Travis Bond is founder and CEO of CareSync of Tampa, FL.

Tell me about yourself and the company.
I’m the founder and CEO of CareSync, which is my ninth company. My last company was Bond Technologies, which created one of the very first browser-based EMRs in the world. We had the opportunity to exit to the Eclipsys Corporation back in 2008, I believe.
I put the band back together in 2011 to create CareSync, which is a patient-centered electronic medical record that has a service on the side that basically acts as a record aggregator service. Carbon-based interfaces go out and get records and put them in a usable format that can be later searched, shared, and collaborated on. That all gave way to a business opportunity that CMS created in 2015 for chronic care management. That’s where we are today as one of the industry’s largest providers of chronic care management services under the new code.
Which is the chicken and which is the egg in offering a product that both consumers and their providers use?
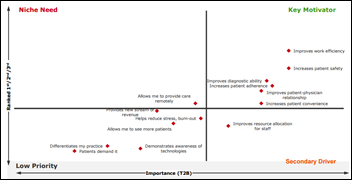
It was probably providential in some ways that we cut our teeth on a consumer product. We weren’t bound by Washington, DC regulatory requirements for a product roadmap. What’s really useful for people when they become a clinical patient is they need information and they need resources that help them to shorten the gap between what providers are saying and doing on their behalf and how they can then respond. That product, started in 2013 and known as CareSync Plus, had about a 3 percent conversion rate when we went out and advertised it to people.
It is the CMS product that now gives us the business-to-business product. We act as the vendor on behalf of the provider to offer essentially the same service. The difference — and why we still have a chicken and an egg — is that about 5,000 members a month come onto the CareSync platform as family members. Some of those family members want the same services that CCM provides under CMS for themselves. We really couldn’t sunset a legacy product when there were still people who wanted to be more of an active caregiver or wanted to be more engaged patient.
What is the scope of the CCM business?
CMS has released information only about twice on how many people and how many claims they’ve produced. At last count several months ago, about 300,000-plus have been enrolled in CCM programs since their inception in 2015. From our point of view, the geography of that number of claims is all 50 states. We have users in 30 states alone. It’s not really because we had any grand master plan, it’s that there is an alignment with many practices that want to try to care for people where they live, work, and play, not just at points or nodes of care.
I think CMS was disappointed that it did not ramp up as quickly because CMS had identified that they were going to pay $10+ billion every year for this program. Theoretically, it created a much bigger total adjustable market per year, $16 billion in 2015 and 2016. That number actually increases to a possible addressable market to $20+ billion because now they’ve given three new codes out to incentivize the market. One is an enrollment code and the other two are to address complex chronic care.
It’s not going away. It was a slow-starting process, but it’s being addressed from many different areas. The inevitability of chronic care management programs throughout healthcare has pretty much been set in stone and will just continue to grow as other new things have been introduced in healthcare over the last several decades, like HMOs and PCMHs and others. This is just another one in the fold that will continue to mature.
If I’m a physician and I think you’re a candidate to participate in CCM, what is your obligation as a patient?
It’s really quite simple. There is the consent process, which CMS wanted to know that there was written confirmation that a patient was elected to participate in something that they were eligible for. In this case, two or more chronic conditions. The chronic conditions, though, were very liberally interpreted by CMS, meaning that they were not going to actually put edits on what a provider thought was a chronically ill condition for the patient. If you look at ICD-9 alone, there are over 4,500 conditions which are marked or flagged chronic in nature.
From a patient’s perspective, it really is how you design the program. Patients need to have access to information, electronically or written, and have access to those that can access that information and are clinically trained or licensed 24/7. It’s more of an access from the vendor or the provider’s perspective. The patient, outside of them consenting to the program, just needs to make themselves available. The program is designed to give back more time and resources to where patients need it and that’s in the consumption of the treatment plans that various providers are administering to them, a reconciliation of that.
We’ve found that variability of patient engagement is as wide as any that you could imagine. Some just like to be called once a month and talked to. Others will have inbound calls and want to talk extensively about their progress. We have patients that will be a few minutes a month or it could literally be in the several hundred minutes per month. Patient requirements are still low, other than their co-insurance or co-pay responsibilities.
Otherwise, it’s intended to be a service that is aggregating information, creating a comprehensive care plan that the patient can then consume and can be collaborated and administered, and then lastly, creating a health summary that can be provided back to the patient or anyone who is seeing the patient. Overall, patient requirements are still low, but it’s incumbent on the provider to maximize the value to the patient of the program as prescribed under CMS.
How does Medicare verify or monitor that services were provided and not just billed?
In the CMS program, you bill Medicare and they pay based upon whatever edits they can run through a computer system. They don’t verify until they actually audit.
This code is really no different. They’ve said at least initially in the first couple of years that they weren’t going to put edits on their claims, meaning that they weren’t going to necessarily determine whether a chronic condition had met some criteria that Medicare would feel is not chronic enough or chronic in the right way. They’ve left that up to the physicians’ discretion.
What we’ve found is we have hundreds of chronic diseases that are on our lists for the patients who we serve. As you know, there are even several thousand rare diseases that meet the chronic definition. As it stands right now, we’ve not seen any claims denied as it relates to the diagnosis that has been tied to the CPT code 99490.
How did CareSync’s recent $20 million in new funding come about and how has it changed what you do?
We were very fortunate to have a lot of venture capitalists and strategics already having conversations with as it related back to our legacy product, CareSync Plus. Many people felt that there needed to be a connective tissue, if you will, for patients where they’re in the space that we call the dark space, which is where you are when you’re not at an appointment or a hospital setting. This dark space is like trying to navigate between airports without a radar system or air traffic control. The thesis was that surely some entity or some party would benefit if patients were better monitored and/or had the opportunities to help themselves adhere to what was prescribed.
When the code came out, it was the match that lit the fire. We were setting ourselves up with people who thought that there were problems in healthcare that could be solved with a combination of nurses and technology. Having those things in place when the code came about allowed us to execute on closing financing rounds from those players. They have since then recommitted to continuing to fund CaresSync.
We feel that the chronic care management market will continue to grow significantly, especially under the new codes in MACRA. We have 18 months of solid data that shows that providers are getting paid. We’re seeing real tangible benefits for clinical outcomes as well. Nine percent of our patients that come into the system have a severe drug-to-drug interaction that no one knew about. That’s nearly one in 10, which is pretty significant because it’s the severe drug-to-drug interactions that potentially are lethal. Sixty-four percent of our patients avoided a duplicate test because they had the results with them. A provider avoided re-prescribing another test because they felt that they had the results that they needed at the time of care.
There are many things that illustrate the advantages of the program. Those things obviously matriculate back to value when you look at an investment community. The key thing in pairing up investments from the investment community and being an entity in this space is the ability to execute at scale. We have found that it is much easier to have a chronic care management program at 30 nurses than it is 300. There are natural elements of growing and scaling that process and learning a lot of things along the way.
I think that what you’ll see overall in the market is that there will be a continued interest from the investment community in supporting this dark space and the vendors that emerge from this innovation opportunity.
Are you seeing any improvement in the ability and willingness of hospitals to provide patients with their electronic records in whatever form they request?
They’re getting a little bit better, but we’re getting a lot smarter. It’s the combination of the two that has created the net result that we are getting better, faster results from the data.
There has been an implementation of these HIT systems lag, in terms of those professionals who are running these systems even knowing that there are features to share the information. There’s still the HIPAA cloud of death and despair that hangs over all of these institutions. They feel that they need to protect this data, even from those who originated it, like the patient. That becomes primarily an education step. There’s still also a lot of medical-legal sensitivity. Why does a person want their data? Do they think we did something wrong?
That’s still a case-by-case process that we have to go through at CareSync. It’s still far easier for a provider to request information than it is a vendor. A vendor is always suspect. It is slowly changing. I wouldn’t say that we have a marked increase in the amount of freedom of information posture of these institutions that hold large amounts of it, but at least we’re seeing some incremental changes in a direction for the positive.
You were selling EHRs in the heady days. Are you glad you aren’t still in the EHR business?
Yes. [laughs] I am glad that I’m not there. In retrospect, the advent of EMRs bogged down the efficiency of a visit.
Having some medical training acted as the foundation for creating our EMR program and helped me. Technology took away from a lot of the observation skills. A good portion of medical school training is spent in diagnostics and observations of patients. Those just can’t be done simultaneously while also working through documentation requirements.
Hopefully, programs like chronic care management and other things that try to reintroduce an experience that the patient feels comfortable in talking and sharing information and how that’s captured — I’m hoping that we can blunt some of the negative impacts that EMRs had. But I would say that if I ever had to be reincarnated, I would not go back into building any piece of software for ambulatory healthcare. That was a very painful pioneering pathway to walk.
Do EHR vendors get blamed for too many clicks and too much pointless information collection instead of those parties on the back end who require collecting that information before paying providers?
Yes. I would have to side with the EMR vendors on this one. It’s not their fault. It’s Washington, DC that creates the product road maps for vendors now. It’s not what users want.
Users want a certain amount of clicking so that they can document, recall, and have that information available for the next visit or for other providers. There’s real fundamental and foundational value to EMRs. But the direction they’ve taken in terms of usability, unfortunately, was hijacked by those that were writing the checks for them in the first place. Under ARRA, the government was paying for them, but as a result of them paying for them, they were able to create what they were going to be under Meaningful Use.
There’s always a balance here. We are better off that we now have EMRs, undeniably. You’re in a far better place in being able to record this information a way that we can learn it more rapidly off the science of healthcare and treating those that have disease.
The disadvantage is that we’ve made the billing system on par with the IRS tax code. We’ve made it so complicated that it’s very difficult to do an effective visit with the necessary amount of documentation in a way that demonstrates what took place such that it could be reimbursed on par for what happened. I’m hoping that we’ll eventually get through this, but I’m worried about the overall physician dissatisfaction with their job as we go through this lonely period of transition.
Are consumers really gaining power, demanding their data, and becoming involved as participants in their own care or are we just wishfully thinking that was the case?
I think it’s slowly happening. The best chance that we have in terms of developing technologies for patients is that patients are becoming more consumer aware. That to me is probably the biggest weapon that we have. The patient is probably the greatest sleeping giant in all of healthcare. When you go through Uber or a good banking scenario or a good restaurant experience, you understand how brands compete for your business, your attention, and the right to serve you. They see that as a privilege. That’s how good businesses become great businesses.
Healthcare has had the patient lag, where they’ve been more passive and they’ve not really felt like they’re in an empowered position. I think a lot of things will start to accumulate to hit a tipping point where the patient will be more in a position of a consumer. When that light bulb goes off, the technology that they’re experiencing healthcare in needs to be more on par with other things that they experience in their lives.
The biggest advantage to the payer, the provider, and the patient is that when you look at where healthcare falls down, it doesn’t fall down in a science problem. It falls down in to an adherence and data-sharing problem. It’s not like we need better cures — we just really need to implement more effectively the ones we’ve already discovered.
Where do you see the company and the industry in the next 5-10 years?
We’ll be making more decisions in real time. Things like IBM Watson and other types of analytics that will be under the hood … we’ll see like a TurboTax for health. These things have happened, so you need to do these things.
The problem with healthcare that we’re going to finally get our hands around over the next 10 years is, how do I go do those things? If somebody tells me to get an MRI, who’s going to do that for me? Innovation is going to start to fill in this last mile of putting the things that need to get done to actually getting done and being tracked. That will start to figure its way out over the next 10 years, principally because it’s being funded against something that is challenging our economy, where 86 percent of the dollars are being spent out there to manage chronic disease. If we don’t get our hands around it, we will end up breaking both the legs of the US economy.
What will change is that vendors, payers, and providers will figure out how to play nicely with the patient who ultimately is writing a big part of the check, whether in taxes or insurance premiums. They will start to find an experience to where they’re now more engaged. Not in vendor classic term of engaged, but making them a more efficient component of the healthcare equation.
Comments Off on HIStalk Interviews Travis Bond, CEO, CareSync




























































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…