Hemant Goel, MBA is president of Spok.

Tell me about yourself and the company.
I have been in healthcare IT for over 30 years. I’ve worked for some large organizations, EMR providers, and I’ve worked for imaging solution companies as well. I joined Spok two years ago.
I’m very well conversant with all of the IT challenges for CIOs and hospitals and how it helps them. How IT has helped in patient care from "To Err is Human" to where we are now with Meaningful Use and all the advancement that has taken place in contributions of healthcare IT and helping clinicians out.
Spok is a player in healthcare IT, where we provide critical communication. Things that EMRs or other systems don’t do. This is fast paced, where minutes count in getting hold of nurses, physicians, alerts, codes, and who’s on call. Our mission is to provide critical communications in a timely basis to the right people so they can react to the situation.
Biomedical devices have evolved into IT or informatics systems. Will messaging follow that same path?
Pagers are going through a transformation as the messaging industry itself changes. Encrypted pagers are out there, two-way pagers, alpha-numeric. There has been an evolution of pagers. They have their own network. They don’t rely on the cellular networks like Verizon, AT&T, and Sprint kind of networks. They are their network with broadband and low frequency, so they are more reliable.
The change is that smart phone and the smart messaging technology are taking over, but reliability is still an issue. Oftentimes you say, I sent you my message, did you get it? They say, I didn’t see anything and the phone has been sitting right here. Those are some of the things that have to get better. When reliability improves, smart phones and smart messaging apps are the future. But pagers have a place right now.
The second thing is that for some employees – like cleaning staff or food staff — hospitals cannot give them smart phones because they are too expensive. Pagers are very convenient and suffice for them. We’re finding that there is a shift in pagers to the organization employees that are more staff. Pagers can help, they’re secure, and they maintain privacy.
There are also physicians who are not willing to give up the pagers. Just like if you go back to the imaging and PACS days, it took a long time before radiologists gave up film even though PACS systems were ready. Eventually it happened. That’s exactly what’s going to happen with pagers. Eventually the technology and reliability in messaging using smart phones and cellular coverage and Wi-Fi is going to be so much better that pagers will disappear. But I think that we are at least eight to 10 years out.
What kind of documentation of messaging activity and proof of delivery do hospitals need?
It’s a combination of both hospital and vendor-provided technologies, including carriers. One of the things we find is that hospital Wi-Fi coverage and overlap coverage is very important. It has to be there and coverage well tested.
On the technology side, I’ll give you a simple example. When I fly out of Minneapolis, there’s airport Wi-Fi that my phone picks up because I do it every day. If I don’t accept the terms and conditions, it kind of gets stuck there. When I don’t get an email after a while, I realize I did not accept terms and conditions. My phone is stuck because it’s defaulting to Wi-Fi data pickup as opposed to my cellular data pickup.
We are working with the providers and technologies to say, is it possible that if I subscribe to it in a way that says if my Wi-Fi is there but I’m not receiving data, switch to cellular and inform me that messages aren’t coming through based on some of my activities that I would expect. It’s a combination of us as vendors, infrastructure providers like cellular companies and their coverage, and of course Wi-Fi coverage inside the hospital. All three of them are advancing and they’ll get better and that will make a big difference in the reliability.
I read that cell phones are used a lot more for text messaging than for making or receiving voice calls. Does that provide any lessons learned for your business?
Millennials rely mostly on messaging and very little on voice calls. I’ve got kids who are millennials and they have WhatsApp and Facebook Messenger. I can’t tell you when they decide to use what, but they use both of them. Being curious in the IT world myself, I’m trying to figure out the pattern as to what prompts them to use which one and where.
What we have found is that for some reason, messaging applications are more utilized. Texting is more utilized. It catches attention to respond right away in the transactional moment better than if you were either to send an email or have a phone conversation. One of the reasons for the demand for messaging applications is people saying, if I have an email or task that’s important or urgent, can you also text me? They respond to that much better.
I guess there is a human factor or psychology involved, but that is indeed true. People respond to messaging and texting and they are using it more for quick, urgent transactions and not emails and phone conversations that much.
Isn’t that phenomenon a technical validation of the pager model that people dismissed as primitive? The messages are once again asynchronous and text-based, with the only real difference being that they’re now sent and received on phones instead of on two-way dedicated pagers.
Sure, but it’s the consolidation of devices that drove it. Pagers were only doing paging. You couldn’t make a phone call on them. You had to look at the pager then you had to pick up the phone. Now you can look at a pager, send a text message, and make a call to you without having to switch my devices.
The whole world of healthcare IT is about efficiency, quick access, integration, interoperability, single devices, what everyone would want. We have also found that the saturation is more than 100 percent of devices because most people now are starting to have two smart phones, professional and personal.
But you are right that at the end of the day, it’s going back. But because you can do more with your phone and more with the app and while pagers were just doing paging, the shift is there. For physicians, nurses, and emergency responders, pager reliability is still a reason to pick it up.
Is secure healthcare message a commodity? What are the differentiators?
I’ll broaden this a little bit because a lot of CIOs and CMIOs in my network have that question, too. You get secure messaging from IMessage. WhatsApp recently put up secure messaging. There are consumer applications that do secure messaging, but they don’t do it in the context of healthcare.
Now there’s a healthcare cadre of application providers that provide secure messaging, Spok being on of them. How do you differentiate yourself? The way we are approaching messaging is that messaging is one aspect of critical communication. It’s not just for physicians and nurses. Critical alerts are another one of them. The care team coordination, to help a patient get better — that’s what everyone is driving towards.
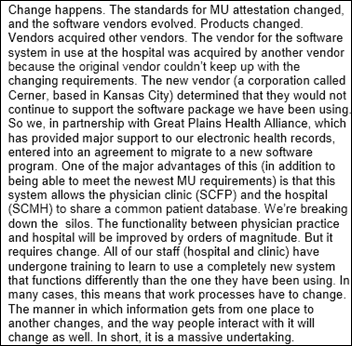
We will all eventually arrive at the same place, just like the EMR companies did. Cerner, Epic, Meditech, Allscripts, and McKesson all had their departmental solutions and eventually became a unified electronic medical record that everyone is driving towards. You hardly find any standalone pharmacy systems now. It just won’t happen with the advent of patient safety and Meaningful Use.
There are messaging companies that do messaging for physicians or for nurses. But eventually a critical communication that encompasses all stakeholders and role-players — physicians, nurses, patients themselves, family engagement like Meaningful Use talked about, the Affordable Care Act, plus other staff engagement and clinical engagement — all that should happen in a single platform with directory accessibility to drive efficiencies and clinical outcomes.
That’s what we believe and that’s what our drive is. Not just messaging for one stakeholder, but critical communication across the entire spectrum for all role-players. I believe everyone will end up there. Then, who’s got a good mousetrap?
What is the hospital demand for EHRs and other transaction systems to drive and document communication directly instead of requiring users to send messages manually?
Interoperability is going to be huge. You mentioned earlier that texting is more common than phone calls or emails. Electronic medical records initiate some things and we should be prepared as a technology to take that initiation and convert that into transactional messages that are needed.
On the flip side, sometimes our transactional messages can drive some of the things happening in the EMR, which is a system of record. We are a transaction in time that occurs. It can be driven by an EMR or we can help drive the EMR based on certain events. When there’s an emergency and there’s an ambulance coming in to the ED, nobody has the time to sit around and take a look at the EMR. You’re stabilizing the patient, you’re calling folks out, you’re calling the doctors, and codes are being initiated.
That’s where companies like Spok come in. The code message has to go to the right nurse, right physicians, and everyone has to come there. You don’t have time to sit down or the luxury to go research or pull up all the things that are happening in the system of record. That’s a clear example of how a messaging or a paging of those kinds of transactional systems can drive the EMR. Then you can go back and do your documentation into those.
Then there are situations in a hospital where you’re in the ICU or in other areas where the EMR can drive a text message to say the patient needs to be taken to radiology. Or there’s an urgent situation and you send a code out and everyone has to show up there.
You can have both sides of the equation. Interoperability is key to make sure we provide an open enough systems that those workflows are well accounted for.
What kind of hospital communications issue negatively impact patient satisfaction?
The biggest one we hear is alarm fatigue. The alarm annoyances in the quiet hospital — which is a big hospital initiative – is one of the most important areas when you’re in the acute care setting.
The second one is waiting on staff. Lots of times you’re waiting on somebody to show up. The care teams are big and there are lots of people and you are not sure who is coming to see you when. Something as simple as you’re ready to be discharged and you know you’re going to be discharged, but it takes three hours while you are waiting on someone to come in and say, "Yep, you’re good to go." That’s a problem. Many other things, but noise and wait times are the two biggest areas that we believe need to be addressed.
A quick text message that says, "You have discharged the patient, everything looks good, here is the discharge order that we can text securely” is a great way to get the patients out and get them feeling better about going home. As alarms thresholds go off or they are about to go off, it can alert the nurse and they can come and take a look at it, that’s even better. That’s a couple examples of how patient engagement and patient satisfaction are going to be hit directly by these kind of technologies.
Do you have any final thoughts?
It’s a great time to be in healthcare. The country and our healthcare system is going through a massive change. It’s always pivoting and changing, and for the better. The infrastructure of healthcare IT is in place, EMRs are in place. Now we have to take it to the next level of wellness and outcomes that are preventive healthcare and make our experience even better and better as the population gets older. I am very delighted to be in this field, have been for 30 years. I have seen a tremendous amount of changes. I’m glad to be a part of contributing to the way we treat patients and how we make lives better. It’s a good place to be.
Comments Off on HIStalk Interviews Hemant Goel, President, Spok










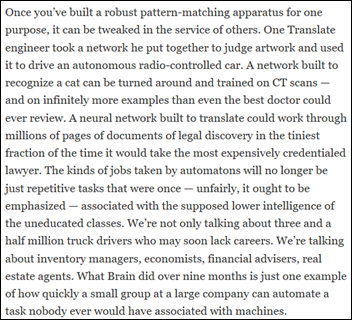












































While unsanctioned AI tools are likely causing great consternation for CIOs/CISOs, the industry has a long track record of clinical…