOC) is also presenting (disclosure: I’m on the board of Teladoc). Teladoc is deploying its telemedicine platform across many specialties and in the payer and provider communities to address issues related to access, convenience, and cost.
- HealthEquity (NASDAQ: HQY) completed their IPO in the second half of 2014, but they also represent another newly public and innovative company helping consumers navigate the transition to high deductible health plans with better tools and engagement.
- FitBit (NYSE: FIT) isn’t presenting, but they have participated in healthcare conferences in the recent past and went public last year. I’m always a little torn about whether this is really a healthcare company, but suffice it to say the potential for inexpensive remote monitoring in healthcare using a tool like FitBit is pretty immense.
These six companies had IPOs in the past 18 months and collectively represent more than $10 billion of market value.
In my 19 years of going to the conference, I’d wager my likely nomination as the next head of HHS that this is the first-year ever that the JPMorgan Healthcare conference had six newly public and truly disruptive healthcare services and healthcare software companies presenting. That’s a very big deal for healthcare — it will lead to more great entrepreneurship and it speaks to the great market needs and opportunity being created by healthcare reform.
This brings me to the current state of innovation in healthcare software and healthcare services, with a little bit of advice for entrepreneurs and larger companies alike trying to capitalize on that innovation.
I’ve never been more optimistic or excited. Pessimists will point to the unsustainability of the exchanges (unaffordable for most in their current form without subsidies and attracting too few healthy people). They’ll say hospitals can’t manage physicians or assume risk. They’ll say that the sector is over-funded with venture and growth capital, there are too many companies being formed to do exactly the same thing, there are too many inexperienced entrepreneurs, and there are too many inexperienced investors. They’ll also point to the venture markets more broadly and the vulnerability of all the unicorns.
All fair points, but I have unbridled optimism for healthcare right now. I don’t think there has ever – ever — been a better opportunity to create more successful healthcare software and services companies, to make them bigger, and to do it faster (I sound like Oscar Goldman in “The Six Million Dollar Man”). I think the healthcare sector is undergoing the same kind of transformation that the financial services sector started in the 1970s and that continues to this day. The changes at the JPMorgan Healthcare conference I described above are a great reflection of the beginnings of that transformation and opportunity.
Healthcare is the single largest sector of the economy at almost $3 trillion. While there are certain things our healthcare system does extremely well and better than anyone else in the world, there are other aspects that are very broken. It obviously costs too much, we use way too much paper and don’t take advantage of software and automation to the extent other industries do, we still use way too much MUMPS and client-server technology, we don’t routinely use clinicians at the top of their license, our reimbursement system has historically incented volume instead of value, we aren’t as thoughtful about care at the end-of-life care as we should be, care is too fragmented and poorly coordinated, hospital systems don’t treat their best customers like a valuable asset that could walk across the street to a different system, insurers have customers paying them more than $10,000 per year year after year and do nothing to establish a personal relationship…
It’s an obvious list that could go on and on, and therein lies the opportunity. It’s so obvious. As a country with a political and economic system that responds better to change than any other place in the world, entrepreneurs have always risen to the task when markets were broken and/or a catalyst was provided. The Affordable Care Act (for all its imperfections) provided that spark. In my opinion, we’re in the top of the first inning of a game that’s going to last two to three decades.
My advice to entrepreneurs is simple. Start your company. Try to think of a unique business or clinical problem that isn’t currently being addressed. Surround yourself with experienced people who have built businesses before. Recognize that you have an opportunity cost so establish a set of metric-based milestones that represent the least you’d hope to achieve over the next six, 12, and 18 months. Stick them on your bathroom mirror, stare at them every morning, and hold yourself accountable / be honest with yourself. If you aren’t hitting them, change paths or go do something else.
Also, pick your financial partners carefully. Money is flowing loosely and freely in this environment. Personally, I think a lot of these capital sources are, in fact, a commodity (and some worse), but there are some truly value-added sources out there and I’d take their money at a discount to work with the right partner.
I’m biased towards experience so that you can diligence what you’re getting from your capital partner. I’d ask for every example they can provide of commercial contracts they introduced to (or helped facilitate for) the companies they invested in. I’d ask the same of every management team member they introduced. I’d make reference calls on them the same way they make reference calls on you and ask to talk not only to CEOs they did well with, but CEOs they fired or CEOs with whom they lost money.
Ask how they think about capital intensity and burn. Personally, I think one of the single most important areas where an investor can add or detract from value is helping to determine whether it’s time to throw fuel on the fire or to continue to let things simmer based on the market size, the competitive environment, the exit environment, and the company’s proven or unproven ability to execute.
I started my investing career at the tail end of the dot-com bubble in the late 1990s. I was fortunate to have generated returns well above the benchmarks during that environment, too. For the reasons mentioned above, I do think this time is different, but there are some valuable lessons for entrepreneurs.
First, you can raise too much money. If you raise $50 million to execute against an opportunity where your exit is only going to be $75-$100 million, you won’t do too well and your investors won’t be too happy (and ours is a small community, so you want happy investors to back you or speak well of you for whatever you do next).
Second, just because you raised all that money, please don’t feel obligated to spend it. To my point above, I think it’s very important to manage your burn and be extraordinarily disciplined about when you put fuel on the fire.
Third, every young company hits a bump (or five) in the road. The line to success is never straight. Treat everyone as respectfully and thoughtfully as possible because even though you’ve got everything figured out today, that might change tomorrow and you will still want doors to open freely and eagerly for you.
Similar to the late 1990s, we’re seeing a tremendous amount of interest from a wide variety of large companies who want to partner with young, innovative companies. This is happening in the broader economy and in healthcare specifically.
Until recently, I was a managing partner at a wonderful venture firm that included as its limited partners some of the largest for-profit and not-for-profit insurers, health systems, pharmacy chains, and healthcare foundations in the country. We also had the opportunity to interact with drug distributors, diagnostic companies, multi-sector technology firms, PBMs, and others who were equally interested in a window into healthcare innovation. There are some common characteristics of larger organizations that partnered with young and innovative companies the best.
First, they recognize that innovation is only a means to an end. There were too many large companies in the late 1990s (Time Warner AOL being the best example) and too many companies in this cycle pursuing innovation and change just because their competitors did it or just because something seemed cool and hip. The laws of nature still apply and you need a clear business objective, a product that makes sense, and a business model that makes sense.
When partnering with young companies, don’t worry about over-paying or every little contract detail. You presumably have a strong balance sheet. To a degree, small differences in price or terms at this stage don’t make a difference in the long run.
What makes a difference is whether you picked the right company. I was fortunate to have led a financing round at Teladoc early on and at the lowest valuation. However, the truth of the matter is that each investor in the subsequent three private rounds have generated outstanding returns to date as well. I led a later and more expensive round at Change Healthcare before Emdeon acquired it. In both cases, it almost didn’t matter what round you participated, just that you partnered with them.
To that point, when partnering with innovative companies, the most important thing you can do is pick the right partner, and good people obviously make good partners. Avoid entrepreneur hubris when coupled with inexperience. Treat good people well. Give them responsibility. Be flexible and responsive with them. Commit to make the partnership work. Provide transparent and timely feedback on how the partnership is working and ask for the same. If you buy or partner with a company with good people, figure out ways to make sure the good people stay and to make sure they expose the rest of the organization to what they’re working on.
There are some great examples of large companies that do innovation well. Aetna partnered successfully with lots of our portfolio companies. United / Optum have been wonderful at almost all of the points above. A number of Blue Cross Blue Shield plans have really stepped up their games in the past decade with direct investments, collaborative investments, and partnerships and acquisitions of technology companies. Walgreens and CVS have done it well with their retail clinics UPMC and The Advisory Board have done it with Evolent. Intermountain Healthcare, Geisinger ….it’s a very large and growing list and much larger than just these companies.
Some of their common themes are that innovation has senior level sponsorship and multiple sponsors. Many of these organizations have a senior-level executive (or someone reporting to a senior-level executive) whose responsibility is to act as facilitator between the executive sponsors of innovation and the folks in the lower parts of the organization who actually get things done. These organizations also make sure to incent their teams — not just on the next big acquisition or meeting projections, but on some of these softer points around innovation. Some of them provide capital for off-cycle and off-budget rapid pilots.
Much more so than HIMSS, the JPMorgan Healthcare Conference is a microcosm of our healthcare ecosystem because it covers every major and minor sector of the market, not just technology. The name of the game at the conference for the past six years (and in healthcare more broadly) is change, and every student of markets knows that big change always creates big opportunity. Healthcare is the single largest sector of the US economy and it is undergoing an unprecedented amount of change.
It’s going to be a great year for the entrepreneurs, investors, and large companies that can capitalize on it. Most important, I’m very optimistic that patients are also going to end up better off for all this change — with better and more consistent quality, with lower-cost alternatives, and with a much improved consumer experience.
Marty Felsenthal has been working with and investing in innovative healthcare software and services companies since 1992 and has led financings and/or provided growth capital to companies such as Teladoc (TDOC), Change Healthcare (acquired by Emdeon), Aperio (acquired by Danaher), PayerPath (acquired by Allscripts), Titan Health (acquired by United Surgical Partners), and USRenal Care (acquired by Leonard Green).







































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…