
William Winkenwerder, MD, MBA is chairman and founder of Winkenwerder Strategies. He was formerly president and CEO of Highmark, Inc.; assistant secretary of defense for health affairs for the United States Department of Defense; and has held leadership positions with Blue Cross Blue Shield of Massachusetts, Emory University, Prudential Healthcare, Kaiser Permanente, and the Department of Health and Human Services. He serves on the boards of health IT vendors CitiusTech, Cureatr, and Accreon.
Tell me about yourself and what you do.
I am the chairman and founder of Winkenwerder Strategies. We’re a healthcare advisory and consulting firm. I focus my efforts currently — and our firm does — on innovative healthcare companies. In that vein, I work with a number of leading private equity firms who are investing in healthcare companies, serve on the boards of these portfolio companies, and invest in these companies. In addition to that, I have a group of advisory clients in the healthcare industry.
Prior to this, I served as the CEO of Highmark Health, one of the largest health insurers in the United States. I also served as assistant secretary of defense for health affairs with responsibility for all the healthcare for the US military and the Tricare program. My background prior to that was about 20 years in the healthcare industry working in the managed care sector, both on the health plan side and the provider side.
I’m an internist by background and training, board certified. I also have a business degree from the Wharton School.
What are the biggest challenges and opportunities in healthcare IT?
There are tremendous opportunities today in the area of health information technology. Healthcare continues to pose tremendous challenges for corporate budgets, personal budgets, and our federal budget, not to mention state budgets.
We continue to spend more money each year. We thought for three of four years that the healthcare cost growth might have been tamed, but it appears that it’s taking off again this year. We are spending now over $3 trillion a year on healthcare in the United States, representing about 17-18 percent of our entire economy. What is a really amazing fact is that over the next 10 years, we will spend many trillions of dollars on healthcare, and within 10 years, we’ll be spending over $5 trillion in a single year.
There are tremendous challenges with all of that cost growth to provide healthcare and pay for healthcare in more efficient ways. I firmly believe that health information technology as an enabler of better business solutions and better care processes is critical to that task.
Where do you think we’re spending too much and getting too little return in terms of overall population health?
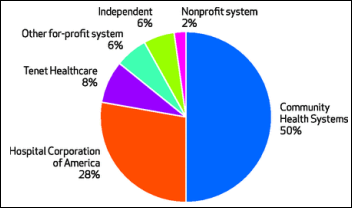
We’re spending too much inside of institutions, principally in hospitals. The hospital sector is the most single expensive sector of the entire healthcare economy. More recently, we’ve been concerned about pharmaceuticals, especially because of price increases these last two or three years, but pharmaceuticals just represent 10 or 11 percent of the entire healthcare dollar. We’re spending a lot of money in the area of long-term care in caring for people with chronic conditions.
It’s difficult to put your finger on a single sector or single area within the entire healthcare economy that is responsible for most of the problem. It really cuts across all the sectors.
We can do things so much more efficiently. But in order to accomplish that task, there have to be the right financial incentives in place and the right information, not just for clinicians and administrators in the healthcare system, but also the right information for consumers to choose and make decisions about their healthcare in order to create more of an economy for healthcare services.
Until just the past few years, there has not been, in many areas, sufficient information for people to make decisions. There has not been sufficient engagement by consumers. That’s beginning to change. People are beginning to take healthcare decisions more into their own hands, principally because they are now experiencing some of the costs directly themselves through the changes in the benefit designs, which have more high deductibles and more co-insurance and cost sharing.
The individual and the family have a vested interest in getting value for their dollars. Even though that creates some pain right now, it’s a good thing in the sense that it’s going to force more economical provision of care.
You just called out the elephant in the room. Are people realizing that their despite non-profit status and source of community pride, hospitals are looking out for their own interests as they integrate to command more market power?
There are lots of shared and conflicting interests when it comes to the local community hospital or even the regional hospital system of today. The problem is that in many markets — in fact, probably most at this point — there is just one hospital system, two, or potentially as many as three. This leaves in place a situation where there’s not sufficient competition. This is especially the case when the hospitals and doctors have come together in a community and really are just one force.
It reduces the number of choices that people have. Frankly, I think it creates a situation where there’s not sufficient room for innovation and change in the way that care can be provided. Being a physician, I think some of the most innovative models of care are through physicians driving change. I hope that, in the future, we’ve got physician-driven systems that are able to compete on equal footing with big hospital-based systems.
You worked in the Pittsburgh market, which was a bellwether for what was about to happen everywhere as providers became insurers, insurers became providers, and competition got ugly. You had UPMC as a national and even international brand. Will that also become common, where we’ll see the emergence of regional or national provider brands?
I do see the emergence of regional and national provider brands. To be clear, I don’t believe that this is all bad by any stretch. There are many great organizations that provide great care and that have developed a great brand because of their quality, their service, and their capability.
The problem comes when that entity acquires many of the resources, the assets for care within a given geographic region. Because healthcare is local, that creates a situation where there’s not choice, because people typically can’t drive hundreds of miles to receive services. It’s not like you can get your healthcare on Amazon or get the service delivered through UPS. You have to go to a local institution, a local doctor and so forth.
It’s important that regardless of who owns the assets, the rule book allows healthy competition to take place. In the absence of that, the only vehicle for control, if you will, of pricing is the government. The government typically has not been reluctant to step in to set prices or influence pricing where they can. I would expect that there will be a push to do that in other ways in other ways, pharmaceuticals, for example.
What has been the impact of the Affordable Care Act and what will it be going forward?
The Affordable Care Act has got, at best, a mixed set of results associated with it. On the positive side, we have more Americans who are insured, principally through the expansion of Medicaid, and to some extent, through the creation and operation of exchanges in most states.
The total number of additionally insured people, I think now is in the range of 16 to 18 million. Much of that is through Medicaid. I think the breakdown on that is like 10 to 12 million through Medicaid and six or seven million through exchanges. The target for the Affordable Care Act was in the range of 32 to 35 million. It’s fallen far short of the target.
At the same time, it’s introduced a lot of requirements and burdens on employers that have not made a lot of employers happy. It’s also created a bureaucratic regulatory infrastructure that I worry introduces unnecessary costs as well as a potential for limiting innovation.
On the positive side, in addition to the newly covered lives, you do have some benefits from the introduction of products on these exchanges that take advantage of things like narrow networks or higher-deductible benefit plans that do, in fact, save costs. These, ironically, are the same things that many people complain about, but they are — from an insurance perspective — the best way to limit the cost to the individual. There’s really a Catch-22 going on with some of these developments.
Certainly this is a highly political issue. It’s been that for six years now, since 2010, and it’s going to be a factor in the 2016 elections. We’ll see where all of that goes. My expectation is that there will be a continuance of certain elements of the Affordable Care Act regardless of who becomes president, but there could be a lot of change to the Affordable Care Act depending upon who gets elected.
The middle class is being hit hardest financially with higher premiums, deductibles, and co-insurance because lower-income families receive federal insurance subsidies and high-income families can afford the higher costs. One ED visit could bankrupt the average family even with insurance. What do you think the average voter wants to happen?
You have to read lots of different polls and you get different answers. People seem to want, in my reading of all of this, coverage to be available that’s affordable, on the one hand. On the other hand, they like to have choice and they would like protection against some of these high costs of healthcare.
It’s really a double bind. There’s no way to provide a really highly affordable coverage plan, for example, in a market where there’s consolidation of providers and not much insurance competition. The cost of care is just going to be expensive.
My hope is that we set the conditions and the incentives into place such that cost of care can be driven down, not just held at bay or made to grow at a slower rate of increase. There’s evidence that care can be delivered at a lower cost than it is today, many times using good technology solutions and putting information into the hands of individuals and providers.
People talk a lot about patient engagement and consumer involvement. Do consumers have more influence as customers and are providers recognizing that they must operate differently as a result?
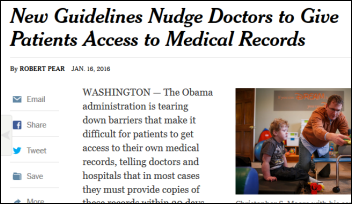
I do believe that consumes are more engaged, have more influence on their care, and want more influence on their care. They are able to get their hands, if they’re reasonably educated and interested, on information about their particular condition. That’s available on the Internet. That’s available through information sources that people can easily access. People are driving decisions at a consumer level today in ways that just weren’t happening a decade ago.
People think insurance companies are the bad guys, but what are their challenges in trying to create and manage a risk pool?
This is where CitiusTech comes into the conversation. CitiusTech is a highly innovative health information technology company solely focused on healthcare and working across all sectors, providers, health plans, life sciences, pharmaceutical, and also working even with other technology companies.
What’s needed, as you try to develop new kinds of risk- and performance-based arrangements between the payers, between the health plans and the providers, and even the pharmaceutical companies, you need really good information. You need large databases. You need to be able to integrate the data. Ideally, you’re using the capabilities of the cloud. You’re delivering great information.
That’s what I found so attractive about CitiusTech that caused me to want to work with them. We started out our relationship about a year ago in an advisory capacity and then I was asked to join their board about six months ago. They’re a great example of a new kind of company that’s totally focused on healthcare and as deep knowledge of not just the bits and the bytes of the technology, but of clinical issues, clinical information, and clinical operations. When you take that and marry it to the financial side, the health plan world, you begin to create some tremendous capabilities and the kind of capabilities that people need today.
What kind of health IT companies would get you excited about either advising them or investing in them?
CitiusTech would be one for sure. I love what they do. I’m excited with what they’re doing. I think their focus is great. It’s not just the technology, it’s the services and solutions and great talented people. That’s one example.
Another great company that I’ve had a relationship with in the past, serving as a board director, is Athenahealth. Again, a cloud-based company that is on the leading edge of change in how they do things.
There are some newer companies that are focused in specific areas. Say, for example, companies like Vitalz and ZocDoc that are focused on things like the consumer and consumer choice. They’re companies that are focused on even things like personalized genetic information. That’s going to come into the lexicon and come into people’s consciousness in terms of things they want to know about themselves that may be predictive of their future healthcare issues and needs.
There are just a lot of great companies out there. Cerner is a great company, in my opinion. They just recently won the contract to create the next-generation electronic healthcare record system for the military, partnering, by the way, with Accenture and Leidos. I served as an advisor to them in their effort to win that contract, which they did.
There’s a long list. There’s just a lot of very interesting and exciting companies out there today. Obviously, if you go to HIMSS, you’ll get to see all of them and more. It’s an interesting time.
You led the Department of Defense in building their EHR that’s now being replaced. What was your reaction to its decision and the never-ending pressure on the DoD and VA to integrate their systems?
It needed to. The system that was implemented in 2003-2004 — that’s 12-13 years ago — was an earlier-generation system. It worked, but it was really clunky. It was not sufficiently meeting the needs of the Military Health System on a global basis.
It was a big step forward at the time. It was, at the time, the largest global electronic health record system in the world. People there can be proud of what was accomplished then, but rightly in my opinion, there was a focus on creating a next-generation system utilizing the resources of a world class consulting firm like Accenture along with Cerner and along with Leidos, which was formerly SAIC and had a lot of legacy relationships and had done legacy work for the Military Health System, and so knew and understood a lot of the ground-level issues. When you put those three entities together, I think you’ve got the best-of-breed total solution.
If you were king of healthcare for a day, what would you do to fix it?
Boy. It would take more than a day [laughs]. That’s my first response.
I think of the healthcare challenge in the United States on multiple levels. One is at a political level. The politics of healthcare have to be addressed and navigated. One is at a government level. We have existing government programs in place. They need reform, including Medicare and Medicaid. Then we have a private sector system that is connected to, partly governed by, and heavily influenced by government. They are moving parts and they’re connected. Any solution or set of solutions needs to take all of that into consideration.
At the end of the day, I think that what most needs to happen is policy change at the federal government level to set the Medicare and Medicaid programs on a course of financial sustainability. They’re not sustainable right now. There are policy changes that need to be undertaken, things like extending the age of eligibility to get into Medicare, other changes with Medicare and Medicaid, etc. I won’t go into all of them, but there are important policy changes that need to happen within those federal programs.
On the private side, we have to work to create a competitive system, as I’ve alluded to earlier, where there is competition between and among providers and providers and insurers. A system in which individuals can be engaged financially themselves, but at the same time, it’s a system that people of low income and little means have support and protection. When healthcare is costing $10,000 a year per person, or for a family, $18,000 or $20,000, somebody who makes $30,000 a year literally is not going to be able to afford healthcare. We need a support system for those individuals. We just must be very careful that we don’t create something that is not sustainable. Right now, we’re on a non-sustainable track.
The politics need to take ideas from both parties and it needs to be clear-eyed in its movement forward. One of the biggest faults of the Affordable Care Act is that it did not have a single vote from one member of a party that represents half of the people. It actually had votes against it from within the Democratic party. That’s not a good thing. When you want to make big changes, you really need some level of bipartisanship. I hope, as we look at 2016 and beyond, that there will be more of that mindset applied to try to solve those problems.
I’m ever the optimist. I like to believe that America is an innovative place and we want to do right by everybody, but we need to continue to develop solutions that can provide high-quality care to most or all of the people and do that at a reasonably affordable price. That’s the goal. I believe that health information technology is central to that objective.





















































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…