Readers Write: Who’s On First? Baseball’s Lessons for Hospital Shift Scheduling
Who’s On First? Baseball’s Lessons for Hospital Shift Scheduling
By Suvas Vajracharya, PhD

A single MLB season includes over 1,200 players, 2,340 games, and 75 million fans in stadiums. In just 10 seasons, it’s possible to generate more baseball schedule options than there are atoms in the universe. Yet a full season of baseball scheduling is still far less complicated than just a single month of scheduling for 24/7 coverage shifts in a hospital emergency department. There’s good reason hospital operations teams are stressed about scheduling. Trying to do this manually with paper or a spreadsheet is an exercise in pure masochism.
First, a bit of history. Major League Baseball started out using a guy in the commissioner’s office to set up season schedules. Harry Simmons quickly found the task so overwhelming that he left the office and worked on the schedule as his full-time job (sound familiar?) In 1981, the league assigned the job to a husband-wife team named Henry and Holly Stephenson, who set the schedules for two decades using a mix of computers and manual scheduling.
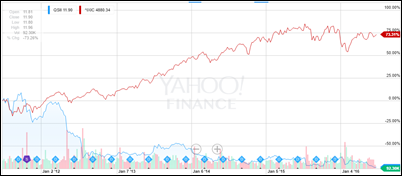
Tech leaders at IBM, MIT, Stanford, and Carnegie Mellon all tried to unseat these scheduling gurus and failed until 2005, when the league switched to what is called “combinatorial optimization” technology to generate their schedules entirely by computer.
Today, the same applied mathematics technology is used in not just Major League Baseball, but in all sports leagues, airline schedules, and retail stores, too. Any time you’ve got a mix of teams, individuals, holidays, facilities, unpredictable weather patterns, changing demand, and lots and lots of rules that sound straight out of high school word problems … that’s a scheduling job for advanced computing.
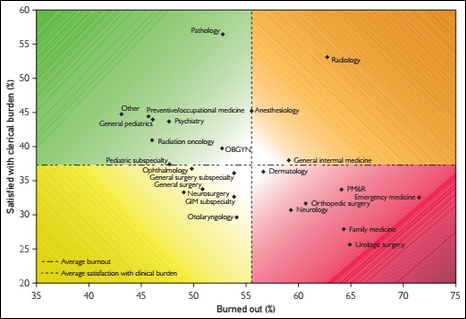
Healthcare, as anyone with experience in the sector might guess, is behind the times when it comes to scheduling technology. The vast majority of hospital departments (an estimated 80 percentage) are still setting schedules manually, like our poor old friend Harry Simmons. It’s a problem that can’t be ignored any longer. Not only is manual scheduling a major time sink for hospital operations staff, it also contributes to the already significant issues of professional burnout and physician shortages.
The MLB uses scheduling software in two distinct ways. First, they generate an established schedule for the season using set rules. These include rules designed to prevent player burnout, such as requiring a day off after a team flies west to east across the country or not playing on certain holidays. There are also operational rules, such as not having two home games in the same city the same night or making sure the weekend and weekday games are equally divided among teams.
In healthcare, these established schedule rules include things like not scheduling back-to-back night shifts for a physician, making sure weekend on-call time is fairly distributed, and ensuring key sub-specialists are available 24/7 for procedures. This rules-based schedule serves as the baseline.
After this, a second type of scheduling tool comes into play. These are requests that let the schedule flexibly adapt to changes. When a blizzard knocks out a week of MLB games or they need to cancel a series in Puerto Rico due to Zika concerns, it’s this second set of optimization technologies that reconfigures the schedule to get things back on track for the season.
In healthcare, schedule requests happen any time and all the time. Vacation, maternity, schedule swaps, requests for overtime, adding locum tenens, adding mandatory training sessions — hospital schedules change far more frequently than MLB schedules, adding to the complexity.
A recent study of over 5,500 real medical department physician shift schedules showed that medical department scheduling varies by specialty. Emergency medicine has by far the most complex process with an average of 62 repeating scheduling rules and 276 monthly schedule change requests. Hospital medicine and OB-GYN follow behind and office-based schedules such as nephrology are much simpler but still beyond anything in the MLB. The math on the number of schedules you could generate with that complexity and variability in emergency medicine is mind-boggling. That specialty also just happens to have the highest rate of physician burnout.
It is time for hospital operations leaders to figure out what the MLB discovered way back in 1981: setting complex schedules is a job for computers. Using sophisticated machine learning to balance dozens of rules and to support flexibility for ongoing changes is good practice for baseball players, pilots, and physicians. With the help of technology, hospitals might already have the solutions they’re looking for when it comes to care coordination, physician retention, increasing patient volume, and preventing staff burnout. It’s time for hospital operations to play ball.
Suvas Vajracharya, PhD is founder and CEO of Lightning Bolt Solutions of South San Francisco, CA.
































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…