EPtalk by Dr. Jayne 6/30/16

Lots of chatter in the physician lounge this week around the installation of the new president of the American Medical Association. Frankly, I haven’t heard physicians discuss the AMA this much in years. The consensus has been that the AMA doesn’t really represent physician interests. Front-line physicians think the AMA has sold them out in a variety of ways.
With that in mind, though, why is the AMA top of mind this week? It’s because new president Dr. Andrew Gurman doesn’t use an electronic health record and is proud to say so.
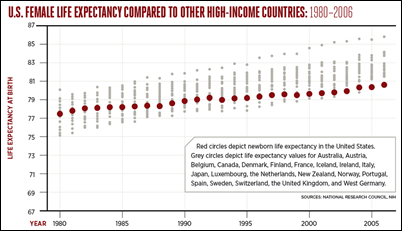
I think we’re all so subject to the EHR hype and the constant barrage of vendor messaging, that we’ve forgotten that there are a lot of physicians out there who either aren’t using EHRs or who have elected not to attest to Meaningful Use. According to CMS data, only 56 percent percent of office-based physicians had demonstrated Meaningful Use of certified EHR technology at the end of 2015. I couldn’t find all the detailed data for 2015, but looking at 2014 data, there were 17 percent of physicians who hadn’t adopted an EHR at all. Of those non-adopters, 48 percent practice either solo or in groups smaller than 10 physicians.
I’d have been a lot more impressed if the new president was a primary care physician who had opted out of EHR, but Dr. Gurman is a solo orthopedic surgeon who specializes in hand surgery. He admits his practice is just taking the 2 percent penalty at this point. If you’re just looking at a 2 percent penalty, the ROI on opting out is pretty clear, especially if Medicare isn’t responsible for the majority if your patient visits.
I don’t know what Dr. Gurman’s payer mix looks like, but the hand surgeons I know work mostly with younger patients who are likely to have commercial insurance coverage. The opt-out becomes harder as the practice’s population ages (more Medicare) or as economic forces shift (more Medicaid).
Those practices I work with that have yet to implement an EHR are generally concerned about costs. To implement an EHR well costs far more than the incentives that have been available to date, and the penalties are minor compared to the cost. Of course, when you look at the other costs that having an EHR can reduce (chart storage, supplies, staffing for inevitable “chart hunts,” inefficiency) one can make the case for an EHR. It’s when you start adding in provider time that the cost curve can start behaving unpredictably.
In an efficient practice with standardized processes and a commitment to fully support the EHR, the ROI can be tremendous. In a practice where physicians don’t have buy-in or the systems aren’t in place to make the EHR run well, the ROI can evaporate in an instant.
It’s possible to delivery high-quality, well-coordinated care without an EHR, but it’s definitely a lot of work. I’ve worked with a number of groups that have not only achieved Level 3 Patient-Centered Medical Home recognition using paper charts, but who also have been able to demonstrate higher-quality care than their peers. The reporting requirements for these initiatives can be significant and typically require using other IT systems to document outcomes even if the practice isn’t using an EHR. It’s certainly easier to use an EHR, especially if you have a robust one, but balancing the demands of the EHR with its benefits is a trick that many practices have yet to master.
I’m working with a practice right now that has only a few physicians and no dedicated resources to support their EHR. They are extremely demanding with their vendor, yet refuse to do even the simplest things to help themselves. For example, the physicians refuse to allocate time for staff to attend the complimentary webinars that their vendor offers for upgrade preparation. I suppose they think the staff will learn about the product changes through telepathy.
The managing partner refuses to work collaboratively with the EHR vendor. Today they copied me on an email to their lab vendor where they were completely out of line, making wild accusations about the EHR vendor. It doesn’t seem like they’ve ever heard the old adage about catching more flies with honey.
I’m particularly sensitive to the statistics about practices that have opted out of Meaningful Use since I’m part of one. We’re fortunate that our payer mix tips towards the commercial side, and that we’ve carefully cultivated other revenue opportunities that aren’t subject to the current regulatory environment. We provide comprehensive occupational health services for some local employers and limited services (such as pre-employment physicals and drug screens) for others. We do travel health and have some contracts for specialized medical clearance. We do use an EHR and initially participated in Meaningful Use, but stopped after it became more burdensome than it was worth.
Even though we’re robust EHR users, I wish there were better ways for us to share data with other practices. Since we provide mostly urgent care services, it would be great to be able to access patient records from primary care physicians or from other acute visits, but we really can’t get anything. We can send CCDAs like nobody’s business (and we do), but we rarely receive anything because patients generally don’t anticipate having to come in for pneumonia, bronchitis, or the flu. Our metropolitan area doesn’t have decent coverage by a health information exchange, so really the only information we can pull into the EHR is the medication history from the PBM.
The major health systems surrounding us have absolutely no desire to share information with our practice because we directly compete with their emergency departments, yet the vendors are the ones that get accused of information blocking.
Until the health systems are in some way incented to share data with the rest of us, it’s going to be hard to move forward and get the information we need to provide better care to our patients and our community. Although most hospitals have embraced EHRs, we all know how hard it is for patients to get their own records electronically. Until we start solving that problem, I don’t have a lot of hope for the hospitals sharing with anyone that’s not closely aligned with them.
We’ll have to see if there’s as much buzz around this AMA president at the end of his term as there is at the beginning. Will primary care physicians embrace him and his goals? Time will definitely tell.

Email Dr. Jayne.





























It's nice when Epic takes on patent trolls and other bad actors in the industry. They do great when they…